FDA records indicate that there are no current recalls for this drug.
Are you a medical professional?
Trending Topics
Bupropion Hydrochloride Er Recall
Get an alert when a recall is issued.
Questions & Answers
Side Effects & Adverse Reactions
Clinical Worsening and Suicide Risk in Treating Psychiatric Disorders:
Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications, and this risk may persist until significant remission occurs. Suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide. There has been a long-standing concern, however, that antidepressants may have a role in inducing worsening of depression and the emergence of suicidality in certain patients during the early phases of treatment. Pooled analyses of short-term placebo-controlled trials of antidepressant drugs (SSRIs and others) showed that these drugs increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (ages 18 to 24) with major depressive disorder (MDD) and other psychiatric disorders. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction with antidepressants compared to placebo in adults aged 65 and older.
The pooled analyses of placebo-controlled trials in children and adolescents with MDD, obsessive compulsive disorder (OCD), or other psychiatric disorders included a total of 24 short-term trials of 9 antidepressant drugs in over 4,400 patients. The pooled analyses of placebo-controlled trials in adults with MDD or other psychiatric disorders included a total of 295 short-term trials (median duration of 2 months) of 11 antidepressant drugs in over 77,000 patients. There was considerable variation in risk of suicidality among drugs, but a tendency toward an increase in the younger patients for almost all drugs studied. There were differences in absolute risk of suicidality across the different indications, with the highest incidence in MDD. The risk differences (drug vs placebo), however, were relatively stable within age strata and across indications.
No suicides occurred in any of the pediatric trials. There were suicides in the adult trials, but the number was not sufficient to reach any conclusion about drug effect on suicide.
It is unknown whether the suicidality risk extends to longer-term use, i.e., beyond several months. However, there is substantial evidence from placebo-controlled maintenance trials in adults with depression that the use of antidepressants can delay the recurrence of depression.
All patients being treated with antidepressants for any indication should be monitored appropriately and observed closely for clinical worsening, suicidality, and unusual changes in behavior, especially during the initial few months of a course of drug therapy, or at times of dose changes, either increases or decreases.
The following symptoms, anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, and mania, have been reported in adult and pediatric patients being treated with antidepressants for major depressive disorder as well as for other indications, both psychiatric and nonpsychiatric. Although a causal link between the emergence of such symptoms and either the worsening of depression and/or the emergence of suicidal impulses has not been established, there is concern that such symptoms may represent precursors to emerging suicidality.
Consideration should be given to changing the therapeutic regimen, including possibly discontinuing the medication, in patients whose depression is persistently worse, or who are experiencing emergent suicidality or symptoms that might be precursors to worsening depression or suicidality, especially if these symptoms are severe, abrupt in onset, or were not part of the patient’s presenting symptoms.
Families and caregivers of patients being treated with antidepressants for major depressive disorder or other indications, both psychiatric and nonpsychiatric, should be alerted about the need to monitor patients for the emergence of agitation, irritability, unusual changes in behavior, and the other symptoms described above, as well as the emergence of suicidality, and to report such symptoms immediately to health care providers. Such monitoring should include daily observation by families and caregivers. Prescriptions for bupropion should be written for the smallest quantity of tablets consistent with good patient management, in order to reduce the risk of overdose.
Neuropsychiatric Symptoms and Suicide Risk in Smoking Cessation Treatment:
Bupropion hydrochloride tablets, bupropion hydrochloride extended-release tablets (SR), and bupropion hydrochloride extended-release tablets (XL) are not approved for smoking cessation treatment, but bupropion under the name ZYBAN# is approved for this use. Serious neuropsychiatric symptoms have been reported in patients taking bupropion for smoking cessation (see BOXED WARNING, ADVERSE REACTIONS). These have included changes in mood (including depression and mania), psychosis, hallucinations, paranoia, delusions, homicidal ideation, hostility, agitation, aggression, anxiety, and panic, as well as suicidal ideation, suicide attempt, and completed suicide. Some reported cases may have been complicated by the symptoms of nicotine withdrawal in patients who stopped smoking. Depressed mood may be a symptom of nicotine withdrawal. Depression, rarely including suicidal ideation, has been reported in smokers undergoing a smoking cessation attempt without medication. However, some of these symptoms have occurred in patients taking bupropion who continued to smoke. When symptoms were reported, most were during bupropion treatment, but some were following discontinuation of bupropion therapy.
These events have occurred in patients with and without pre-existing psychiatric disease; some have experienced worsening of their psychiatric illnesses. All patients being treated with bupropion as part of smoking cessation treatment should be observed for neuropsychiatric symptoms or worsening of pre-existing psychiatric illness.
Patients with serious psychiatric illness such as schizophrenia, bipolar disorder, and major depressive disorder did not participate in the pre-marketing studies of ZYBAN#.
Advise patients and caregivers that the patient using bupropion for smoking cessation should stop taking bupropion and contact a healthcare provider immediately if agitation, depressed mood, or changes in behavior or thinking that are not typical for the patient are observed, or if the patient develops suicidal ideation or suicidal behavior. In many postmarketing cases, resolution of symptoms after discontinuation of ZYBAN# was reported, although in some cases the symptoms persisted, therefore, ongoing monitoring and supportive care should be provided until symptoms resolve.
The risks of using bupropion for smoking cessation should be weighed against the benefits of its use. ZYBAN# has been demonstrated to increase the likelihood of abstinence from smoking for as long as six months compared to treatment with placebo. The health benefits of quitting smoking are immediate and substantial.
Screening Patients for Bipolar Disorder:
A major depressive episode may be the initial presentation of bipolar disorder. It is generally believed (though not established in controlled trials) that treating such an episode with an antidepressant alone may increase the likelihood of precipitation of a mixed/manic episode in patients at risk for bipolar disorder. Whether any of the symptoms described above represent such a conversion is unknown. However, prior to initiating treatment with an antidepressant, patients with depressive symptoms should be adequately screened to determine if they are at risk for bipolar disorder; such screening should include a detailed psychiatric history, including a family history of suicide, bipolar disorder, and depression. It should be noted that bupropion is not approved for use in treating bipolar depression.
Bupropion-Containing Products
Patients should be made aware that bupropion hydrochloride extended-release tablets (SR) contains the same active ingredient found in ZYBAN®#, used as an aid to smoking cessation treatment, and that bupropion hydrochloride extended-release tablets (SR) should not be used in combination with ZYBAN®#, or any other medications that contain bupropion hydrochloride, (such as bupropion hydrochloride tablets, the immediate-release formulation or bupropion hydrochloride extended-release tablets (XL), the extended-release formulation).
Seizures:
Bupropion is associated with a dose-related risk of seizures. The risk of seizures is also related to patient factors, clinical situations, and concomitant medications, which must be considered in selection of patients for therapy with bupropion. Bupropion should be discontinued and not restarted in patients who experience a seizure while on treatment.
Dose: At doses of bupropion up to a dose of 300 mg/day, the incidence of seizure is approximately 0.1% (1/1,000) and increases to approximately 0.4% (4/1,000) at the maximum recommended dose of 400 mg/day.
Data for the immediate-release formulation of bupropion revealed a seizure incidence of approximately 0.4% (i.e., 13 of 3,200 patients followed prospectively) in patients treated at doses in a range of 300 to 450 mg/day. The 450 mg/day upper limit of this dose range is close to the currently recommended maximum dose of 400 mg/day for bupropion hydrochloride extended-release tablets (SR). This seizure incidence (0.4%) may exceed that of other marketed antidepressants and bupropion hydrochloride extended-release tablets (SR) up to 300 mg/day by as much as 4-fold. This relative risk is only an approximate estimate because no direct comparative studies have been conducted.
Additional data accumulated for the immediate-release formulation of bupropion suggested that the estimated seizure incidence increases almost tenfold between 450 and 600 mg/day, which is twice the usual adult dose and one and one-half the maximum recommended daily dose (400 mg) of bupropion hydrochloride extended-release tablets (SR). This disproportionate increase in seizure incidence with dose incrementation calls for caution in dosing.
Data for bupropion hydrochloride extended-release tablets (SR) revealed a seizure incidence of approximately 0.1% (i.e., 3 of 3,100 patients followed prospectively) in patients treated at doses in a range of 100 to 300 mg/day. It is not possible to know if the lower seizure incidence observed in this study involving the sustained-release formulation of bupropion resulted from the different formulation or the lower dose used. However, as noted above, the immediate-release and sustained-release formulations are bioequivalent with regard to both rate and extent of absorption during steady state (the most pertinent condition to estimating seizure incidence), since most observed seizures occur under steady-state conditions.
Patient factors: Predisposing factors that may increase the risk of seizure with bupropion use include history of head trauma or prior seizure, central nervous system (CNS) tumor, the presence of severe hepatic cirrhosis, and concomitant medications that lower seizure threshold.
Clinical situations: Circumstances associated with an increased seizure risk include, among others, excessive use of alcohol or sedatives (including benzodiazepines); addiction to opiates, cocaine, or stimulants; use of over-the-counter stimulants and anorectics; and diabetes treated with oral hypoglycemics or insulin.
Concomitant medications: Many medications (e.g., antipsychotics, antidepressants, theophylline, systemic steroids) are known to lower seizure threshold.
Recommendations for Reducing the Risk of Seizure: Retrospective analysis of clinical experience gained during the development of bupropion suggests that the risk of seizure may be minimized if
the total daily dose of bupropion hydrochloride extended-release tablets (SR) does not exceed 400 mg,
the daily dose is administered twice daily, and
the rate of incrementation of dose is gradual.
No single dose should exceed 200 mg to avoid high peak concentrations of bupropion and/or its metabolites.
Bupropion should be administered with extreme caution to patients with a history of seizure, cranial trauma, or other predisposition(s) toward seizure, or patients treated with other agents (e.g., antipsychotics, other antidepressants, theophylline, systemic steroids, etc.) that lower seizure threshold.
Hepatic Impairment:
Bupropion should be used with extreme caution in patients with severe hepatic cirrhosis. In these patients a reduced frequency and/or dose is required, as peak bupropion, as well as AUC, levels are substantially increased and accumulation is likely to occur in such patients to a greater extent than usual. The dose should not exceed 100 mg every day or 150 mg every other day in these patients (see CLINICAL PHARMACOLOGY, PRECAUTIONS, and DOSAGE AND ADMINISTRATION).
Potential for Hepatotoxicity:
In rats receiving large doses of bupropion chronically, there was an increase in incidence of hepatic hyperplastic nodules and hepatocellular hypertrophy. In dogs receiving large doses of bupropion chronically, various histologic changes were seen in the liver, and laboratory tests suggesting mild hepatocellular injury were noted.
Legal Issues
There is currently no legal information available for this drug.
FDA Safety Alerts
There are currently no FDA safety alerts available for this drug.
Manufacturer Warnings
There is currently no manufacturer warning information available for this drug.
FDA Labeling Changes
There are currently no FDA labeling changes available for this drug.
Uses
Bupropion hydrochloride extended-release tablets (SR) are indicated for the treatment of major depressive disorder.
The efficacy of bupropion in the treatment of a major depressive episode was established in two 4-week controlled trials of depressed inpatients and in one 6-week controlled trial of depressed outpatients whose diagnoses corresponded most closely to the Major Depression category of the APA Diagnostic and Statistical Manual (DSM) (see CLINICAL PHARMACOLOGY).
A major depressive episode (DSM-IV) implies the presence of 1) depressed mood or 2) loss of interest or pleasure; in addition, at least 5 of the following symptoms have been present during the same 2-week period and represent a change from previous functioning: depressed mood, markedly diminished interest or pleasure in usual activities, significant change in weight and/or appetite, insomnia or hypersomnia, psychomotor agitation or retardation, increased fatigue, feelings of guilt or worthlessness, slowed thinking or impaired concentration, a suicide attempt or suicidal ideation.
The efficacy of bupropion hydrochloride extended-release tablets (SR) in maintaining an antidepressant response for up to 44 weeks following 8 weeks of acute treatment was demonstrated in a placebo-controlled trial (see CLINICAL PHARMACOLOGY). Nevertheless, the physician who elects to use bupropion hydrochloride extended-release tablets (SR) for extended periods should periodically reevaluate the long-term usefulness of the drug for the individual patient.
History
There is currently no drug history available for this drug.
Other Information
There are no additional details available for this product.
Sources
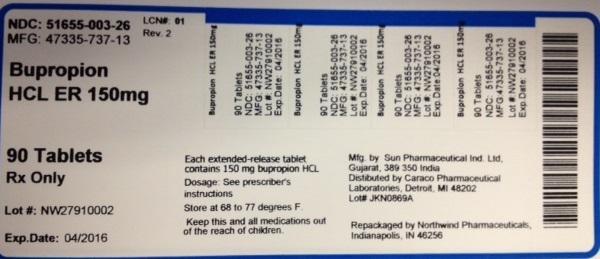
Bupropion Hydrochloride Er Manufacturers
-
Northwind Pharmaceuticals
![Bupropion Hydrochloride Er (Bupropion Hydrochloride) Tablet [Northwind Pharmaceuticals]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Bupropion Hydrochloride Er | Northwind Pharmaceuticals
![Bupropion Hydrochloride Er (Bupropion Hydrochloride) Tablet [Northwind Pharmaceuticals] Bupropion Hydrochloride Er (Bupropion Hydrochloride) Tablet [Northwind Pharmaceuticals]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
General Dosing Considerations: It is particularly important to administer bupropion hydrochloride extended-release tablets (SR) in a manner most likely to minimize the risk of seizure (see WARNINGS). Gradual escalation in dosage is also important if agitation, motor restlessness, and insomnia, often seen during the initial days of treatment, are to be minimized. If necessary, these effects may be managed by temporary reduction of dose or the short-term administration of an intermediate to long-acting sedative hypnotic. A sedative hypnotic usually is not required beyond the first week of treatment. Insomnia may also be minimized by avoiding bedtime doses. If distressing, untoward effects supervene, dose escalation should be stopped.
Bupropion hydrochloride extended-release tablets (SR) should be swallowed whole and not crushed, divided, or chewed.
Initial Treatment: The usual adult target dose for bupropion hydrochloride extended-release tablets (SR) is 300 mg/day, given as 150 mg twice daily. Dosing with bupropion hydrochloride extended-release tablets (SR) should begin at 150 mg/day given as a single daily dose in the morning. If the 150 mg initial dose is adequately tolerated, an increase to the 300 mg/day target dose, given as 150 mg twice daily, may be made as early as day 4 of dosing. There should be an interval of at least 8 hours between successive doses.
Increasing the Dosage Above 300 mg/day: As with other antidepressants, the full antidepressant effect of bupropion hydrochloride extended-release tablets (SR) may not be evident until 4 weeks of treatment or longer. An increase in dosage to the maximum of 400 mg/day, given as 200 mg twice daily, may be considered for patients in whom no clinical improvement is noted after several weeks of treatment at 300 mg/day.
Maintenance Treatment: It is generally agreed that acute episodes of depression require several months or longer of sustained pharmacological therapy beyond response to the acute episode. In a study in which patients with major depressive disorder, recurrent type, who had responded during 8 weeks of acute treatment with bupropion were assigned randomly to placebo or to the same dose of bupropion (150 mg twice daily) during 44 weeks of maintenance treatment as they had received during the acute stabilization phase, longer-term efficacy was demonstrated (see CLINICAL TRIALS under CLINICAL PHARMACOLOGY). Based on these limited data, it is unknown whether or not the dose of bupropion needed for maintenance treatment is identical to the dose needed to achieve an initial response. Patients should be periodically reassessed to determine the need for maintenance treatment and the appropriate dose for such treatment.
Dosage Adjustment for Patients with Impaired Hepatic Function: Bupropion should be used with extreme caution in patients with severe hepatic cirrhosis. The dose should not exceed 100 mg every day or 150 mg every other day in these patients. Bupropion should be used with caution in patients with hepatic impairment (including mild-to-moderate hepatic cirrhosis) and a reduced frequency and/or dose should be considered in patients with mild-to-moderate hepatic cirrhosis (see CLINICAL PHARMACOLOGY, WARNINGS, and PRECAUTIONS).
Dosage Adjustment for Patients with Impaired Renal Function: Bupropion should be used with caution in patients with renal impairment and a reduced frequency and/or dose should be considered (see CLINICAL PHARMACOLOGY and PRECAUTIONS).
Login To Your Free Account