FDA records indicate that there are no current recalls for this drug.
Are you a medical professional?
Trending Topics
Vistide Recall
Get an alert when a recall is issued.
Questions & Answers
Side Effects & Adverse Reactions
Dose-dependent nephrotoxicity is the major dose-limiting toxicity related to VISTIDE administration. Cases of acute renal failure resulting in dialysis and/or contributing to death have occurred with as few as one or two doses of VISTIDE. Renal function (serum creatinine and urine protein) must be monitored within 48 hours prior to each dose of VISTIDE. Dose adjustment or discontinuation is required for changes in renal function (serum creatinine and/or urine protein) while on therapy. Proteinuria, as measured by urinalysis in a clinical laboratory, may be an early indicator of VISTIDE-related nephrotoxicity. Continued administration of VISTIDE may lead to additional proximal tubular cell injury, which may result in glycosuria, decreases in serum phosphate, uric acid, and bicarbonate, elevations in serum creatinine, and/or acute renal failure, in some cases, resulting in the need for dialysis. Patients with these adverse events occurring concurrently and meeting a criteria of Fanconi's syndrome have been reported. Renal function that did not return to baseline after drug discontinuation has been observed in clinical studies of VISTIDE.
Intravenous normal saline hydration and oral probenecid must accompany each VISTIDE infusion. Probenecid is known to interact with the metabolism or renal tubular excretion of many drugs (see PRECAUTIONS). The safety of VISTIDE has not been evaluated in patients receiving other known potentially nephrotoxic agents, such as intravenous aminoglycosides (e.g., tobramycin, gentamicin, and amikacin), amphotericin B, foscarnet, intravenous pentamidine, vancomycin, and non-steroidal anti-inflammatory agents (see DOSAGE AND ADMINISTRATION).
Initiation of therapy with VISTIDE is contraindicated in patients with a baseline serum creatinine > 1.5 mg/dL, a creatinine clearance ≤ 55 mL/min, or a urine protein ≥ 100 mg/dL (equivalent to ≥ 2+ proteinuria).
Neutropenia may occur during VISTIDE therapy. Neutrophil count should be monitored while receiving VISTIDE therapy.
Decreased intraocular pressure may occur during VISTIDE therapy, and in some instances has been associated with decreased visual acuity. Intraocular pressure should be monitored during VISTIDE therapy.
Decreased serum bicarbonate associated with proximal tubule injury and renal wasting syndrome (including Fanconi's syndrome) have been reported in patients receiving VISTIDE (see ADVERSE REACTIONS). Cases of metabolic acidosis in association with liver dysfunction and pancreatitis resulting in death have been reported in patients receiving VISTIDE.
Legal Issues
There is currently no legal information available for this drug.
FDA Safety Alerts
There are currently no FDA safety alerts available for this drug.
Manufacturer Warnings
There is currently no manufacturer warning information available for this drug.
FDA Labeling Changes
There are currently no FDA labeling changes available for this drug.
Uses
VISTIDE is indicated for the treatment of CMV retinitis in patients with acquired immunodeficiency syndrome (AIDS). THE SAFETY AND EFFICACY OF VISTIDE HAVE NOT BEEN ESTABLISHED FOR TREATMENT OF OTHER CMV INFECTIONS (SUCH AS PNEUMONITIS OR GASTROENTERITIS), CONGENITAL OR NEONATAL CMV DISEASE, OR CMV DISEASE IN NON-HIV-INFECTED INDIVIDUALS.
History
There is currently no drug history available for this drug.
Other Information
VISTIDE® is the brand name for cidofovir injection. The chemical name of cidofovir is 1-[(S)-3-hydroxy-2-(phosphonomethoxy)propyl]cytosine dihydrate (HPMPC), with the molecular formula of C8H14N3O6P•2H2O and a molecular weight of 315.22 (279.19 for anhydrous). The chemical structure is:

Cidofovir is a white crystalline powder with an aqueous solubility of ≥ 170 mg/mL at pH 6–8 and a log P (octanol/aqueous buffer, pH 7.1) value of -3.3.
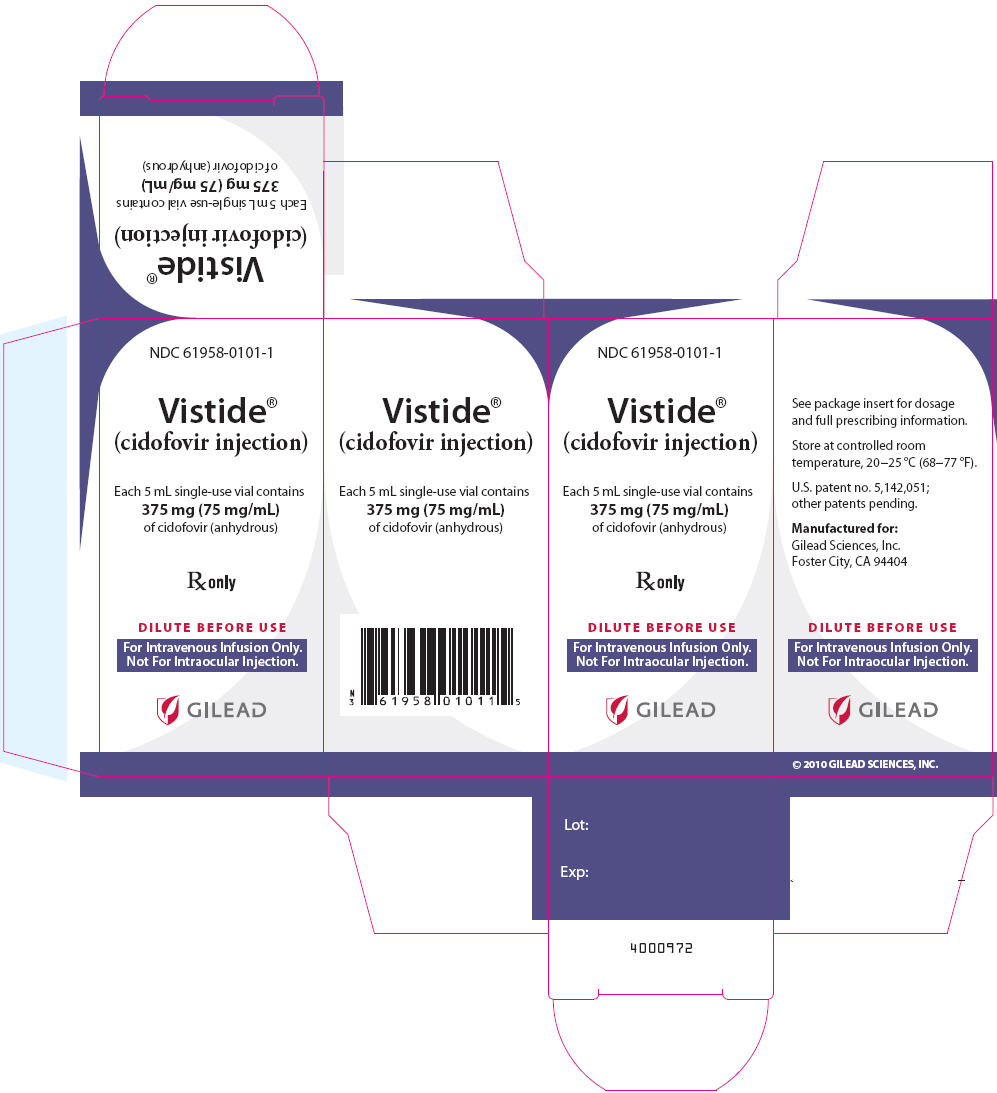
VISTIDE is a sterile, hypertonic aqueous solution for intravenous infusion only. The solution is clear and colorless. It is supplied in clear glass vials, each containing 375 mg of anhydrous cidofovir in 5 mL aqueous solution at a concentration of 75 mg/mL. The formulation is pH-adjusted to 7.4 with sodium hydroxide and/or hydrochloric acid and contains no preservatives. The appropriate volume of VISTIDE must be removed from the single-use vial and diluted prior to administration (see DOSAGE AND ADMINISTRATION).
Sources
Vistide Manufacturers
-
Gilead Sciences, Inc.
![Vistide (Cidofovir) Injection [Gilead Sciences, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Vistide | Gilead Sciences, Inc.
![Vistide (Cidofovir) Injection [Gilead Sciences, Inc.] Vistide (Cidofovir) Injection [Gilead Sciences, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
VISTIDE MUST NOT BE ADMINISTERED BY INTRAOCULAR INJECTION.
DosageTHE RECOMMENDED DOSAGE, FREQUENCY, OR INFUSION RATE MUST NOT BE EXCEEDED. VISTIDE MUST BE DILUTED IN 100 MILLILITERS 0.9% (NORMAL) SALINE PRIOR TO ADMINISTRATION. TO MINIMIZE POTENTIAL NEPHROTOXICITY, PROBENECID AND INTRAVENOUS SALINE PREHYDRATION MUST BE ADMINISTERED WITH EACH VISTIDE INFUSION.
Induction TreatmentThe recommended induction dose of VISTIDE for patients with a serum creatinine of ≤ 1.5 mg/dL, a calculated creatinine clearance > 55 mL/min, and a urine protein < 100 mg/dL (equivalent to < 2+ proteinuria) is 5 mg/kg body weight (given as an intravenous infusion at a constant rate over 1 hr) administered once weekly for two consecutive weeks. Because serum creatinine in patients with advanced AIDS and CMV retinitis may not provide a complete picture of the patient's underlying renal status, it is important to utilize the Cockcroft-Gault formula to more precisely estimate creatinine clearance (CrCl). As creatinine clearance is dependent on serum creatinine and patient weight, it is necessary to calculate clearance prior to initiation of VISTIDE. CrCl (mL/min) should be calculated according to the following formula:
Creatinine clearance for males = [140-age (years)] × [body wt (kg)]
72 × [serum creatinine (mg/dL)] Creatinine clearance for females = [140-age (years)] × [body wt (kg)] × 0.85
72 × [serum creatinine (mg/dL)] Maintenance TreatmentThe recommended maintenance dose of VISTIDE is 5 mg/kg body weight (given as an intravenous infusion at a constant rate over 1 hr), administered once every 2 weeks.
Dose Adjustment Changes in Renal Function During VISTIDE TherapyThe maintenance dose of VISTIDE must be reduced from 5 mg/kg to 3 mg/kg for an increase in serum creatinine of 0.3 – 0.4 mg/dL above baseline. VISTIDE therapy must be discontinued for an increase in serum creatinine of ≥ 0.5 mg/dL above baseline or development of ≥ 3+ proteinuria.
Preexisting Renal ImpairmentVISTIDE is contraindicated in patients with a serum creatinine concentration > 1.5 mg/dL, a calculated creatinine clearance ≤ 55 mL/min, or a urine protein ≥ 100 mg/dL (equivalent to ≥ 2+ proteinuria).
ProbenecidProbenecid must be administered orally with each VISTIDE dose. Two grams must be administered 3 hr prior to the VISTIDE dose and one gram administered at 2 and again at 8 hr after completion of the 1 hr VISTIDE infusion (for a total of 4 grams).
Ingestion of food prior to each dose of probenecid may reduce drug-related nausea and vomiting. Administration of an antiemetic may reduce the potential for nausea associated with probenecid ingestion. In patients who develop allergic or hypersensitivity symptoms to probenecid, the use of an appropriate prophylactic or therapeutic antihistamine and/or acetaminophen should be considered (see CONTRAINDICATIONS).
HydrationPatients must receive at least one liter of 0.9% (normal) saline solution intravenously with each infusion of VISTIDE. The saline solution should be infused over a 1–2 hr period immediately before the VISTIDE infusion. Patients who can tolerate the additional fluid load should receive a second liter. If administered, the second liter of saline should be initiated either at the start of the VISTIDE infusion or immediately afterwards, and infused over a 1 to 3 hr period.
Method of Preparation and AdministrationInspect vials visually for particulate matter and discoloration prior to administration. If particulate matter or discoloration is observed, the vial should not be used. With a syringe, extract the appropriate volume of VISTIDE from the vial and transfer the dose to an infusion bag containing 100 mL 0.9% (normal) saline solution. Infuse the entire volume intravenously into the patient at a constant rate over a 1 hr period. Use of a standard infusion pump for administration is recommended.
It is recommended that VISTIDE infusion admixtures be administered within 24 hr of preparation and that refrigerator or freezer storage not be used to extend this 24 hr limit.
If admixtures are not intended for immediate use, they may be stored under refrigeration (2–8°C) for no more than 24 hr. Refrigerated admixtures should be allowed to equilibrate to room temperature prior to use.
The chemical stability of VISTIDE admixtures was demonstrated in polyvinyl chloride composition and ethylene/propylene copolymer composition commercial infusion bags, and in glass bottles. No data are available to support the addition of other drugs or supplements to the cidofovir admixture for concurrent administration.
VISTIDE is supplied in single-use vials. Partially used vials should be discarded (see Handling and Disposal).
Compatibility with Ringer's solution, Lactated Ringer's solution or bacteriostatic infusion fluids has not been evaluated.
Handling and DisposalDue to the mutagenic properties of cidofovir, adequate precautions including the use of appropriate safety equipment are recommended for the preparation, administration, and disposal of VISTIDE. The National Institutes of Health presently recommends that such agents be prepared in a Class II laminar flow biological safety cabinet and that personnel preparing drugs of this class wear surgical gloves and a closed front surgical-type gown with knit cuffs. If VISTIDE contacts the skin, wash membranes and flush thoroughly with water. Excess VISTIDE and all other materials used in the admixture preparation and administration should be placed in a leak-proof, puncture-proof container. The recommended method of disposal is high temperature incineration.
Patient MonitoringSerum creatinine and urine protein must be monitored within 48 hours prior to each dose. White blood cell counts with differential should be monitored prior to each dose. In patients with proteinuria, intravenous hydration should be administered and the test repeated. Intraocular pressure, visual acuity and ocular symptoms should be monitored periodically.
Login To Your Free Account