FDA records indicate that there are no current recalls for this drug.
Are you a medical professional?
Trending Topics
Apple Recall
Get an alert when a recall is issued.
Questions & Answers
Side Effects & Adverse Reactions
See boxed WARNINGS at the beginning of this information sheet.
Do not administer allergenic extract injections intravenously. Patients should always be observed for at least 20 to 30 minutes after any skin test or injection. Concentrated allergenic extracts should be diluted with Sterile Diluent for Allergenic Extract prior to use for intradermal testing and for immunotherapy preparation. Systemic reactions may occur infrequently and may range from mild exaggeration of the patient’s allergic symptoms to urticaria, rhinitis, conjunctivitis, angioedema, cough, wheezing, fainting, pallor, bradycardia, hypotension, or even, in extremely sensitive individuals, to anaphylactic shock and death. Have epinephrine 1:1,000 readily available in case of a reaction. Emergency measures and personnel trained for medical emergencies should be immediately available in the event of a life-threatening reaction. Patients with unstable asthma or steroid dependent asthmatics and patients with underlying cardiovascular disease are at greater risk. Patients taking beta-blocker medication may not respond to the usual dose of epinephrine.
Diagnostic testing as well as immunotherapy should be temporarily withheld from patients or the dose reduced until cause of reaction is evaluated by prescribing physician if any of the following conditions exist: (1) severe symptoms of rhinitis and/or asthma, (2) infection or flu accompanied by fever, (3) exposure to excessive amounts of clinically relevant allergen prior to a scheduled injection, and (4) systemic reaction to previous injection.
Legal Issues
There is currently no legal information available for this drug.
FDA Safety Alerts
There are currently no FDA safety alerts available for this drug.
Manufacturer Warnings
There is currently no manufacturer warning information available for this drug.
FDA Labeling Changes
There are currently no FDA labeling changes available for this drug.
Uses
Immunotherapy using allergenic extracts is indicated for use in patients with severe allergy symptoms (hay fever, rhinitis, etc.) to pollens, molds, insects, animal danders and various other allergens. Immunotherapy is intended for patients whose symptoms are not satisfactorily controlled by avoidance of the offending allergen or by the use of symptomatic medications. Treatment uses only those specific allergens that the patient is sensitive to based on diagnostic tests and medical history. It is not intended for treatment of patients who do not manifest immediate hypersensitivity reactions to the allergenic extract following skin testing.
History
There is currently no drug history available for this drug.
Other Information
Therapeutic extracts (concentrates) are designed primarily for the physician equipped to prepare dilutions and mixtures as necessary. Allergenic Extracts are manufactured from various biological allergenic source materials including pollens, molds, epidermals, insects, food and environmental inhalants. The extraction is performed in a glycerin solution and the resulting concentration is expressed as weight to volume (w/v) ratio. This is the weight of dry pollen in grams to volume of glycerin extracting solution in milliliters. Extracts are filtered and sterile filled. Tests include those for safety and sterility. The route of administration is subcutaneous. Scratch diagnostic extracts are of the same therapeutic extract formulation and their route of administration is percutaneous. Intradermal diagnostic extracts are dilutions of the therapeutic extracts using Sterile Diluent for Allergenic Extract.
| Inactive ingredients: | ||
| Therapeutic and Scratch extracts: | Intradermal 1:500 v/v (foods) | Intradermal 1:1,000 v/v (pollens, molds, epidermals, inhalants) |
| Glycerin, USP, 50% v/v | Glycerin, USP, 0.1% v/v | Glycerin, USP, 0.05% v/v |
| Sodium chloride, USP, 0.166% w/v | Sodium chloride, USP, 0.9% w/v | Sodium chloride, USP, 0.9% w/v |
| Sodium bicarbonate, USP, 0.091% w/v | Sodium bicarbonate, USP, 0.000182% w/v | Sodium bicarbonate, USP, 0.000091% w/v |
| Phenol, USP, 0.4% w/v | Phenol, USP, 0.4% w/v | |
| Sterile Diluent for Allergenic Extract: | ||
| Normal Saline with Phenol: | Human Serum Albumin: | Glycerin, USP, 50% w/v |
| Sodium chloride, USP 0.9% w/v | Sodium chloride, USP 0.9% w/v | Sodium bicarbonate, USP 0.091% w/v |
| Phenol, USP 0.4% w/v | Phenol, USP 0.4% w/v | Sodium chloride, USP 0.166% w/v |
| Water for Injection, USP q.s. | Normal Serum Albumin (Human), 0.03% w/v | Water for Injection, USP, q.s. |
| Air replaced with Nitrogen, NF | Water for Injection, USP q.s. | |
| Air replaced with Nitrogen, NF |
The following allergenic extracts are designated and labeled “FOR DIAGNOSTIC USE ONLY”. Data to support the therapeutic use of these extracts has not been established: Coffee Cottonseed Flaxseed Housefly Mosquito
The strength of Standardized Short Ragweed and Ragweed Mix, Giant and Short extracts is described (in addition to w/v) as antigen E content. The concentration of antigen E per milliliter of the final preparation as determined by radial immunodiffusion (RID). The antigen E content of an extract is influenced by several variables. These include antigen E content of the pollen, nature of extracting solutions, ratio of pollen weight to volume of extracting solution and storage conditions. Variables which influence antigen E stability during storage conditions include nature of the solvent, antigen E concentration and storage temperature. Glycerin is a stabilizer of antigen E and other allergens.
Sources
Apple Manufacturers
-
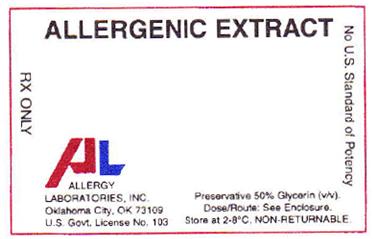
Allergy Laboratories, Inc.
![Apple Injection, Solution Apricot Injection, Solution Avocado Injection, Solution Banana Injection, Solution Blackberry Injection, Solution Blueberry (Blue Ridge Blueberry) Injection, Solution Cantaloupe Injection, Solution Cherry Food (Cherry) Injection, Solution Osage Orange Var Bois Darc Pollen (Maclura Pomifera Pollen) Injection, Solution Lake Trout (Trout) Injection, Solution Tuna Injection, Solution Turkey Food (Turkey) Injection, Solution Black Walnut Food (Black Walnut) Injection, Solution [Allergy Laboratories, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Apple | Allergy Laboratories, Inc.
![Apple Injection, Solution Apricot Injection, Solution Avocado Injection, Solution Banana Injection, Solution Blackberry Injection, Solution Blueberry (Blue Ridge Blueberry) Injection, Solution Cantaloupe Injection, Solution Cherry Food (Cherry) Injection, Solution Osage Orange Var Bois Darc Pollen (Maclura Pomifera Pollen) Injection, Solution Lake Trout (Trout) Injection, Solution Tuna Injection, Solution Turkey Food (Turkey) Injection, Solution Black Walnut Food (Black Walnut) Injection, Solution [Allergy Laboratories, Inc.] Apple Injection, Solution Apricot Injection, Solution Avocado Injection, Solution Banana Injection, Solution Blackberry Injection, Solution Blueberry (Blue Ridge Blueberry) Injection, Solution Cantaloupe Injection, Solution Cherry Food (Cherry) Injection, Solution Osage Orange Var Bois Darc Pollen (Maclura Pomifera Pollen) Injection, Solution Lake Trout (Trout) Injection, Solution Tuna Injection, Solution Turkey Food (Turkey) Injection, Solution Black Walnut Food (Black Walnut) Injection, Solution [Allergy Laboratories, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Allergenic extracts may be administered for diagnostic testing or therapeutic purposes. The dosage will depend on the particular use of the extract.
General: When used for diagnostic testing to determine a patient’s sensitivity to specific antigens and aid in the diagnosis and treatment of atopic disease, the recommended procedure is to initially perform puncture tests, then follow with intradermal tests. The number of skin tests applied at one time will depend on the particular patient and their allergic history. These tests should be performed and observed in 15 to 20 minutes. Additional tests may be applied in sequence. Perform tests on the anterolateral aspect of the upper arm on an area that permits the effective application of a tourniquet proximal to the site of the test. The skin at the site of injection should be disinfected with rubbing alcohol before testing. A positive reaction usually develops in 15 to 20 minutes. The positive response is a wheal and flare reaction that is larger than the negative control and evaluated based on the size of the reaction.
Controls: A negative control containing the same solution that the extract was prepared in should be applied to a test site in the same manner as the tests being performed. Histamine phosphate should be used as a positive control for evaluation of skin testing. Refer to manufacturers directions provided with Histamine phosphate for recommended dosage and administration.
Percutaneous testing: In general, skin is scratched, punctured or pricked just before the allergen is applied or through a drop of test allergen which is placed on the skin. There are several devices available for this technique. Refer to the device manufacturers instructions for proper use. Test areas should be no closer than 4-5 cm apart to avoid the interference of multiple reactions. Clean test areas with alcohol and air dry. Place the allergen on the volar surface of the patient’s forearm, upper arm, or back.
1. For puncture tests, apply one drop of extract to the skin. Pierce the drop of extract and skin using a sterile hypodermic needle or vaccinating needle. Maintain the needle perpendicular to the skin surface and rock the needle back and forth to produce a small hole without bleeding. Do not rotate or gouge the needle. Remove needle from skin and wipe excess extract from skin surface.
2. For scratch tests using a scarifier or needle: make a scratch 1/16 inch long on the epidermis penetrating the outer cornified area but being careful not to draw blood. Apply one drop of allergen to the scratch or puncture.
Intracutaneous (Intradermal) testing: If puncture test is negative, proceed with intradermal test. Intradermal tests should not be performed if puncture test is positive. Use a separate sterile syringe (tuberculin type equipped with a 27 gauge by 3/8 inch needle with intradermal bevel) for each antigen. To administer the test, inject 0.02 mL of allergen into the epidermis using dilutions of the concentrated extract; a 1:500 v/v dilution for foods and 1:1,000 v/v dilution for other extracts. If the test has been performed properly, the solution should raise a bleb 2 to 3 mm in diameter. If the bleb does not appear, the injection was made too deeply. To prepare intradermal testing strengths using 1:20 w/v bulk concentrates, use the following example: Add 1 mL of 1:20 w/v to 4 mL diluent to make a 1:100 v/v dilution. Add 1 mL of 1:100 v/v to 4 mL diluent to make a 1:500 v/v dilution. Add 0.5 mL of 1:100 v/v dilution to 4.5 mL diluent to make a 1:1,000 v/v dilution.
Interpretation of results: Percutaneous tests Intradermal tests 1 1+ Erythema with 5mm wheal 0 <5mm Erythema with a <5mm wheal 2+ Erythema with a 5-10mm wheal +/- 5-10mm Erythema with a 5-10mm wheal 3+ Erythema with a 10-15mm wheal 1+ 11-20mm Erythema with a 5-10mm wheal 4+ Erythema with a wheal 15mm or larger with pseudopodia 2+ 21-30mm Erythema with a 5-10mm wheal 3+ 31-40mm Erythema with a 10-15mm wheal or with pseudopodia 4+ >40mm Erythema with >15mm wheal or with pseudopodiaImmunotherapy:
(1) General: Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permit. Injections are given subcutaneously; preferably in the arm. It is advantageous to give injections in alternate arms. Use sterile precautions and a tuberculin syringe when administering each dose. Allergen immunotherapy is typically initiated with a diluted formulation of allergens prescribed by a physician for administration to a patient. Doses are gradually increased over time and ultimately reach a maintenance dose where the patient is maintained for as long as the physician or patient feels is necessary. The formulation and dosage schedule is determined by the physician and is based on diagnostic testing and patient history. Patients with very high sensitivities should be initiated with lower concentrations (higher dilutions) and may need a very relaxed progression to maintenance doses. Pre-seasonal therapy may be initiated three months before seasonal difficulty begins and brought to maintenance dose and discontinued after that season ends. Perennial therapy (recommended) brings the patient up to tolerated maintenance dose where they remain until improvement of allergic symptoms occurs. Injections may be given at intervals of 4 to 7 days with either therapy.
(2) Suggested dilution series: Concentrated Allergenic Extracts must be diluted with Sterile Diluent for Allergenic Extract before using for immunotherapy. A 1:100,000 v/v dilution of concentrate is usually satisfactory to start treatment. To prepare a 10-fold dilution series from concentrated bulk extract, the following is suggested: Add 1 mL of 1:20 w/v extract to 4 mL diluent to make a 1:100 v/v dilution. Add 0.5 mL of the 1:100 dilution to 4.5 mL of diluent to make a 1:1,000 v/v dilution. Add 0.5 mL of the 1:1,1000 dilution to 4.5 mL diluent to make a 1:10,000 v/v dilution. Add 0.5 mL of the 1:10,000 dilution to 4.5 mL of diluent to make a 1:100,000 v/v dilution. The series may be extended to 1:1,000,000 v/v by preparing one more similar dilution as a precaution for sensitive patients.
(3) Maintenance: The maintenance level is the largest dose tolerated by the patient that relieves symptoms without producing undesirable local or general reactions. After immunotherapy has been established, a maintenance dose should be given at weekly intervals. The interval between maintenance doses can be increased gradually from one week to 10 days, to 2 weeks, 3 weeks, or even 4 weeks as allergy symptoms allow. Repeat maintenance doses at a given interval three or four times to check for continued allergy symptom relief before increasing the interval further. If large local (or systemic) reactions occur at one interval, do not increase the interval. Protection is lost rapidly if the interval between doses is more than 4 weeks. It may not be possible for all patients to reach the maximum dose indicated on the suggested dosage schedule.
(4) Suggested dosage schedule: Because the degree of sensitivity varies in many individuals, the dose and interval may need adjustment and should reflect the patient’s tolerance and response. A dose should never be given until all reactions resulting from a previous dose have entirely disappeared. After a period on immunotherapy, better tolerance may permit a longer interval between injections, or a larger maintenance dose, or both.
1:100,000 v/v 1:10,000 v/v 1:1,000 v/v 1:100 v/v Dose Vol. (mL) Dose Vol. (mL) Dose Vol. (mL) Dose Vol. (mL) Maintenance 1 0.02 8 0.02 13 0.02 19 0.02 2 0.04 9 0.05 14 0.05 20 0.05 Continue 0.25 mL of 1:100 v/v weekly. 3 0.06 10 0.10 15 0.10 21 0.08 4 0.10 11 0.15 16 0.15 22 0.10 5 0.15 12 0.25 17 0.20 23 0.15 6 0.20 18 0.25 24 0.20 7 0.25 25 0.25(5) Dose adjustments: Since the individual components of the extract are those to which the patient is allergic and to which he will be exposed, typical allergic symptoms may follow shortly after the injection, particularly those experienced by the patient during exposure when the antigen from the environment plus the injected antigen exceeds the patient’s tolerance to the antigen. In such cases, decrease the size of the next scheduled dose by at least one-half of the previous dose.
(6) Administration: Use aseptic precautions when diluting and/or preparing an injection. To avoid cross-contamination, do not use the same needle to withdraw materials from multiple vials. Use a sterile tuberculin syringe (26 or 27 gauge) with a needle at least 5/8” long and graduated in 0.01 mL units to measure each dose.
Login To Your Free Account