FDA records indicate that there are no current recalls for this drug.
Are you a medical professional?
Trending Topics
Brevibloc Recall
Get an alert when a recall is issued.
Questions & Answers
Side Effects & Adverse Reactions
Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications, and this risk may persist until significant remission occurs. Suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide. There has been a long-standing concern, however, that antidepressants may have a role in inducing worsening of depression and the emergence of suicidality in certain patients during the early phases of treatment. Pooled analyses of short-term placebo-controlled trials of antidepressant drugs (SSRIs and others) showed that these drugs increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (ages 18–24) with major depressive disorder (MDD) and other psychiatric disorders. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction with antidepressants compared to placebo in adults aged 65 and older.
The pooled analyses of placebo-controlled trials in children and adolescents with MDD, obsessive compulsive disorder (OCD), or other psychiatric disorders included a total of 24 short-term trials of 9 antidepressant drugs in over 4400 patients. The pooled analyses of placebo-controlled trials in adults with MDD or other psychiatric disorders included a total of 295 short-term trials (median duration of 2 months) of 11 antidepressant drugs in over 77,000 patients. There was considerable variation in risk of suicidality among drugs, but a tendency toward an increase in the younger patients for almost all drugs studied. There were differences in absolute risk of suicidality across the different indications, with the highest incidence in MDD. The risk differences (drug vs placebo), however, were relatively stable within age strata and across indications. These risk differences (drug-placebo difference in the number of cases of suicidality per 1000 patients treated) are provided in Table 1.
| Age Range | Drug-Placebo Difference in Number of Cases of Suicidality per 1000 Patients Treated |
|---|---|
| Increases Compared to Placebo | |
| <18 | 14 additional cases |
| 18–24 | 5 additional cases |
| Decreases Compared to Placebo | |
| 25–64 | 1 fewer case |
| ≥65 | 6 fewer cases |
No suicides occurred in any of the pediatric trials. There were suicides in the adult trials, but the number was not sufficient to reach any conclusion about drug effect on suicide.
It is unknown whether the suicidality risk extends to longer-term use, i.e., beyond several months. However, there is substantial evidence from placebo-controlled maintenance trials in adults with depression that the use of antidepressants can delay the recurrence of depression.
All patients being treated with antidepressants for any indication should be monitored appropriately and observed closely for clinical worsening, suicidality, and unusual changes in behavior, especially during the initial few months of a course of drug therapy, or at times of dose changes, either increases or decreases.
The following symptoms, anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, and mania, have been reported in adult and pediatric patients being treated with antidepressants for major depressive disorder as well as for other indications, both psychiatric and nonpsychiatric. Although a causal link between the emergence of such symptoms and either the worsening of depression and/or the emergence of suicidal impulses has not been established, there is concern that such symptoms may represent precursors to emerging suicidality.
Consideration should be given to changing the therapeutic regimen, including possibly discontinuing the medication, in patients whose depression is persistently worse, or who are experiencing emergent suicidality or symptoms that might be precursors to worsening depression or suicidality, especially if these symptoms are severe, abrupt in onset, or were not part of the patient's presenting symptoms.
Families and caregivers of patients being treated with antidepressants for major depressive disorder or other indications, both psychiatric and nonpsychiatric, should be alerted about the need to monitor patients for the emergence of agitation, irritability, unusual changes in behavior, and the other symptoms described above, as well as the emergence of suicidality, and to report such symptoms immediately to health care providers. Such monitoring should include daily observation by families and caregivers. Prescriptions for Nardil should be written for the smallest quantity of tablets consistent with good patient management, in order to reduce the risk of overdose.
A major depressive episode may be the initial presentation of bipolar disorder. It is generally believed (though not established in controlled trials) that treating such an episode with an antidepressant alone may increase the likelihood of precipitation of a mixed/manic episode in patients at risk for bipolar disorder. Whether any of the symptoms described above represent such a conversion is unknown. However, prior to initiating treatment with an antidepressant, patients with depressive symptoms should be adequately screened to determine if they are at risk for bipolar disorder; such screening should include a detailed psychiatric history, including a family history of suicide, bipolar disorder, and depression. It should be noted that Nardil is not approved for use in treating bipolar depression.
It should be noted that NARDIL is not approved for use in treating any indications in the pediatric population.
The most serious reactions to NARDIL involve changes in blood pressure.
The most important reaction associated with NARDIL administration is the occurrence of hypertensive crises, which have sometimes been fatal.
These crises are characterized by some or all of the following symptoms: occipital headache which may radiate frontally, palpitation, neck stiffness or soreness, nausea, vomiting, sweating (sometimes with fever and sometimes with cold, clammy skin), dilated pupils, and photophobia. Either tachycardia or bradycardia may be present and can be associated with constricting chest pain.
NOTE: Intracranial bleeding has been reported in association with the increase in blood pressure.
Blood pressure should be observed frequently to detect evidence of any pressor response in all patients receiving NARDIL. Therapy should be discontinued immediately upon the occurrence of palpitation or frequent headaches during therapy.
If a hypertensive crisis occurs, NARDIL should be discontinued immediately and therapy to lower blood pressure should be instituted immediately. On the basis of present evidence, phentolamine is recommended. (The dosage reported for phentolamine is 5 mg intravenously.) Care should be taken to administer this drug slowly in order to avoid producing an excessive hypotensive effect. Fever should be managed by means of external cooling.
All patients should be warned that the following foods, beverages, and medications must be avoided while taking NARDIL, and for two weeks after discontinuing use.
Foods and Beverages To Avoid
Meat and Fish
Pickled herring
Liver
Dry sausage (including Genoa salami, hard salami, pepperoni, and Lebanon bologna)
Vegetables
Broad bean pods (fava bean pods)
Sauerkraut
Dairy Products
Cheese (cottage cheese and cream cheese are allowed)
Yogurt
Beverages
Beer and wine
Alcohol-free and reduced-alcohol beer and wine products
Miscellaneous
Yeast extract (including brewer's yeast in large quantities)
Meat extract
Excessive amounts of chocolate and caffeine
Also, any spoiled or improperly refrigerated, handled, or stored protein-rich foods such as meats, fish, and dairy products, including foods that may have undergone protein changes by aging, pickling, fermentation, or smoking to improve flavor should be avoided.
OTC Medications To Avoid
Cold and cough preparations (including those containing dextromethorphan)
Nasal decongestants (tablets, drops, or spray)
Hay-fever medications
Sinus medications
Asthma inhalant medications
Antiappetite medicines
Weight-reducing preparations
"Pep" pills
L-tryptophan containing preparations
Also, certain prescription drugs should be avoided. Therefore, patients under the care of another physician or dentist should inform him/her that they are taking NARDIL.
Patients should be warned that the use of the above foods, beverages, or medications may cause a reaction characterized by headache and other serious symptoms due to a rise in blood pressure, with the exception of dextromethorphan which may cause reactions similar to those seen with meperidine. Also, there has been a report of an interaction between NARDIL and dextromethorphan (ingested as a lozenge) causing drowsiness and bizarre behavior.
Patients should be instructed to report promptly the occurrence of headache or other unusual symptoms.
Concomitant Use with Dibenzazepine Derivative Drugs
If the decision is made to administer NARDIL concurrently with other antidepressant drugs, or within less than 10 days after discontinuation of antidepressant therapy, the patient should be cautioned by the physician regarding the possibility of adverse drug interaction.
A List of Dibenzazepine Derivative Drugs by Generic Name Follows:
nortriptyline hydrochloride
amitriptyline hydrochloride
perphenazine and amitriptyline hydrochloride
clomipramine hydrochloride
desipramine hydrochloride
imipramine hydrochloride
doxepin
carbamazepine
cyclobenzaprine HCl
amoxapine
maprotiline HCl
trimipramine maleate
protriptyline HCl
mirtazapine
NARDIL should be used with caution in combination with antihypertensive drugs, including thiazide diuretics and β-blockers, since exaggerated hypotensive effects may result.
The safe use of NARDIL during pregnancy or lactation has not been established. The potential benefit of this drug, if used during pregnancy, lactation, or in women of childbearing age, should be weighed against the possible hazard to the mother or fetus.
Doses of NARDIL in pregnant mice well exceeding the maximum recommended human dose have caused a significant decrease in the number of viable offspring per mouse. In addition, the growth of young dogs and rats has been retarded by doses exceeding the maximum human dose.
Legal Issues
There is currently no legal information available for this drug.
FDA Safety Alerts
There are currently no FDA safety alerts available for this drug.
Manufacturer Warnings
There is currently no manufacturer warning information available for this drug.
FDA Labeling Changes
There are currently no FDA labeling changes available for this drug.
Uses
NARDIL has been found to be effective in depressed patients clinically characterized as "atypical," "nonendogenous," or "neurotic." These patients often have mixed anxiety and depression and phobic or hypochondriacal features. There is less conclusive evidence of its usefulness with severely depressed patients with endogenous features.
NARDIL should rarely be the first antidepressant drug used. Rather, it is more suitable for use with patients who have failed to respond to the drugs more commonly used for these conditions.
History
There is currently no drug history available for this drug.
Other Information
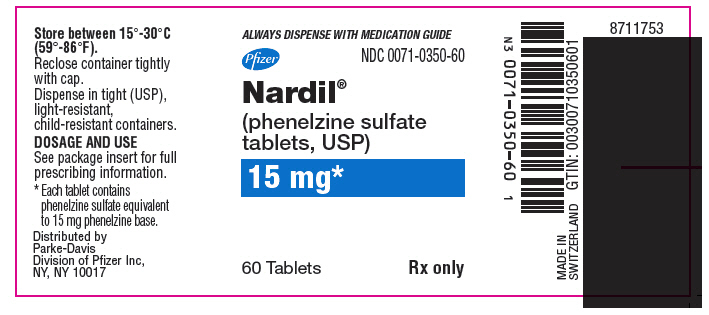
NARDIL® (phenelzine sulfate) is a potent inhibitor of monoamine oxidase (MAO). Phenelzine sulfate is a hydrazine derivative. It has a molecular weight of 234.27 and is chemically described as C8 H12 N2 • H2SO4. Its chemical structure is shown below:

Each NARDIL film-coated tablet for oral administration contains phenelzine sulfate equivalent to 15 mg of phenelzine base and the following inactive ingredients: mannitol, USP; croscarmellose sodium, NF; povidone, USP; edetate disodium, USP; magnesium stearate, NF; isopropyl alcohol, USP; purified water, USP; opadry orange Y30-13242A.
Sources
Brevibloc Manufacturers
-
Baxter Healthcare Corporation
![Brevibloc (Esmolol Hydrochloride) Injection [Baxter Healthcare Corporation]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Brevibloc | Parke-davis Div Of Pfizer Inc
![Brevibloc (Esmolol Hydrochloride) Injection [Baxter Healthcare Corporation] Brevibloc (Esmolol Hydrochloride) Injection [Baxter Healthcare Corporation]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Initial doseThe usual starting dose of NARDIL is one tablet (15 mg) three times a day.
Early phase treatmentDosage should be increased to at least 60 mg per day at a fairly rapid pace consistent with patient tolerance. It may be necessary to increase dosage up to 90 mg per day to obtain sufficient MAO inhibition. Many patients do not show a clinical response until treatment at 60 mg has been continued for at least 4 weeks.
Maintenance doseAfter maximum benefit from NARDIL is achieved, dosage should be reduced slowly over several weeks. Maintenance dose may be as low as one tablet, 15 mg, a day or every other day, and should be continued for as long as is required.
-
General Injectables & Vaccines
![Brevibloc Injection, Solution [General Injectables & Vaccines]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Brevibloc | General Injectables & Vaccines
![Brevibloc Injection, Solution [General Injectables & Vaccines] Brevibloc Injection, Solution [General Injectables & Vaccines]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 Dosing for the Treatment of Supraventricular Tachycardia or Noncompensatory Sinus TachycardiaBREVIBLOC is administered by continuous intravenous infusion with or without a loading dose. Additional loading doses and/or titration of the maintenance infusion (step-wise dosing) may be necessary based on desired ventricular response.
In the absence of loading doses, continuous infusion of a single concentration of esmolol reaches pharmacokinetic and pharmacodynamic steady-state in about 30 minutes.
The effective maintenance dose for continuous and step-wise dosing is 50 to 200 mcg per kg per minute, although doses as low as 25 mcg per kg per minute have been adequate. Dosages greater than 200 mcg per kg per minute provide little added heart rate lowering effect, and the rate of adverse reactions increases.
Maintenance infusions may be continued for up to 48 hours.
2.2 Intraoperative and Postoperative Tachycardia and HypertensionIn this setting it is not always advisable to slowly titrate to a therapeutic effect. Therefore two dosing options are presented: immediate control and gradual control.
Immediate Control
Administer 1 mg per kg as a bolus dose over 30 seconds followed by an infusion of 150 mcg per kg per min if necessary. Adjust the infusion rate as required to maintain desired heart rate and blood pressure. Refer to Maximum Recommended Doses below.Gradual Control
Administer 500 mcg per kg as a bolus dose over 1 minute followed by a maintenance infusion of 50 mcg per kg per min for 4 minutes. Depending on the response obtained, continue dosing as outlined for supraventricular tachycardia. Refer to Maximum Recommended Doses below.Maximum Recommended Doses
For the treatment of tachycardia, maintenance infusion dosages greater than 200 mcg per kg per min are not recommended; dosages greater than 200 mcg per kg per min provide little additional heart rate-lowering effect, and the rate of adverse reactions increases. For the treatment of hypertension, higher maintenance infusion dosages (250-300 mcg per kg per min) may be required. The safety of doses above 300 mcg per kg per minute has not been studied. 2.3 Transition from BREVIBLOC Injection Therapy to Alternative DrugsAfter patients achieve adequate control of the heart rate and a stable clinical status, transition to alternative antiarrhythmic drugs may be accomplished.
When transitioning from BREVIBLOC to alternative drugs, the physician should carefully consider the labeling instructions of the alternative drug selected and reduce the dosage of BREVIBLOC as follows:
Thirty minutes following the first dose of the alternative drug, reduce the BREVIBLOC infusion rate by one-half (50%). After administration of the second dose of the alternative drug, monitor the patient's response and if satisfactory control is maintained for the first hour, discontinue the BREVIBLOC infusion. 2.4 Directions for UseBREVIBLOC injection is available in a pre-mixed bag and ready-to-use vial. BREVIBLOC is not compatible with Sodium Bicarbonate (5%) solution (limited stability) or furosemide (precipitation).
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Premixed Bag
The medication port is to be used solely for withdrawing an initial bolus from the bag. Use aseptic technique when withdrawing the bolus dose. Do not add any additional medications to the bag.Ready-to-Use Vial
The Ready-to-use Vial may be used to administer a loading dosage by hand-held syringe while the maintenance infusion is being prepared [see How Supplied/Storage and Handling (16.2)].
Compatibility with Commonly Used Intravenous Fluids
BREVIBLOC was tested for compatibility with ten commonly used intravenous fluids at a final concentration of 10 mg esmolol hydrochloride per mL. BREVIBLOC was found to be compatible with the following solutions and was stable for at least 24 hours at controlled room temperature or under refrigeration:
Dextrose (5%) Injection, USP Dextrose (5%) in Lactated Ringer's Injection Dextrose (5%) in Ringer's Injection Dextrose (5%) and Sodium Chloride (0.45%) Injection, USP Dextrose (5%) and Sodium Chloride (0.9%) Injection, USP Lactated Ringer's Injection, USP Potassium Chloride (40 mEq/liter) in Dextrose (5%) Injection, USP Sodium Chloride (0.45%) Injection, USP Sodium Chloride (0.9%) Injection, USP
Login To Your Free Account


![Brevibloc Injection, Solution [General Injectables & Vaccines]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=c8d2e135-ec31-4eee-bce2-c85e7858c5e1&name=Label1.jpg)