FDA records indicate that there are no current recalls for this drug.
Are you a medical professional?
Trending Topics
Zarontin Recall
Get an alert when a recall is issued.
Questions & Answers
Side Effects & Adverse Reactions
Blood dyscrasias, including some with fatal outcome, have been reported to be associated with the use of ethosuximide; therefore, periodic blood counts should be performed. Should signs and/or symptoms of infection (e.g., sore throat, fever) develop, blood counts should be considered at that point.
Ethosuximide is capable of producing morphological and functional changes in the animal liver. In humans, abnormal liver and renal function studies have been reported. Ethosuximide should be administered with extreme caution to patients with known liver or renal disease. Periodic urinalysis and liver function studies are advised for all patients receiving the drug.
Cases of systemic lupus erythematosus have been reported with the use of ethosuximide. The physician should be alert to this possibility.
Antiepileptic drugs (AEDs), including Zarontin, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. Patients treated with any AED for any indication should be monitored for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior.
Pooled analyses of 199 placebo-controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted Relative Risk 1.8, 95% CI:1.2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence rate of suicidal behavior or ideation among 27,863 AED-treated patients was 0.43%, compared to 0.24% among 16,029 placebo-treated patients, representing an increase of approximately one case of suicidal thinking or behavior for every 530 patients treated. There were four suicides in drug-treated patients in the trials and none in placebo-treated patients, but the number is too small to allow any conclusion about drug effect on suicide.
The increased risk of suicidal thoughts or behavior with AEDs was observed as early as one week after starting drug treatment with AEDs and persisted for the duration of treatment assessed. Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed.
The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. The finding of increased risk with AEDs of varying mechanisms of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5–100 years) in the clinical trials analyzed.
Table 1 shows absolute and relative risk by indication for all evaluated AEDs.
| Indication | Placebo Patients with Events Per 1000 Patients | Drug Patients with Events Per 1000 Patients | Relative Risk: Incidence of Events in Drug Patients/Incidence in Placebo Patients | Risk Difference: Additional Drug Patients with Events Per 1000 Patients |
|---|---|---|---|---|
| Epilepsy | 1.0 | 3.4 | 3.5 | 2.4 |
| Psychiatric | 5.7 | 8.5 | 1.5 | 2.9 |
| Other | 1.0 | 1.8 | 1.9 | 0.9 |
| Total | 2.4 | 4.3 | 1.8 | 1.9 |
The relative risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
Anyone considering prescribing Zarontin or any other AED must balance the risk of suicidal thoughts and behavior with the risk of untreated illness. Epilepsy and many other illnesses for which AEDs are prescribed are themselves associated with morbidity and mortality and an increased risk of suicidal thoughts and behavior. Should suicidal thoughts and behavior emerge during treatment, the prescriber needs to consider whether the emergence of these symptoms in any given patient may be related to the illness being treated.
Patients, their caregivers, and families should be informed that AEDs increase the risk of suicidal thoughts and behavior and should be advised of the need to be alert for the emergence or worsening of the signs and symptoms of depression, any unusual changes in mood or behavior, or the emergence of suicidal thoughts, behavior, or thoughts about self-harm. Behaviors of concern should be reported immediately to healthcare providers.
Serious dermatologic reactions, including Stevens-Johnson syndrome (SJS), have been reported with ethosuximide treatment. SJS can be fatal. The onset of symptoms is usually within 28 days, but can occur later. Zarontin should be discontinued at the first sign of a rash, unless the rash is clearly not drug-related. If signs or symptoms suggest SJS, use of this drug should not be resumed and alternative therapy should be considered.
Ethosuximide crosses the placenta.
Reports suggest an association between the use of anticonvulsant drugs by women with epilepsy and an elevated incidence of birth defects in children born to these women. Data are more extensive with respect to phenytoin and phenobarbital, but these are also the most commonly prescribed anticonvulsants; less systematic or anecdotal reports suggest a possible similar association with the use of all known anticonvulsant drugs.
Cases of birth defects have been reported with ethosuximide. The reports suggesting an elevated incidence of birth defects in children of drug-treated epileptic women cannot be regarded as adequate to prove a definite cause and effect relationship. There are intrinsic methodological problems in obtaining adequate data on drug teratogenicity in humans; the possibility also exists that other factors, e.g., genetic factors or the epileptic condition itself, may be more important than drug therapy in leading to birth defects. The great majority of mothers on anticonvulsant medication deliver normal infants. It is important to note that anticonvulsant drugs should not be discontinued in patients in whom the drug is administered to prevent major seizures because of the strong possibility of precipitating status epilepticus with attendant hypoxia and threat to life. In individual cases where the severity and frequency of the seizure disorder are such that the removal of medication does not pose a serious threat to the patient, discontinuation of the drug may be considered prior to and during pregnancy, although it cannot be said with any confidence that even minor seizures do not pose some hazard to the developing embryo or fetus.
The prescribing physician will wish to weigh these considerations in treating or counseling epileptic women of childbearing potential.
Ethosuximide is excreted in human breast milk. Because the effects of ethosuximide on the nursing infant are unknown, caution should be exercised when ethosuximide is administered to a nursing mother. Ethosuximide should be used in nursing mothers only if the benefits clearly outweigh the risks.
Legal Issues
There is currently no legal information available for this drug.
FDA Safety Alerts
There are currently no FDA safety alerts available for this drug.
Manufacturer Warnings
There is currently no manufacturer warning information available for this drug.
FDA Labeling Changes
There are currently no FDA labeling changes available for this drug.
Uses
Zarontin is indicated for the control of absence (petit mal) epilepsy.
History
There is currently no drug history available for this drug.
Other Information
Zarontin (ethosuximide) is an anticonvulsant succinimide, chemically designated as alpha-ethyl-alpha-methyl-succinimide, with the following structural formula:

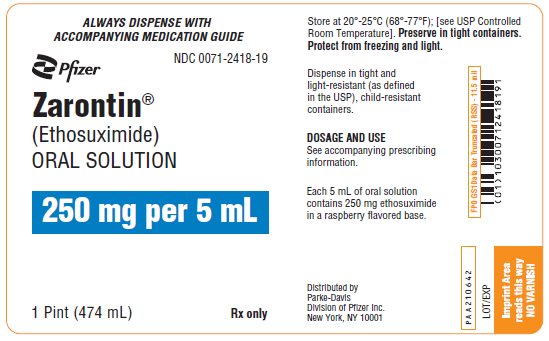
Each teaspoonful (5 mL), for oral administration, contains 250 mg ethosuximide, USP. Also contains citric acid, anhydrous, USP; FD&C red No. 40; FD&C yellow No. 6; flavor; glycerin, USP; purified water, USP; saccharin sodium, USP; sodium benzoate, NF; sodium citrate, USP; sucrose, NF.
Sources
Zarontin Manufacturers
-
Parke-davis Div Of Pfizer Inc
![Zarontin (Ethosuximide) Solution [Parke-davis Div Of Pfizer Inc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Zarontin | Parke-davis Div Of Pfizer Inc
![Zarontin (Ethosuximide) Solution [Parke-davis Div Of Pfizer Inc] Zarontin (Ethosuximide) Solution [Parke-davis Div Of Pfizer Inc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Zarontin is administered by the oral route. The initial dose for patients 3 to 6 years of age is one teaspoonful (250 mg) per day; for patients 6 years of age and older, 2 teaspoonfuls (500 mg) per day. The dose thereafter must be individualized according to the patient's response. Dosage should be increased by small increments. One useful method is to increase the daily dose by 250 mg every four to seven days until control is achieved with minimal side effects. Dosages exceeding 1.5 g daily, in divided doses, should be administered only under the strictest supervision of the physician. The optimal dose for most pediatric patients is 20 mg/kg/day. This dose has given average plasma levels within the accepted therapeutic range of 40 to 100 mcg/mL. Subsequent dose schedules can be based on effectiveness and plasma level determinations.
Zarontin may be administered in combination with other anticonvulsants when other forms of epilepsy coexist with absence (petit mal). The optimal dose for most pediatric patients is 20 mg/kg/day.
-
Parke-davis Div Of Pfizer Inc
![Zarontin (Ethosuximide) Capsule [Parke-davis Div Of Pfizer Inc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Zarontin | Parke-davis Div Of Pfizer Inc
![Zarontin (Ethosuximide) Capsule [Parke-davis Div Of Pfizer Inc] Zarontin (Ethosuximide) Capsule [Parke-davis Div Of Pfizer Inc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Zarontin is administered by the oral route. The initial dose for patients 3 to 6 years of age is one capsule (250 mg) per day; for patients 6 years of age and older, 2 capsules (500 mg) per day. The dose thereafter must be individualized according to the patient's response. Dosage should be increased by small increments. One useful method is to increase the daily dose by 250 mg every four to seven days until control is achieved with minimal side effects. Dosages exceeding 1.5 g daily, in divided doses, should be administered only under the strictest supervision of the physician. The optimal dose for most pediatric patients is 20 mg/kg/day. This dose has given average plasma levels within the accepted therapeutic range of 40 to 100 mcg/mL. Subsequent dose schedules can be based on effectiveness and plasma level determinations.
Zarontin may be administered in combination with other anticonvulsants when other forms of epilepsy coexist with absence (petit mal). The optimal dose for most pediatric patients is 20 mg/kg/day.
Login To Your Free Account


![Zarontin (Ethosuximide) Capsule [Parke-davis Div Of Pfizer Inc]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=0e008f33-70a1-4bc6-b3a0-d45214418ab6&name=zarontin-03.jpg)