FDA records indicate that there are no current recalls for this drug.
Are you a medical professional?
Trending Topics
Hypertensolol Recall
Get an alert when a recall is issued.
Questions & Answers
Side Effects & Adverse Reactions
WARNINGS
Hypertension and Angina
Cardiac Failure
Sympathetic stimulation is a vital component supporting circulatory function in congestive heart failure, and beta blockade carries the potential hazard of further depressing myocardial contractility and precipitating more severe failure. In hypertensive and angina patients who have congestive heart failure controlled by digitalis and diuretics, metoprolol should be administered cautiously.
In Patients Without a History of Cardiac Failure
Continued depression of the myocardium with beta-blocking agents over a period of time can, in some cases, lead to cardiac failure. At the first sign or symptom of impending cardiac failure, patients should be fully digitalized and/or given a diuretic. The response should be observed closely. If cardiac failure continues, despite adequate digitalization and diuretic therapy, metoprolol should be withdrawn.
Bronchospastic Diseases
PATIENTS WITH BRONCHOSPASTIC DISEASES SHOULD, IN GENERAL, NOT RECEIVE BETA BLOCKERS, including metoprolol. Because of its relative beta1 selectivity, however, metoprolol may be used with caution in patients with bronchospastic disease who do not respond to, or cannot tolerate, other antihypertensive treatment. Since beta1 selectivity is not absolute, a beta2-stimulating agent should be administered concomitantly, and the lowest possible dose of metoprolol tartrate should be used. In these circumstances it would be prudent initially to administer metoprolol in smaller doses three times daily, instead of larger doses two times daily, to avoid the higher plasma levels associated with the longer dosing interval (see DOSAGE AND ADMINISTRATION).
Major Surgery
The necessity or desirability of withdrawing beta-blocking therapy, including metoprolol, prior to major surgery is controversial; the impaired ability of the heart to respond to reflex adrenergic stimuli may augment the risks of general anesthesia and surgical procedures.
Metoprolol, like other beta blockers, is a competitive inhibitor of beta-receptor agonists, and its effects can be reversed by administration of such agents, e.g., dobutamine or isoproterenol. However, such patients may be subject to protracted severe hypotension. Difficulty in restarting and maintaining the heart beat has also been reported with beta blockers.
Diabetes and Hypoglycemia
Metoprolol should be used with caution in diabetic patients if a beta-blocking agent is required. Beta blockers may mask tachycardia occurring with hypoglycemia, but other manifestations such as dizziness and sweating may not be significantly affected.
Pheochromocytoma
If metoprolol is used in the setting of pheochromocytoma, it should be given in combination with an alpha blocker, and only after the alpha blocker has been initiated. Administration of beta blockers alone in the setting of pheochromocytoma has been associated with a paradoxical increase in blood pressure due to the attenuation of beta-mediated vasodilatation in skeletal muscle.
Thyrotoxicosis
Beta-adrenergic blockade may mask certain clinical signs (e.g., tachycardia) of hyperthyroidism. Patients suspected of developing thyrotoxicosis should be managed carefully to avoid abrupt withdrawal of beta blockade, which might precipitate a thyroid storm.
Myocardial Infarction
Cardiac Failure
Sympathetic stimulation is a vital component supporting circulatory function, and beta blockade carries the potential hazard of depressing myocardial contractility and precipitating or exacerbating minimal cardiac failure.
During treatment with metoprolol, the hemodynamic status of the patient should be carefully monitored. If heart failure occurs or persists despite appropriate treatment, metoprolol should be discontinued.
Bradycardia
Metoprolol produces a decrease in sinus heart rate in most patients; this decrease is greatest among patients with high initial heart rates and least among patients with low initial heart rates. Acute myocardial infarction (particularly inferior infarction) may in itself produce significant lowering of the sinus rate. If the sinus rate decreases to less than 40 beats/min, particularly if associated with evidence of lowered cardiac output, atropine (0.25 to 0.5 mg) should be administered intravenously. If treatment with atropine is not successful, metoprolol should be discontinued, and cautious administration of isoproterenol or installation of a cardiac pacemaker should be considered.
AV Block
Metoprolol slows AV conduction and may produce significant first- (P-R interval greater than or equal to 0.26 sec), second-, or third-degree heart block. Acute myocardial infarction also produces heart block.
If heart block occurs, metoprolol should be discontinued and atropine (0.25 to 0.5 mg) should be administered intravenously. If treatment with atropine is not successful, cautious administration of isoproterenol or installation of a cardiac pacemaker should be considered.
Hypotension
If hypotension (systolic blood pressure less than or equal to 90 mmHg) occurs, metoprolol should be discontinued, and the hemodynamic status of the patient and the extent of myocardial damage carefully assessed. Invasive monitoring of central venous, pulmonary capillary wedge, and arterial pressures may be required. Appropriate therapy with fluids, positive inotropic agents, balloon counterpulsation, or other treatment modalities should be instituted. If hypotension is associated with sinus bradycardia or AV block, treatment should be directed at reversing these (see above).
Bronchospastic Diseases
PATIENTS WITH BRONCHOSPASTIC DISEASES SHOULD, IN GENERAL, NOT RECEIVE BETA BLOCKERS, including metoprolol. Because of its relative beta1 selectivity, metoprolol may be used with extreme caution in patients with bronchospastic disease. Because it is unknown to what extent beta2-stimulating agents may exacerbate myocardial ischemia and the extent of infarction, these agents should not be used prophylactically. If bronchospasm not related to congestive heart failure occurs, metoprolol should be discontinued. A theophylline derivative or a beta2 agonist may be administered cautiously, depending on the clinical condition of the patient. Both theophylline derivatives and beta2 agonists may produce serious cardiac arrhythmias.
Legal Issues
There is currently no legal information available for this drug.
FDA Safety Alerts
There are currently no FDA safety alerts available for this drug.
Manufacturer Warnings
There is currently no manufacturer warning information available for this drug.
FDA Labeling Changes
There are currently no FDA labeling changes available for this drug.
Uses
INDICATIONS AND USAGE
Hypertension
Metoprolol tartrate tablets are indicated for the treatment of hypertension. They may be used alone or in combination with other antihypertensive agents.
Angina Pectoris
Metoprolol tartrate tablets are indicated in the long-term treatment of angina pectoris.
Myocardial Infarction
Metoprolol tartrate tablets are indicated in the treatment of hemodynamically stable patients with definite or suspected acute myocardial infarction to reduce cardiovascular mortality. Treatment with intravenous metoprolol tartrate can be initiated as soon as the patient's clinical condition allows (see DOSAGE AND ADMINISTRATION, CONTRAINDICATIONS, and WARNINGS). Alternatively, treatment can begin within 3 to 10 days of the acute event (see DOSAGE AND ADMINISTRATION).
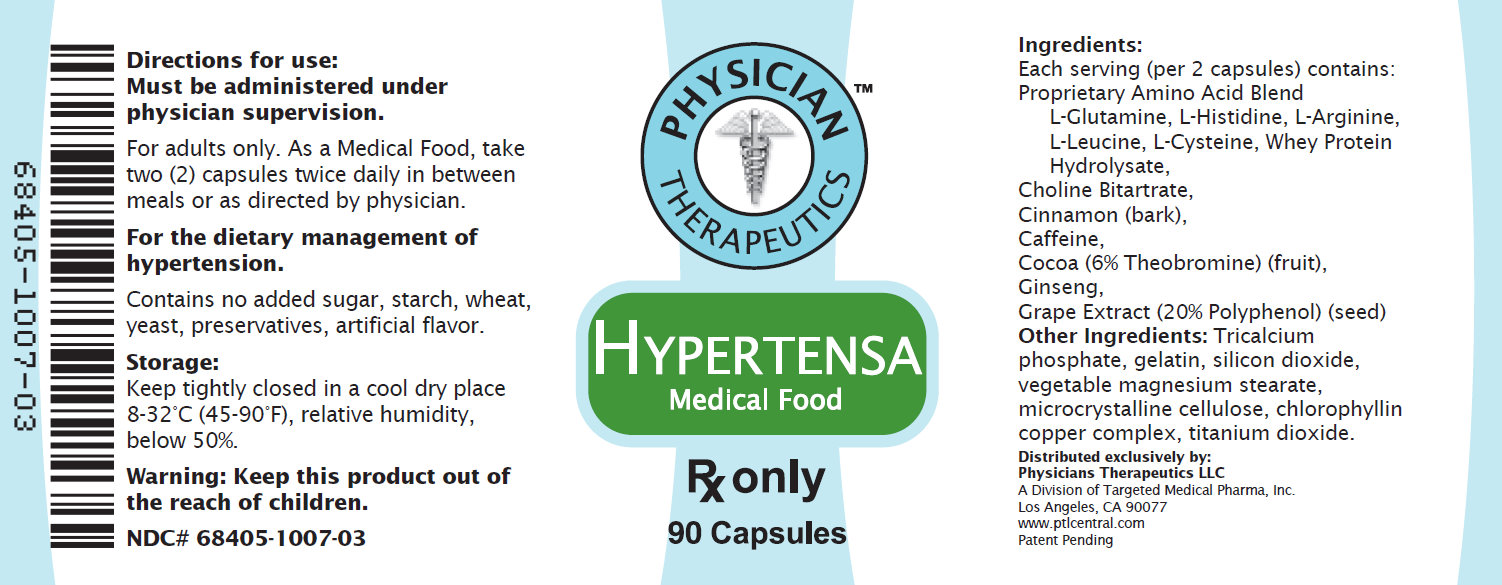
INDICATIONS FOR USE Hypertensa is intended for the clinical dietary management of the metabolic processes in patients with hypertension.
History
There is currently no drug history available for this drug.
Other Information
DESCRIPTION
Metoprolol tartrate is a selective beta1-adrenoreceptor blocking agent, available as 50 and 100 mg tablets for oral administration. Metoprolol tartrate is 1-(isopropylamino)-3-[p-(2-methoxyethyl) phenoxy]-2-propanol (2:1) dextro-tartrate salt, and its structural formula is:

PRODUCT DESCRIPTION Primary Ingredients Hypertensa consists of a proprietary blend of amino acids, cocoa, cinnamon and flavonoids in specific proportions. These ingredients fall into the category of Generally Regarded as Safe” (GRAS) as defined by the Food and Drug Administration (FDA) (Sections 201(s) and 409 of the Federal Food, Drug, and Cosmetic Act). A GRAS substance is distinguished from a food additive on the basis of the common knowledge about the safety of the substance for its intended use. The standard for an ingredient to achieve GRAS status requires not only technical demonstration of non-toxicity and safety, but also general recognition of safety through widespread usage and agreement of that safety by experts in the field. Many ingredients have been determined by the U.S. Food and Drug Administration (FDA) to be GRAS, and are listed as such by regulation, in Volume 21 Code of Federal Regulations (CFR) Sections 182, 184, and 186. Amino Acids Amino Acids are the building blocks of proteins. All amino acids are GRAS listed as they have been ingested by humans for thousands of years. The doses of the amino acids in Hypertensa are equivalent to those found in the usual human diet. Patients with hypertension may require an increased amount of certain amino acids that cannot be obtained from normal diet alone. Arginine, for example, is a conditional amino acid. The body can make arginine in the liver, but the liver produced arginine can only be used in the liver itself. Arginine is needed to produce nitric oxide (NO). NO is required to dilate the constricted blood vessels that are the cause of high blood pressure. Patients with hypertension have an increase in the enzyme, arginase that degrades arginine before it can be used to produce NO. Some patients with hypertension have a resistance to the use of arginine that is similar to the mechanism found in insulin resistance that is genetically determined. Patients with hypertension cannot acquire sufficient arginine from the diet without ingesting a prohibitively large amount of calories, particularly calories from protein. . Flavonoids Flavonoids are a group of phytochemical compounds found in all vascular plants including fruits and vegetables. They are a part of a larger class of compounds known as polyphenols. Many of the therapeutic or health benefits of colored fruits and vegetables, cocoa, red wine, and green tea are directly related to their flavonoid content. The specially formulated flavonoids found in Hypertensa cannot be obtained from conventional foods in the necessary proportions to elicit a therapeutic response. Other Ingredients Hypertensa contains the following “inactive” or other ingredients, as fillers, excipients, and colorings: magnesium stearate, microcrystalline cellulose, Maltodextrin NF, gelatin (as the capsule material), Physical Description Hypertensa is a yellow to light brown powder. Hypertensa contains L-Glutamine, L-Histadine, L-Arginine, L-Leucine, L-Cysteine, Whey Protein Hydrolysate, Choline Bitartrate, Cinnamon, Caffeine, Cocoa, Ginseng, and Grape Extract.
Sources
Hypertensolol Manufacturers
-
Physician Therapeutics Llc
![Hypertensolol (Metoprolol Tartrate, Arginine) Kit [Physician Therapeutics Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Hypertensolol | Physician Therapeutics Llc
![Hypertensolol (Metoprolol Tartrate, Arginine) Kit [Physician Therapeutics Llc] Hypertensolol (Metoprolol Tartrate, Arginine) Kit [Physician Therapeutics Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
DOSAGE AND ADMINISTRATION
Hypertension
The dosage of metoprolol tartrate tablets USP should be individualized. Metoprolol tartrate tablets should be taken with or immediately following meals.
The usual initial dosage of metoprolol tartrate tablets USP is 100 mg daily in single or divided doses, whether used alone or added to a diuretic. The dosage may be increased at weekly (or longer) intervals until optimum blood pressure reduction is achieved. In general, the maximum effect of any given dosage level will be apparent after 1 week of therapy. The effective dosage range of metoprolol tartrate tablets USP is 100 to 450 mg per day. Dosages above 450 mg per day have not been studied. While once-daily dosing is effective and can maintain a reduction in blood pressure throughout the day, lower doses (especially 100 mg) may not maintain a full effect at the end of the 24 hour period, and larger or more frequent daily doses may be required. This can be evaluated by measuring blood pressure near the end of the dosing interval to determine whether satisfactory control is being maintained throughout the day. Beta1 selectivity diminishes as the dose of metoprolol is increased.
Angina Pectoris
The dosage of metoprolol tartrate tablets USP should be individualized. Metoprolol tartrate tablets should be taken with or immediately following meals.
The usual initial dosage of metoprolol tartrate tablets USP 100 mg daily, given in two divided doses. The dosage may be gradually increased at weekly intervals until optimum clinical response has been obtained or there is pronounced slowing of the heart rate. The effective dosage range of metoprolol tartrate tablets USP is 100 to 400 mg per day. Dosages above 400 mg per day have not been studied. If treatment is to be discontinued, the dosage should be reduced gradually over a period of 1 to 2 weeks (see WARNINGS).
Myocardial Infarction
Early Treatment
During the early phase of definite or suspected acute myocardial infarction, treatment with metoprolol tartrate can be initiated as soon as possible after the patient's arrival in the hospital. Such treatment should be initiated in a coronary care or similar unit immediately after the patient's hemodynamic condition has stabilized.
Treatment in this early phase should begin with the intravenous administration of three bolus injections of 5 mg of metoprolol tartrate each; the injections should be given at approximately 2 minute intervals. During the intravenous administration of metoprolol, blood pressure, heart rate, and electrocardiogram should be carefully monitored.
In patients who tolerate the full intravenous dose (15 mg), metoprolol tartrate tablets USP, 50 mg every 6 hours, should be initiated 15 minutes after the last intravenous dose and continued for 48 hours. Thereafter, patients should receive a maintenance dosage of 100 mg twice daily (see Late Treatment below).
Patients who appear not to tolerate the full intravenous dose should be started on metoprolol tartrate tablets USP either 25 mg or 50 mg every 6 hours (depending on the degree of intolerance) 15 minutes after the last intravenous dose or as soon as their clinical condition allows. In patients with severe intolerance, treatment with metoprolol should be discontinued (see WARNINGS).
Late Treatment
Patients with contraindications to treatment during the early phase of suspected or definite myocardial infarction, patients who appear not to tolerate the full early treatment, and patients in whom the physician wishes to delay therapy for any other reason should be started on metoprolol tartrate tablets USP, 100 mg twice daily, as soon as their clinical condition allows. Therapy should be continued for at least 3 months. Although the efficacy of metoprolol beyond 3 months has not been conclusively established, data from studies with other beta blockers suggest that treatment should be continued for 1 to 3 years.
Note: Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.DOSAGE AND ADMINISTRATION Recommended Administration For the dietary management of the metabolic processes associated with hypertension. Take (2) capsules once or twice daily, as directed by physician. As with most amino acid formulations Hypertensa should be taken without food to increase the absorption of key ingredients.
Login To Your Free Account