FDA records indicate that there are no current recalls for this drug.
Are you a medical professional?
Trending Topics
Lamotrigine Recall
Get an alert when a recall is issued.
Questions & Answers
Side Effects & Adverse Reactions
There is currently no warning information available for this product. We apologize for any inconvenience.
Legal Issues
There is currently no legal information available for this drug.
FDA Safety Alerts
There are currently no FDA safety alerts available for this drug.
Manufacturer Warnings
There is currently no manufacturer warning information available for this drug.
FDA Labeling Changes
There are currently no FDA labeling changes available for this drug.
Uses
1.1 Epilepsy
Adjunctive Therapy:
Lamotrigine tablets are indicated as adjunctive therapy for the following seizure types in patients ≥ 2 years of age:
partial seizures
primary generalized tonic-clonic seizures
generalized seizures of Lennox-Gastaut syndrome
Monotherapy:
Lamotrigine tablets are indicated for conversion to monotherapy in adults (≥16 years of age) with partial seizures who are receiving treatment with carbamazepine, phenytoin, phenobarbital, primidone, or valproate as the single antiepileptic drug (AED).
Safety and effectiveness of lamotrigine tablets have not been established (1) as initial monotherapy; (2) for conversion to monotherapy from AEDs other than carbamazepine, phenytoin, phenobarbital, primidone, or valproate; or (3) for simultaneous conversion to monotherapy from 2 or more concomitant AEDs.
1.2 Bipolar Disorder
Lamotrigine tablets are indicated for the maintenance treatment of Bipolar I Disorder to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in adults (≥18 years of age) treated for acute mood episodes with standard therapy. The effectiveness of lamotrigine tablets in the acute treatment of mood episodes has not been established.
The effectiveness of lamotrigine tablets as maintenance treatment was established in 2 placebo-controlled trials in patients with Bipolar I Disorder as defined by DSM-IV [see Clinical Studies (14.2)]. The physician who elects to prescribe lamotrigine tablets for periods extending beyond 16 weeks should periodically re-evaluate the long-term usefulness of the drug for the individual patient.
History
There is currently no drug history available for this drug.
Other Information
-
Lamotrigine, an AED of the phenyltriazine class, is chemically unrelated to existing AEDs. Its chemical name is 3,5-diamino-6-(2,3-dichlorophenyl)-as-triazine, its molecular formula is C9H7N5Cl2, and its molecular weight is 256.09. Lamotrigine is a white to pale cream-colored powder and has a pKa of 5.7. Lamotrigine is very slightly soluble in water (0.17 mg/mL at 25°C) and slightly soluble in 0.1 M HCl (4.1 mg/mL at 25°C). The structural formula is:
Lamotrigine tablets USP are supplied for oral administration as 25 mg, 100 mg, 150 mg or 200 mg tablets. Each tablet contains the labeled amount of lamotrigine and the following inactive ingredients: lactose monohydrate, magnesium stearate, microcrystalline cellulose, povidone and sodium starch glycolate. In addition, the 200 mg tablets contain FD&C Blue No. 2 Lake.
Sources
Lamotrigine Manufacturers
-
Direct Rx
![Lamotrigine Tablet [Direct Rx]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Direct Rx
![Lamotrigine Tablet [Direct Rx] Lamotrigine Tablet [Direct Rx]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning ]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablet is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3) ].
Lamotrigine Tablets Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3) ] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3) ].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3) ], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3) ].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3) ]. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6) , Clinical Pharmacology (12.3) ], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7) , Clinical Pharmacology (12.3) ]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.
Discontinuation Strategy:
Epilepsy: For patients receiving lamotrigine tablets in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9) ].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9) ].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine Tablets in Patients Over 12 Years of Age With Epilepsya Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
For For Patients NOT TAKING For Patients Patients Carbamazepine, TAKING TAKING Phenytoin, Carbamazepine, Valproatea Phenobarbital, Phenytoin, or Primidoneb, Phenobarbital, or Valproatea or Primidoneb and NOT TAKING Valproatea Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day
(in 2 divided doses) Weeks 5 onwards to
maintenance Increase by 25 to
50 mg/day every 1 to 2 weeks Increase by 50
mg/day every 1
to 2 weeks Increase by
100 mg/day every
1 to 2 weeks. Usual maintenance
dose 100 to 200 mg/day
with valproate alone 225 to 375 mg/day
(in 2 divided doses). 300 to 500 mg/day
(in 2 divided doses). 100 to 400 mg/day
with valproate
and other drugs that induce glucuronidation (in 1 or 2 divided doses)Patients 2 to 12 Years Of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine Tablets in Patients 2 to 12 Years of Age With EpilepsyNote: Only whole tablets should be used for dosing.
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
For Patients TAKING
Valproatea For Patients NOT
TAKING Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea For Patients TAKING
Carbamazepine, Phenytoin, Phenobarbital, or
Primidoneb and NOT
TAKING Valproatea Weeks 1 and 2 0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the
nearest whole tablet (see Table 3 for weight
based dosing guide). 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the
nearest whole tablet. 0.6 mg/kg/day
in 2 divided doses, rounded down to the
nearest whole tablet. Weeks 3 and 4 0.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
(see Table 3 for weight
based dosing guide). 0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet. 1.2 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet. Weeks 5
onwards to
maintenance The dose should be increased every
1 to 2 weeks as follows:
calculate 0.3 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose. The dose should be increased every
1 to 2 weeks as follows:
calculate 0.6 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose The dose should be increased every
1 to 2 weeks as follows:
calculate 1.2 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose Usual
Maintenance
Dose 1 to 5 mg/kg/day
(maximum 200 mg/day
in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day
(maximum 300 mg/day
in 2 divided doses) 5 to 15 mg/kg/day
(maximum 400 mg/day
in 2 divided doses) Maintenance dose in
patients
less than 30 kg May need to be increased
by as much as 50%,
based on clinical response May need to be increased
by as much as 50%,
based on clinical response May need to be increased
by as much as 50%, based
on clinical response Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in two divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets: After achieving a dose of 500 mg/day of lamotrigine tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets:
The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets in Patients ≥16 Years of Age with Epilepsy Lamotrigine Tablets Valproate Step 1 Achieve a dose of 200 mg/day according to
guidelines in Table 1
(if not already on 200 mg/day). Maintain previous stable dose. Step 2 Maintain at 200 mg/day. Decrease to 500 mg/day by decrements no greater than
500 mg/day/week and then maintain the dose of
500 mg/day for 1 week. Step 3 Increase to 300 mg/day and maintain for 1 week. Simultaneously decrease to
250 mg/day and maintain for 1 week. Step 4 Increase by 100 mg/day every
week to achieve maintenance dose of 500 mg/day. Discontinue.Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2) ]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7) , Clinical Pharmacology (12.3) ].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning ].
Table 5. Escalation Regimen for Lamotrigine Tablets for Patients With Bipolar Disordera Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
For Patients TAKING
Valproatea For Patients NOT TAKING
Carbamazepine, Phenytoin, Phenobarbital,
Primidoneb, or Valproatea For Patients TAKING
Carbamazepine, Phenytoin,
Phenobarbital, or Primidoneb and NOT TAKING
Valproatea Weeks 1 and 2 25 mg every
other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to Lamotrigine Tablets for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications Discontinuation of Psychotropic Drugs
(excluding Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea) After Discontinuation of
Valproatea After Discontinuation of
Carbamazepine, Phenytoin,
Phenobarbital, or Primidoneb Current dose of lamotrigine tablets
(mg/day)
100 Current dose of lamotrigine tablets
(mg/day)
400a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Week 1 Maintain current dose of lamotrigine tablets 150 400 Week 2 Maintain current dose of lamotrigine tablets 200 300 Week 3 onward Maintain current dose of lamotrigine tablets 200 200The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine tablets was established in two randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2) ]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Avpak
![Lamotrigine (Lamotrigine) Tablet [Avpak]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Avpak
![Lamotrigine (Lamotrigine) Tablet [Avpak] Lamotrigine (Lamotrigine) Tablet [Avpak]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for Lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation for lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued Lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of Lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine. Drugs that induce glucuronidation include carbamazepine, phenytoin, phenobarbital, primidone, rifampin, estrogen-containing oral contraceptives, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Valproate inhibits glucuronidation. For dosing considerations for Lamotrigine in patients on estrogen-containing contraceptives and atazanavir/ritonavir, see below and Table 13. For dosing considerations for Lamotrigine in patients on other drugs known to induce or inhibit glucuronidation, see Table 1, Table 2, Table 5, Table 6, and Table 13.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of Lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for Lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with Lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of Lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: In women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be increased by as much as 2-fold over the recommended target maintenance dose to maintain a consistent lamotrigine plasma level.
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of Lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (pill-free week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to Lamotrigine consistently occur during the pill-free week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the pill-free week are not recommended. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of Lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: In women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of Lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. In women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of Lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of Lamotrigine in the presence of progestogens alone will likely not be needed.
Patients Taking Atazanavir/Ritonavir: While atazanavir/ritonavir does reduce the lamotrigine plasma concentration, no adjustments to the recommended dose-escalation guidelines for Lamotrigine should be necessary solely based on the use of atazanavir/ritonavir. Dose escalation should follow the recommended guidelines for initiating adjunctive therapy with Lamotrigine based on concomitant AED or other concomitant medications (see Tables 1, 2, and 5). In patients already taking maintenance doses of Lamotrigine and not taking glucuronidation inducers, the dose of Lamotrigine may need to be increased if atazanavir/ritonavir is added, or decreased if atazanavir/ritonavir is discontinued [see Clinical Pharmacology (12.3)].
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 subjects with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of Lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In clinical trials in patients with bipolar disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these patients with bipolar disorder. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients older than 12 years and patients aged 2 to 12 years. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AEDs or other concomitant medications (see Table 1 for patients older than 12 years and Table 2 for patients aged 2 to 12 years). A weight-based dosing guide for patients aged 2 to 12 years on concomitant valproate is provided in Table 3.
Patients Older Than 12 Years: Recommended dosing guidelines are summarized in Table 1.
Table 1 Escalation Regimen for Lamotrigine in Patients Older Than 12 Years With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions ( 7 ), Clinical Pharmacology ( 12.3 )]. † Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)]. In Patients TAKING Valproate* In Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†,or Valproate* In Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day
(in 2 divided doses) Week 5 onward to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks. Increase by 50 mg/day
every 1 to 2 weeks. Increase by 100 mg/day every 1 to 2 weeks. Usual maintenance dose 100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses) 225 to 375 mg/day
(in 2 divided doses) 300 to 500 mg/day (in 2 divided doses)Patients Aged 2 to 12 Years: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients Aged 2 to 12 Years With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)]. In Patients TAKING Valproate* In Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone† or
Valproate* In Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Weeks 1 and 2 0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide) 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide) 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Week 5 onward to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose. The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose. The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose. Usual maintenance dose 1 to 5 mg/kg/day
(maximum 200 mg/day in 1 or 2 divided doses)
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day
(maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response. May need to be increased by as much as 50%, based on clinical response. May need to be increased by as much as 50%, based on clinical response. Note: Only whole tablets should be used for dosing. Table 3. The Initial Weight-Based Dosing Guide for Patients Aged 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive trials in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1- 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to attempt to maintain seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations for lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of lamotrigine using the guidelines in Table 1, the concomitant enzyme-inducing AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves the 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients Aged 16 Years and Older With EpilepsyLamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1.
Maintain established stable dose.
Step 2
Maintain at 200 mg/day.
Decrease dose by decrements no greater than 500 mg/day/week to 500 mg/day and then maintain for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion From Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenytoin, phenobarbital, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitor lopinavir/ritonavir that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine in Patients With Bipolar Disorder * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)]. In Patients TAKING Valproate* In Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate* In Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to Lamotrigine in Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)]. Discontinuation of Psychotropic Drugs (excluding Valproate*Carbamazepine, Phenytoin, Phenobarbital, Primidone†) After Discontinuation of Valproate* After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone† Current dose of lamotrigine (mg/day) 100Current dose of lamotrigine (mg/day) 400
Week 1 Maintain current dose of Lamotrigine 150 400 Week 2 Maintain current dose of Lamotrigine 200 300 Week 3 onward Maintain current dose of Lamotrigine 200 200The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with Lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with Lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Proficient Rx Lp
![Lamotrigine Tablet [Proficient Rx Lp]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Proficient Rx Lp
![Lamotrigine Tablet [Proficient Rx Lp] Lamotrigine Tablet [Proficient Rx Lp]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning ]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablet is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3) ].
Lamotrigine Tablets Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3) ] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3) ].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3) ], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3) ].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3) ]. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6) , Clinical Pharmacology (12.3) ], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7) , Clinical Pharmacology (12.3) ]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.
Discontinuation Strategy:
Epilepsy: For patients receiving lamotrigine tablets in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9) ].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9) ].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine Tablets in Patients Over 12 Years of Age With Epilepsy a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.For
For Patients NOT TAKING
For Patients
Patients
Carbamazepine,
TAKING
TAKING
Phenytoin,
Carbamazepine,
Valproatea
Phenobarbital,
Phenytoin,
or Primidoneb,
Phenobarbital,
or Valproatea
or Primidoneb
and NOT TAKING
Valproatea
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)Weeks 5 onwards to
maintenanceIncrease by 25 to
50 mg/day every 1 to 2 weeksIncrease by 50
mg/day every 1
to 2 weeksIncrease by
100 mg/day every
1 to 2 weeks.Usual maintenance
dose100 to 200 mg/day
with valproate alone225 to 375 mg/day
(in 2 divided doses).300 to 500 mg/day
(in 2 divided doses).100 to 400 mg/day
with valproate
and other drugs that induce glucuronidation(in 1 or 2 divided doses)
Patients 2 to 12 Years Of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine Tablets in Patients 2 to 12 Years of Age With Epilepsy Note: Only whole tablets should be used for dosing. a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.For Patients TAKING
ValproateaFor Patients NOT
TAKING Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
ValproateaFor Patients TAKING
Carbamazepine, Phenytoin, Phenobarbital, or
Primidoneb and NOT
TAKING ValproateaWeeks 1 and 2
0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the
nearest whole tablet (see Table 3 for weight
based dosing guide).0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the
nearest whole tablet.0.6 mg/kg/day
in 2 divided doses, rounded down to the
nearest whole tablet.Weeks 3 and 4
0.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
(see Table 3 for weight
based dosing guide).0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet.1.2 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet.Weeks 5
onwards to
maintenanceThe dose should be increased every
1 to 2 weeks as follows:
calculate 0.3 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose.The dose should be increased every
1 to 2 weeks as follows:
calculate 0.6 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily doseThe dose should be increased every
1 to 2 weeks as follows:
calculate 1.2 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily doseUsual
Maintenance
Dose1 to 5 mg/kg/day
(maximum 200 mg/day
in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone4.5 to 7.5 mg/kg/day
(maximum 300 mg/day
in 2 divided doses)5 to 15 mg/kg/day
(maximum 400 mg/day
in 2 divided doses)Maintenance dose in
patients
less than 30 kgMay need to be increased
by as much as 50%,
based on clinical responseMay need to be increased
by as much as 50%,
based on clinical responseMay need to be increased
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is
by as much as 50%, based
on clinical response
Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in two divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets: After achieving a dose of 500 mg/day of lamotrigine tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets:
The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets in Patients ≥16 Years of Age with EpilepsyLamotrigine Tablets
Valproate
Step 1
Achieve a dose of 200 mg/day according to
guidelines in Table 1
(if not already on 200 mg/day).Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than
500 mg/day/week and then maintain the dose of
500 mg/day for 1 week.Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to
250 mg/day and maintain for 1 week.Step 4
Increase by 100 mg/day every
week to achieve maintenance dose of 500 mg/day.Discontinue.
Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2) ]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7) , Clinical Pharmacology (12.3) ].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning ].
Table 5. Escalation Regimen for Lamotrigine Tablets for Patients With Bipolar Disorder a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.For Patients TAKING
ValproateaFor Patients NOT TAKING
Carbamazepine, Phenytoin, Phenobarbital,
Primidoneb, or ValproateaFor Patients TAKING
Carbamazepine, Phenytoin,
Phenobarbital, or Primidoneb and NOT TAKING
ValproateaWeeks 1 and 2
25 mg every
other day25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
Table 6. Dosage Adjustments to Lamotrigine Tablets for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications Discontinuation of Psychotropic Drugs
(excluding Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea)
After Discontinuation of
Valproatea
After Discontinuation of
Carbamazepine, Phenytoin,
Phenobarbital, or Primidoneb
Current dose of lamotrigine tablets
(mg/day)
100
Current dose of lamotrigine tablets
(mg/day)
400
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.Week 1
Maintain current dose of lamotrigine tablets
150
400
Week 2
Maintain current dose of lamotrigine tablets
200
300
Week 3 onward
Maintain current dose of lamotrigine tablets
200
200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine tablets was established in two randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2) ]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ] Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Dosing is based on concomitant medications, indication, and patient age. ( 2.2 , 2.4 ) To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations should not be exceeded. ( 2.1 ) Do not restart lamotrigine in patients who discontinued due to rash unless the potential benefits clearly outweigh the risks. ( 2.1 ) Adjustments to maintenance doses will in most cases be required in patients starting or stopping estrogen-containing oral contraceptives. ( 2.1 , 5.8 ) Lamotrigine tablets should be discontinued over a period of at least 2 weeks (approximately 50% reduction per week). ( 2.1 , 5.9 )Epilepsy
Adjunctive therapy—See Table 1 for patients >12 years of age and Tables 2 and 3 for patients 2 to 12 years. ( 2.2 ) Conversion to monotherapy—See Table 4. ( 2.3 )Bipolar Disorder: See Tables 5 and 6 ( 2.4 )
Rash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning ]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablet is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3) ].
Lamotrigine Tablets Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3) ] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3) ].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3) ], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3) ].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3) ]. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6) , Clinical Pharmacology (12.3) ], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7) , Clinical Pharmacology (12.3) ]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.
Discontinuation Strategy:
Epilepsy: For patients receiving lamotrigine tablets in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9) ].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9) ].
This section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine Tablets in Patients Over 12 Years of Age With Epilepsy
For
For Patients NOT TAKING
For Patients
Patients
Carbamazepine,
TAKING
TAKING
Phenytoin,
Carbamazepine,
Valproatea
Phenobarbital,
Phenytoin,
or Primidoneb,
Phenobarbital,
or Valproatea
or Primidoneb
and NOT TAKING
Valproatea
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Weeks 5 onwards to
maintenance
Increase by 25 to
50 mg/day every 1 to 2 weeks
Increase by 50
mg/day every 1
to 2 weeks
Increase by
100 mg/day every
1 to 2 weeks.
Usual maintenance
dose
100 to 200 mg/day
with valproate alone
225 to 375 mg/day
(in 2 divided doses).
300 to 500 mg/day
(in 2 divided doses).
100 to 400 mg/day
with valproate
and other drugs that induce glucuronidation
(in 1 or 2 divided doses)
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Patients 2 to 12 Years Of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine Tablets in Patients 2 to 12 Years of Age With Epilepsy
For Patients TAKING
Valproatea
For Patients NOT
TAKING Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea
For Patients TAKING
Carbamazepine, Phenytoin, Phenobarbital, or
Primidoneb and NOT
TAKING Valproatea
Weeks 1 and 2
0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the
nearest whole tablet (see Table 3 for weight
based dosing guide).
0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the
nearest whole tablet.
0.6 mg/kg/day
in 2 divided doses, rounded down to the
nearest whole tablet.
Weeks 3 and 4
0.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
(see Table 3 for weight
based dosing guide).
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet.
1.2 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet.
Weeks 5
onwards to
maintenance
The dose should be increased every
1 to 2 weeks as follows:
calculate 0.3 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose.
The dose should be increased every
1 to 2 weeks as follows:
calculate 0.6 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose
The dose should be increased every
1 to 2 weeks as follows:
calculate 1.2 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose
Usual
Maintenance
Dose
1 to 5 mg/kg/day
(maximum 200 mg/day
in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone
4.5 to 7.5 mg/kg/day
(maximum 300 mg/day
in 2 divided doses)
5 to 15 mg/kg/day
(maximum 400 mg/day
in 2 divided doses)
Maintenance dose in
patients
less than 30 kg
May need to be increased
by as much as 50%,
based on clinical response
May need to be increased
by as much as 50%,
based on clinical response
May need to be increased
by as much as 50%, based
on clinical response
Note: Only whole tablets should be used for dosing.
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is
Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
The goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in two divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets: After achieving a dose of 500 mg/day of lamotrigine tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets:
The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets in Patients ≥16 Years of Age with Epilepsy
Lamotrigine Tablets
Valproate
Step 1
Achieve a dose of 200 mg/day according to
guidelines in Table 1
(if not already on 200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than
500 mg/day/week and then maintain the dose of
500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to
250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every
week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
The goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2) ]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7) , Clinical Pharmacology (12.3) ].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning ].
Table 5. Escalation Regimen for Lamotrigine Tablets for Patients With Bipolar Disorder
For Patients TAKING
Valproatea
For Patients NOT TAKING
Carbamazepine, Phenytoin, Phenobarbital,
Primidoneb, or Valproatea
For Patients TAKING
Carbamazepine, Phenytoin,
Phenobarbital, or Primidoneb and NOT TAKING
Valproatea
Weeks 1 and 2
25 mg every
other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 6. Dosage Adjustments to Lamotrigine Tablets for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications
Discontinuation of Psychotropic Drugs
(excluding Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea)
After Discontinuation of
Valproatea
After Discontinuation of
Carbamazepine, Phenytoin,
Phenobarbital, or Primidoneb
Current dose of lamotrigine tablets
(mg/day)
100
Current dose of lamotrigine tablets
(mg/day)
400
Week 1
Maintain current dose of lamotrigine tablets
150
400
Week 2
Maintain current dose of lamotrigine tablets
200
300
Week 3 onward
Maintain current dose of lamotrigine tablets
200
200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine tablets was established in two randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2) ]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Global Pharmaceuticals, Division Of Impax Laboratories Inc.
![Lamotrigine Tablet, Orally Disintegrating [Global Pharmaceuticals, Division Of Impax Laboratories Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Global Pharmaceuticals, Division Of Impax Laboratories Inc.
![Lamotrigine Tablet, Orally Disintegrating [Global Pharmaceuticals, Division Of Impax Laboratories Inc.] Lamotrigine Tablet, Orally Disintegrating [Global Pharmaceuticals, Division Of Impax Laboratories Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone† or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † These drugs induce glucuronidation and increase clearance [see Drug Interactions (7) Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [See Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day
(in 2 divided doses) Week 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks Usual maintenance dose 100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses) 225 to 375 mg/day
(in 2 divided doses) 300 to 500 mg/day
(in 2 divided doses)Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Note: Only whole tablets should be used for dosing. * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † These drugs induce glucuronidation and increase clearance [see Drug Interactions (7) Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. Weeks 1 and 2 0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide) 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide) 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Week 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual Maintenance Dose 1 to 5 mg/kg/day
(maximum 200 mg/day in 1 or 2 divided doses)
1 to 3 mg/kg/day
with valproate alone 4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day
(maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years of Age Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient's weight is Give this daily dose, using the most appropriate combination of lamotrigine 2-mg and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age with Epilepsy Lamotrigine Valproate Step 1 Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day). Maintain previous stable dose. Step 2 Maintain at 200 mg/day. Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week. Step 3 Increase to 300 mg/day and maintain for 1 week. Simultaneously decrease to 250 mg/day and maintain for 1 week. Step 4 Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day. Discontinue.Conversion From Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see Drug Interactions (7),Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone†, and NOT TAKING Valproate* * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Aministration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications* Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone*, or Valproate†) After Discontinuation of Valproate† After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone* Current dose of Lamotrigine
(mg/day) 100 Current dose of Lamotrigine
(mg/day) 400 * These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Aministration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. † Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Week 1 Maintain current dose of Lamotrigine 150 400 Week 2 Maintain current dose of Lamotrigine 200 300 Week 3 onward Maintain current dose of Lamotrigine 200 200The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
2.6 Administration of Lamotrigine Orally Disintegrating TabletsLamotrigine orally disintegrating tablets should be placed onto the tongue and moved around in the mouth. The tablet will disintegrate rapidly, can be swallowed with or without water, and can be taken with or without food.
-
Direct Rx
![Lamotrigine Tablet [Direct Rx]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Direct Rx
![Lamotrigine Tablet [Direct Rx] Lamotrigine Tablet [Direct Rx]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing Considerations
Rash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning ]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablet is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3) ].
Lamotrigine Tablets Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3) ] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3) ].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3) ], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3) ].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3) ]. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6) , Clinical Pharmacology (12.3) ], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7) , Clinical Pharmacology (12.3) ]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.
Discontinuation Strategy:
Epilepsy: For patients receiving lamotrigine tablets in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9) ].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9) ].
2.2 Epilepsy – Adjunctive Therapy
This section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine Tablets in Patients Over 12 Years of Age With Epilepsya Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
For For Patients NOT TAKING For Patients Patients Carbamazepine, TAKING TAKING Phenytoin, Carbamazepine, Valproatea Phenobarbital, Phenytoin, or Primidoneb, Phenobarbital, or Valproatea or Primidoneb and NOT TAKING Valproatea Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day
(in 2 divided doses) Weeks 5 onwards to
maintenance Increase by 25 to
50 mg/day every 1 to 2 weeks Increase by 50
mg/day every 1
to 2 weeks Increase by
100 mg/day every
1 to 2 weeks. Usual maintenance
dose 100 to 200 mg/day
with valproate alone 225 to 375 mg/day
(in 2 divided doses). 300 to 500 mg/day
(in 2 divided doses). 100 to 400 mg/day
with valproate
and other drugs that induce glucuronidation (in 1 or 2 divided doses)Patients 2 to 12 Years Of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine Tablets in Patients 2 to 12 Years of Age With EpilepsyNote: Only whole tablets should be used for dosing.
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
For Patients TAKING
Valproatea For Patients NOT
TAKING Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea For Patients TAKING
Carbamazepine, Phenytoin, Phenobarbital, or
Primidoneb and NOT
TAKING Valproatea Weeks 1 and 2 0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the
nearest whole tablet (see Table 3 for weight
based dosing guide). 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the
nearest whole tablet. 0.6 mg/kg/day
in 2 divided doses, rounded down to the
nearest whole tablet. Weeks 3 and 4 0.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
(see Table 3 for weight
based dosing guide). 0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet. 1.2 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet. Weeks 5
onwards to
maintenance The dose should be increased every
1 to 2 weeks as follows:
calculate 0.3 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose. The dose should be increased every
1 to 2 weeks as follows:
calculate 0.6 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose The dose should be increased every
1 to 2 weeks as follows:
calculate 1.2 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose Usual
Maintenance
Dose 1 to 5 mg/kg/day
(maximum 200 mg/day
in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day
(maximum 300 mg/day
in 2 divided doses) 5 to 15 mg/kg/day
(maximum 400 mg/day
in 2 divided doses) Maintenance dose in
patients
less than 30 kg May need to be increased
by as much as 50%,
based on clinical response May need to be increased
by as much as 50%,
based on clinical response May need to be increased
by as much as 50%, based
on clinical response Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to Monotherapy
The goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in two divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets: After achieving a dose of 500 mg/day of lamotrigine tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets:
The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets in Patients ≥16 Years of Age with Epilepsy Lamotrigine Tablets Valproate Step 1 Achieve a dose of 200 mg/day according to
guidelines in Table 1
(if not already on 200 mg/day). Maintain previous stable dose. Step 2 Maintain at 200 mg/day. Decrease to 500 mg/day by decrements no greater than
500 mg/day/week and then maintain the dose of
500 mg/day for 1 week. Step 3 Increase to 300 mg/day and maintain for 1 week. Simultaneously decrease to
250 mg/day and maintain for 1 week. Step 4 Increase by 100 mg/day every
week to achieve maintenance dose of 500 mg/day. Discontinue.Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar Disorder
The goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2) ]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7) , Clinical Pharmacology (12.3) ].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning ].
Table 5. Escalation Regimen for Lamotrigine Tablets for Patients With Bipolar Disordera Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
For Patients TAKING
Valproatea For Patients NOT TAKING
Carbamazepine, Phenytoin, Phenobarbital,
Primidoneb, or Valproatea For Patients TAKING
Carbamazepine, Phenytoin,
Phenobarbital, or Primidoneb and NOT TAKING
Valproatea Weeks 1 and 2 25 mg every
other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to Lamotrigine Tablets for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications Discontinuation of Psychotropic Drugs
(excluding Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea) After Discontinuation of
Valproatea After Discontinuation of
Carbamazepine, Phenytoin,
Phenobarbital, or Primidoneb Current dose of lamotrigine tablets
(mg/day)
100 Current dose of lamotrigine tablets
(mg/day)
400a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Week 1 Maintain current dose of lamotrigine tablets 150 400 Week 2 Maintain current dose of lamotrigine tablets 200 300 Week 3 onward Maintain current dose of lamotrigine tablets 200 200The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine tablets was established in two randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2) ]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
State Of Florida Doh Central Pharmacy
![Lamotrigine Tablet [State Of Florida Doh Central Pharmacy]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | State Of Florida Doh Central Pharmacy
![Lamotrigine Tablet [State Of Florida Doh Central Pharmacy] Lamotrigine Tablet [State Of Florida Doh Central Pharmacy]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning ]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablet is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3) ].
Lamotrigine Tablets Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3) ] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3) ].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3) ], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3) ].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3) ]. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6) , Clinical Pharmacology (12.3) ], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7) , Clinical Pharmacology (12.3) ]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.
Discontinuation Strategy:
Epilepsy: For patients receiving lamotrigine tablets in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9) ].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9) ].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine Tablets in Patients Over 12 Years of Age With Epilepsya Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
For
For Patients NOT TAKING
For Patients
Patients
Carbamazepine,
TAKING
TAKING
Phenytoin,
Carbamazepine,
Valproatea
Phenobarbital,
Phenytoin,
or Primidoneb,
Phenobarbital,
or Valproatea
or Primidoneb
and NOT TAKING
Valproatea
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Weeks 5 onwards to
maintenance
Increase by 25 to
50 mg/day every 1 to 2 weeks
Increase by 50
mg/day every 1
to 2 weeks
Increase by
100 mg/day every
1 to 2 weeks.
Usual maintenance
dose
100 to 200 mg/day
with valproate alone
225 to 375 mg/day
(in 2 divided doses).
300 to 500 mg/day
(in 2 divided doses).
100 to 400 mg/day
with valproate
and other drugs that induce glucuronidation
(in 1 or 2 divided doses)
Patients 2 to 12 Years Of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine Tablets in Patients 2 to 12 Years of Age With EpilepsyNote: Only whole tablets should be used for dosing.
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
For Patients TAKING
Valproatea
For Patients NOT
TAKING Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea
For Patients TAKING
Carbamazepine, Phenytoin, Phenobarbital, or
Primidoneb and NOT
TAKING Valproatea
Weeks 1 and 2
0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the
nearest whole tablet (see Table 3 for weight
based dosing guide).
0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the
nearest whole tablet.
0.6 mg/kg/day
in 2 divided doses, rounded down to the
nearest whole tablet.
Weeks 3 and 4
0.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
(see Table 3 for weight
based dosing guide).
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet.
1.2 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet.
Weeks 5
onwards to
maintenance
The dose should be increased every
1 to 2 weeks as follows:
calculate 0.3 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose.
The dose should be increased every
1 to 2 weeks as follows:
calculate 0.6 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose
The dose should be increased every
1 to 2 weeks as follows:
calculate 1.2 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose
Usual
Maintenance
Dose
1 to 5 mg/kg/day
(maximum 200 mg/day
in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone
4.5 to 7.5 mg/kg/day
(maximum 300 mg/day
in 2 divided doses)
5 to 15 mg/kg/day
(maximum 400 mg/day
in 2 divided doses)
Maintenance dose in
patients
less than 30 kg
May need to be increased
by as much as 50%,
based on clinical response
May need to be increased
by as much as 50%,
based on clinical response
May need to be increased
by as much as 50%, based
on clinical response
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is
Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in two divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets: After achieving a dose of 500 mg/day of lamotrigine tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets:
The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets in Patients ≥16 Years of Age with Epilepsy
Lamotrigine Tablets
Valproate
Step 1
Achieve a dose of 200 mg/day according to
guidelines in Table 1
(if not already on 200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than
500 mg/day/week and then maintain the dose of
500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to
250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every
week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2) ]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7) , Clinical Pharmacology (12.3) ].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning ].
Table 5. Escalation Regimen for Lamotrigine Tablets for Patients With Bipolar Disordera Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
For Patients TAKING
Valproatea
For Patients NOT TAKING
Carbamazepine, Phenytoin, Phenobarbital,
Primidoneb, or Valproatea
For Patients TAKING
Carbamazepine, Phenytoin,
Phenobarbital, or Primidoneb and NOT TAKING
Valproatea
Weeks 1 and 2
25 mg every
other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
Table 6. Dosage Adjustments to Lamotrigine Tablets for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications
Discontinuation of Psychotropic Drugs
(excluding Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea)
After Discontinuation of
Valproatea
After Discontinuation of
Carbamazepine, Phenytoin,
Phenobarbital, or Primidoneb
Current dose of lamotrigine tablets
(mg/day)
100
Current dose of lamotrigine tablets
(mg/day)
400
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Week 1
Maintain current dose of lamotrigine tablets
150
400
Week 2
Maintain current dose of lamotrigine tablets
200
300
Week 3 onward
Maintain current dose of lamotrigine tablets
200
200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine tablets was established in two randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2) ]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
State Of Florida Doh Central Pharmacy
![Lamotrigine (Lamotrigine ) Tablet [State Of Florida Doh Central Pharmacy]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | State Of Florida Doh Central Pharmacy
![Lamotrigine (Lamotrigine ) Tablet [State Of Florida Doh Central Pharmacy] Lamotrigine (Lamotrigine ) Tablet [State Of Florida Doh Central Pharmacy]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
Lamotrigine Starter Kits provide lamotrigine at doses consistent with the recommended titration schedule for the first 5 weeks of treatment, based upon concomitant medications for patients with epilepsy (>12 years of age) and Bipolar I Disorder (≥18 years of age) and are intended to help reduce the potential for rash. The use of lamotrigine Starter Kits is recommended for appropriate patients who are starting or restarting lamotrigine [see How Supplied/Storage and Handling (16)].
It is recommended that lamotrigine tablets, USP not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsya Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
For Patients TAKING
Valproatea
For Patients NOT
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital,
Primidoneb, or
Valproatea
For Patients
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidoneb and
NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Week 5
onwards to
maintenance
Increase by 25 to 50
mg/day every 1 to
2 weeks
Increase by 50
mg/day every 1 to
2 weeks
Increase by 100
mg/day every 1 to
2 weeks.
Usual
Maintenance
Dose
100 to 200 mg/day
with valproate
alone
100 to 400 mg/day
with valproate and
other drugs that
induce
glucuronidation
(in 1 or 2 divided
doses)
225 to 375 mg/day
(in 2 divided doses)
300 to 500 mg/day
(in 2 divided doses)
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
The smallest available strength of lamotrigine tablets is 25 mg, and only whole tablets should be administered. If the calculated dose cannot be achieved using whole tablets, the dose should be rounded down to the nearest whole tablet [see How Supplied/Storage and Handling (16) and Medication Guide].
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With EpilepsyNote: Only whole tablets should be used for dosing.
aValproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7),
Clinical Pharmacology (12.3)].bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)].
Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see
Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
For Patients
TAKING Valproatea
For Patients NOT
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital,
Primidoneb, or
Valproatea
For Patients TAKING
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidoneb and NOT
TAKING Valproatea
Weeks 1
and 2
0.15 mg/kg/day
in 1 or 2 divided
doses, rounded
down to the nearest
whole tablet (see
Table 3 for weight-based dosing guide)
0.3 mg/kg/day
in 1 or 2 divided
doses, rounded down
to the nearest whole
tablet
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
Weeks 3
and 4
0.3 mg/kg/day
in 1 or 2 divided
doses, rounded
down to the nearest
whole tablet (see
Table 3 for weight-based dosing guide)
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
1.2 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
Week 5
onwards to
maintenance
The dose should be
increased every 1 to
2 weeks as follows:
calculate 0.3 mg/kg/day,
round this amount
down to the nearest
whole tablet, and
add this amount to
the previously
administered daily
dose
The dose should be increased every 1 to
2 weeks as follows: calculate
0.6 mg/kg/day, round
this amount down to
the nearest whole
tablet, and add this
amount to the
previously
administered daily
dose
The dose should be increased every 1 to
2 weeks as follows: calculate
1.2 mg/kg/day, round
this amount down to
the nearest whole
tablet, and add this
amount to the
previously
administered daily
dose
Usual
Maintenance
Dose
1 to 5 mg/kg/day
(maximum
200 mg/day in 1 or 2
divided doses).
1 to 3 mg/kg/day
with valproate alone
4.5 to 7.5 mg/kg/day
(maximum 300
mg/day in 2 divided
doses)
5 to 15 mg/kg/day
(maximum 400
mg/day in 2 divided
doses)
Maintenance
dose in
patients less
than 30 kg
May need to be
increased by as
much as 50%, based
on clinical response
May need to be
increased by as much
as 50%, based on
clinical response
May need to be
increased by as much
as 50%, based on
clinical response
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years of Age Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is
Give this daily dose, using the most appropriate combination of lamotrigine
2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age With Epilepsy
Lamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to
guidelines in Table 1 (if not already on
200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by
decrements no greater than
500 mg/day/week and then
maintain the dose of
500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1
week.
Simultaneously decrease to
250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve
maintenance dose of 500 mg/day.
Discontinue.
Conversion From Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disordera Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
For Patients TAKING Valproatea
For Patients NOT TAKING
Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea
For Patients TAKING
Carbamazepine, Phenytoin, Phenobarbital,
or Primidoneb and
NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in
divided doses
Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medicationsa Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Discontinuation of Psychotropic Drugs
(excluding Carbamazepine, Phenytoin,
After Discontinuation of Valproatea
After Discontinuation of Carbamazepine,
Phenytoin, Phenobarbital,or
Primidoneb
Phenobarbital, Primidoneb, or Valproatea)
Current dose of Lamotrigine (mg/day)
100
Current dose of Lamotrigine (mg/day)
400
Week 1
Maintain current dose of Lamotrigine
150
400
Week 2
Maintain current dose of Lamotrigine
200
300
Week 3 onward
Maintain current dose of Lamotrigine
200
200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
State Of Florida Doh Central Pharmacy
![Lamotrigine Tablet [State Of Florida Doh Central Pharmacy]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | State Of Florida Doh Central Pharmacy
![Lamotrigine Tablet [State Of Florida Doh Central Pharmacy] Lamotrigine Tablet [State Of Florida Doh Central Pharmacy]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
Lamotrigine Starter Kits provide lamotrigine at doses consistent with the recommended titration schedule for the first 5 weeks of treatment, based upon concomitant medications for patients with epilepsy (>12 years of age) and Bipolar I Disorder (≥18 years of age) and are intended to help reduce the potential for rash. The use of Lamotrigine Starter Kits is recommended for appropriate patients who are starting or restarting lamotrigine [see How Supplied/Storage and Handling (16)].
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy For Patients TAKING Valproate * For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day
(in 2 divided doses) Week 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks Usual maintenance dose 100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses) 225 to 375 mg/day
(in 2 divided doses) 300 to 500 mg/day
(in 2 divided doses)Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy For Patients TAKING Valproate * For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Note: Only whole tablets should be used for dosing. * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Weeks 1 and 2 0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Week 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual maintenance dose 1 to 5 mg/kg/day
(maximum 200 mg/day in 1 or 2 divided doses)
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day
(maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical responseDosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years of Age Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient's weight is Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age With Epilepsy Lamotrigine Valproate Step 1 Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day). Maintain previous stable dose. Step 2 Maintain at 200 mg/day. Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week. Step 3 Increase to 300 mg/day and maintain for 1 week. Simultaneously decrease to 250 mg/day and maintain for 1 week. Step 4 Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day. Discontinue.Conversion From Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone†, and NOT TAKING Valproate* * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone*, or Valproate†) After Discontinuation of Valproate† After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital or Primidone* Current dose of Lamotrigine (mg/day) 100 Current dose of Lamotrigine (mg/day) 400 * These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. † Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Week 1 Maintain current dose of Lamotrigine 150 400 Week 2 Maintain current dose of Lamotrigine 200 300 Week 3 onward Maintain current dose of Lamotrigine 200 200The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Sandoz Inc
![Lamotrigine Tablet Lamotrigine Kit [Sandoz Inc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Sandoz Inc
![Lamotrigine Tablet Lamotrigine Kit [Sandoz Inc] Lamotrigine Tablet Lamotrigine Kit [Sandoz Inc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
Lamotrigine Tablet Starter Kits provide lamotrigine at doses consistent with the recommended titration schedule for the first 5 weeks of treatment, based upon concomitant medications for patients with epilepsy (>12 years of age) and Bipolar I Disorder (≥18 years of age) and are intended to help reduce the potential for rash. The use of lamotrigine Starter Kits is recommended for appropriate patients who are starting or restarting lamotrigine [see How Supplied/Storage and Handling (16 ).
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives:Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine In Women Taking Estrogen-Containing Oral Contraceptives:
Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)]. Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment should be necessary to the dose of lamotrigine. Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment to the dose of lamotrigine should be necessary.Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations ( 8.7), Clinical Pharmacology (12.3 )]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy:Epilepsy: For patients receiving lamotrigine in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, or primidone should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy - Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Epilepsy Regimen for Lamotrigine in Patients Over 12 Years of Age WithFor Patients Taking
Valproate *For Patients Taking
AEDs Other Than
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidone†, and Not
Taking ValproateFor Patients Taking
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidone† and Not
Taking Valproate Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day100 mg/day
(in 2 divided doses)Weeks 5 onwards
to maintenanceIncrease by 25 to
50 mg/day every 1 to
2 weeksIncrease by 50 mg/day
every 1 to 2 weeksIncrease by
100 mg/day every 1 to
2 weeks.Usual
Maintenance
Dose100 to 200 mg/day
with valproate alone
100 to 400 mg/day with
valproate and other
drugs that induce
glucuronication
(in 1 or 2 divided doses)225 to 375 mg/day
(in 2 divided doses)300 to 500 mg/day
(in 2 divided doses)* Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Pharmacokinetics (12.3)].
† These drugs induce glucuronidation and increase clearance [see Drug Interactions (7),
Pharmacokinetics (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives and rifampin [see Drug Interactions (7), Pharmacokinetics 12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin should follow the same dosing titration/maintenance regimen used with drugs that induce glucuronidation and increase clearance.
Patients 2 to 12 Years of Age:Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for LAMOTRIGINE in Patients 2 to 12 Years of Age With Epilepsy
For Patients Taking
Valproate *For Patients Taking
AEDs Other Than
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidone†, and Not
Taking ValproateFor Patients Taking
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidone† and Not
Taking Valproate Weeks 1 and 20.15 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
(see Table 3 for weight
based dosing guide)0.3mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet0.6mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet Weeks 3 and 40.3mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
(see Table 3 for weight
based dosing guide)0.6mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet1.2mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tabletWeeks 5
onwards to
maintenanceThe dose should be
increased every 1 to
2 weeks as follows:
calculate
0.3 mg/kg/day, round
this amount down to
the nearest whole
tablet, and add this
amount to the
previously
administered daily doseThe dose should be
increased every 1 to
2 weeks as follows:
calculate 0.6 mg/kg/day,
round this amount down
to the nearest whole
tablet, and add this
amount to the previously
administered daily doseThe dose should be
increased every 1 to
2 weeks as follows:
calculate 1.2 mg/kg/day,
round this amount down
to the nearest whole
tablet, and add this
amount to the previously
administered daily doseUsual
Maintenance
Dose1 to 5mg/kg/day
(maximum
200 mg/day in 1 or
2 divided doses).
1 to 3mg/kg/day with
valproate alone4.5 to 7.5mg/kg/day
(maximum 300 mg/day
in 2 divided doses)5 to 15mg/kg/day
(maximum 400 mg/day
in 2 divided doses)Maintenance
dose in
patients less
than 30 kgMay need to be
increased by as much
as 50%, based on
clinical responseMay need to be increased
by as much as 50%,
based on clinical
responseMay need to be
increased by as much as
50%, based on clinical
responseNote: Only whole tablets should be used for dosing.
* Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Pharmacokinetics (12.3)].
† These drugs induce glucuronidation and increase clearance [see Drug Interactions (7),
Pharmacokinetics (12.3)]. Other drugs which have similar effects include estrogen-containing
oral contraceptives and rifampin [see Drug Interactions (7), Pharmacokinetics (12.3)].
Dosing recommendations for oral contraceptives can be found in General Dosing
Considerations [see Dosage and Administration (2.1)]. Patients on rifampin should follow the
same dosing titration/maintenance regimen used with drugs that induce glucuronidation and
increase clearance.Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy
If the patient's weight is Give this daily dose, using the most appropriate combination of LAMOTRIGINE 2-mg and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy - Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine:After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine:The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age with Epilepsy
Lamotrigine Valproate Step 1 Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day). Maintain previous stable dose. Step 2 Maintain at 200 mg/day. Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week. Step 3 Increase to 300 mg/day and maintain for 1 week.Simultaneously decrease to 250 mg/day and maintain for
1 week. Step 4 Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day. Discontinue.Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine:No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, which increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder*
For Patients Taking Valproate‡ For Patients Not Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Rifampin† and Not Taking Valproate‡ For Patients Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Rifampin† and Not Taking Valproate‡ Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses* See Drug Interactions (7) and Clinical Pharmacology (12.3) for a description of known drug interactions.
† Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine.
‡ Valproate has been shown to decrease the apparent clearance of lamotrigine.
Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications*
Discontinuation of
Psychotropic Drugs
(excluding
Carbamazepine,
Phenytoin,
Phenobarbital,
Primidone, Rifampin†, or
Valproate‡)After Discontinuation
of Valproate‡
After Discontinuation of
Carbamazepine,
Phenytoin,
Phenobarbital,
Primidone, or Rifampin†
Current dose of
lamotrigine (mg/day)
100Current dose of
lamotrigine (mg/day)
400 Week1Maintain current dose of
lamotrigine 150 400 Week 2Maintain current dose of
lamotrigine 200 300Week 3
onwardMaintain current dose of
lamotrigine 200 200* See Drug Interactions (7) and Clinical Pharmacology (12.3) for a description of known dru interactions.
† Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to
increase the apparent clearance of lamotrigine.‡ Valproate has been shown to decrease the apparent clearance of lamotrigine.
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Mckesson Packaging Services Business Unit Of Mckesson Corporation
![Lamotrigine Tablet [Mckesson Packaging Services Business Unit Of Mckesson Corporation]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Mckesson Packaging Services Business Unit Of Mckesson Corporation
![Lamotrigine Tablet [Mckesson Packaging Services Business Unit Of Mckesson Corporation] Lamotrigine Tablet [Mckesson Packaging Services Business Unit Of Mckesson Corporation]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Epilepsy: Adjunctive Use:Lamotrigine tablets are indicated as adjunctive therapy for partial seizures and the generalized seizures of Lennox-Gastaut syndrome in adult and pediatric patients (≥ 2 years of age).
Monotherapy Use:Lamotrigine tablets are indicated for conversion to monotherapy in adults with partial seizures who are receiving treatment with carbamazepine, phenytoin, phenobarbital, primidone, or valproate as the single AED.
Safety and effectiveness of lamotrigine tablets have not been established (1) as initial monotherapy, (2) for conversion to monotherapy from AEDs other than carbamazepine, phenytoin, phenobarbital, primidone, or valproate, or (3) for simultaneous conversion to monotherapy from 2 or more concomitant AEDs.
Bipolar Disorder:Lamotrigine tablets are indicated for the maintenance treatment of Bipolar I Disorder to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The effectiveness of lamotrigine tablets in the acute treatment of mood episodes has not been established.
General Dosing Considerations for Epilepsy and Bipolar Disorder Patients:The risk of nonserious rash is increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablets is exceeded. There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have been reported in the absence of these factors (see BOX WARNING). Therefore, it is important that the dosing recommendations be followed closely.
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 halflives, it is recommended that initial dosing recommendations and guidelines be followed.
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation:Drugs other than those listed in PRECAUTIONS: Drug Interactionshave not been systematically evaluated in combination with lamotrigine. Since lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine, and doses of lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder:A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response.
The half-life of lamotrigine is affected by other concomitant medications (see CLINICAL PHARMACOLOGY: Pharmacokinetics and Drug Metabolism).
See also DOSAGE AND ADMINISTRATION: Special Populations.
Special Populations: Women and Oral Contraceptives: Starting Lamotrigine in Women Taking Oral Contraceptives:Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine (see PRECAUTIONS: Drug Interactions), no adjustments to the recommended dose escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED (see Table 11). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine:(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dosein order to maintain a consistent lamotrigine plasma level (see PRECAUTIONS: Drug Interactions). (2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose will in most cases need to be increased by as much as 2-fold, in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate unless lamotrigineplasma levels or clinical response support larger increases (see Table 11, column 2).Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse events, such as dizziness, ataxia, and diplopia (see PRECAUTIONS: Drug Interactions). If adverse events attributable to lamotrigine consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment should be necessary to the dose of lamotrigine. (3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50%, in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise (see PRECAUTIONS: Drug Interactions). For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy:The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment:Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver dysfunction (see CLINICAL PHARMACOLOGY), the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Functional Impairment:Initial doses of lamotrigine should be based on patients’ AED regimen (see above); reduced maintenance doses may be effective for patients with significant renal functional impairment (see CLINICAL PHARMACOLOGY). Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Epilepsy: Adjunctive Therapy With Lamotrigine for Epilepsy:This section provides specific dosing recommendations for patients 2 to 12 years of age and patients greater than 12 years of age. Within each of these age groups, specific dosing recommendations are provided depending upon concomitant AED (Table 9 for patients 2 to 12 years of age and Table 11 for patients greater than 12 years of age). A weight based dosing guide for pediatric patients on concomitant valproate is provided in Table 10.
Patients 2 to 12 Years of Age:Recommended dosing guidelines are summarized in Table 9. Note that some of the starting doses and dose escalations listed in Table 9 are different than those used in clinical trials; however, the maintenance doses are the same as in clinical trials. Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestions that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 9. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy Note: Only whole tablets should be used for dosing * Rifampin and estrogen-containing contraceptives have also been shown to increase the apparent clearance of lamotrigine (see PRECAUTIONS: Drug Interactions).For Patients Taking
Valproate (see Table 10 for
weight-based dosing guide)For Patients Taking AEDs
Other Than Carbamazepine,
Phenytoin, Phenobarbital,
Primidone or Valproate*For Patients Taking
Carbamazepine, Phenytoin,
Phenobarbital, Primidone*
and Not Taking ValproateWeeks 1 and 2
0.15 mg/kg/day in 1 or 2
divided doses, rounded
down to the nearest whole
tablet (see Table 10 for
weight-based dosing guide).0.3 mg/kg/day in 1 or
2 divided doses, rounded down to the nearest
whole tablet.0.6 mg/kg/day in 2 divided
doses, rounded down to the
nearest whole tablet.Weeks 3 and 4
0.3 mg/kg/day in 1 or
2 divided doses, rounded
down to the nearest whole
tablet (see Table 10 for
weight-based dosing guide).0.6 mg/kg/day in 2 divided
doses, rounded down to the
nearest whole tablet.1.2 mg/kg/day in 2 divided doses,
rounded down to the
nearest whole tablet.Weeks 5 onwards to
maintenanceThe dose should be increased
every 1 to 2 weeks as follows:
calculate 0.3 mg/kg/day,
round this amount down to the nearest whole tablet, and add
this amount to the previously
administered daily dose.The dose should be increased
every 1 to 2 weeks as follows:
calculate 0.6 mg/kg/day,
round this amount down to the nearest whole tablet,
and add this amount to the
previously administered daily doseThe dose should be increased
every 1 to 2 weeks as follows:
calculate 1.2 mg/kg/day,
round this amount down to
the nearest whole tablet, and
add this amount to the previously administered daily
doseUsual Maintenance
Dose1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in
2 divided doses)5 to 15 mg/kg/day
(maximum 400 mg/day in
2 divided doses)Maintenance dose in patients less than
30 kgMay need to be increased by as
much as 50%, based on clinical
responseMay need to be increased by as
much as 50%, based on
clinical responseMay need to be increased by as
Table 10. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy
much as 50%, based on
clinical responseIf the patient’s weight is
Give this daily dose, using the most appropriate
combination of lamotrigine 2-mg and 5-mg tabletsGreater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Patients Over 12 Years of Age:Recommended dosing guidelines are summarized in Table 11
Table 11. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy * Rifampin and estrogen-containing oral contraceptives have also been shown to increase the apparent clearance of lamotrigine (see PRECAUTIONS: Drug Interactions)For Patients Taking Valproate
For Patients Taking AEDs
Other Than Carbamazepine,
Phenytoin, Phenobarbital,
Primidone or Valproate*For Patients Taking
Carbamazepine, Phenytoin,
Phenobarbital, Primidone*
and Not Taking ValproateWeeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Weeks 5 onwards to
maintenanceIncrease by 25 to 50 mg/day every
1 to 2 weeksIncrease by 50 mg/day
every 1 to 2 weeksIncrease by 100 mg/day
every 1 to 2 weeks.Usual Maintenance
Dose100 to 400 mg/day
(1 or 2 divided doses) 100 to
200 mg/daywith valproate alone225 to 375 mg/day
(in 2 divided doses).300 to 500 mg/day
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate as the Single AED to Monotherapy With Lamotrigine in Patients ≥ 16 Years of Age With Epilepsy:
(in 2 divided doses).The goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded (see BOX WARNING).
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine:After achieving a dose of 500 mg/day of lamotrigine according to Table 11, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine:The conversion regimen involves 4 steps. (see Table 12).
Table 12. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age With EpilepsyLamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to
guidelines in Table 11 (if not already on
200 mg/day).Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements
no greater than 500 mg/day per week
and then maintain the dose of
500 mg/day for 1 week.Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day
and maintain for 1 week.Step 4
Increase by 100 mg/day every week to achieve
maintenance dose of 500 mg/day.Discontinue.
Conversion From Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine:No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
Usual Maintenance Dose for Epilepsy:The usual maintenance doses identified in Tables 9 -11 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/ day have been used. The advantage of using doses above those recommended in the Tables 9 -12 has not been established in controlled trials.
Discontinuation Strategy for Patients With Epilepsy:For patients receiving lamotrigine in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse experiences is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal (see PRECAUTIONS).
Discontinuing carbamazepine, phenytoin, phenobarbital, or primidone should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder:The goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, which increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated, however, no additional benefit was seen at 400 mg/day compared to 200 mg/day (see CLINICAL STUDIES: Bipolar Disorder). Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 13. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2 week period in equal weekly increments (see Table 14). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2 week period in equal weekly decrements (see Table 14). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
Dosage adjustments will be necessary in most patients who start or stop estrogen-containing oral contraceptives while taking lamotrigine (see DOSAGE AND ADMINISTRATION, Special Populations, Women and oral contraceptives, Adjustments to the maintenance dose of lamotrigine).
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets (see CLINICAL PHARMACOLOGY: Drug Interactions).
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded (see BOX WARNING).
Table 13. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder* * See CLINICAL PHARMACOLOGY, Drug Interactions and PRECAUTIONS, Drug Interactions for a description of known drug interactions. † Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine. ‡ Valproate has been shown to decrease the apparent clearance of lamotrigine. For Patients Not Taking
Carbamazepine, (or Other Enzyme-
Inducing Drugs†) or Valproate‡For Patients Taking
Valproate‡For Patients Taking Carbamazepine
(or Other Enzyme-Inducing Drugs)
and Not Taking Valproate‡Weeks 1 and 2
25 mg daily
25 mg every other day
50 mg daily
Weeks 3 and 4
50 mg daily
25 mg daily
100 mg daily, in divided doses
Week 5
100 mg daily
50 mg daily
200 mg daily, in divided doses
Week 6
200 mg daily
100 mg daily
300 mg daily, in divided doses
Week 7
200 mg daily
100 mg daily
up to 400 mg daily, in divided doses
Table 14. Adjustments to Lamotrigine Dosing for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications* * See CLINICAL PHARMACOLOGY, Drug Interactionsand PRECAUTIONS, Drug Interactions for a description of known drug interactions † Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine. ‡ Valproate has been shown to decrease the apparent clearance of lamotrigine.Discontinuation of
Psychotropic Drugs
(excluding Carbamazepine, or Other Enzyme-Inducing Drugs)†After Discontinuation of
Valproate‡After Discontinuation of
Carbamazepine, or Other
Enzyme-Inducing Drugs†Current lamotrigine dose (mg/day) 100
Current lamotrigine dose
(mg/day) 400Week 1
Maintain current
Lamotrigine dose150
400
Week 2
Maintain current
Lamotrigine dose200
300
Week 3 onward
Maintain current
Lamotrigine dose200
200
There is no body of evidence available to answer the question of how long the patient should remain on lamotrigine tablet therapy. Systematic evaluation of the efficacy of lamotrigine in patients with either depression or mania who responded to standard therapy during an acute 8 to 16 week treatment phase and were then randomized to lamotrigine or placebo for up to 76 weeks of observation for affective relapse demonstrated a benefit of such maintenance treatment (see CLINICAL STUDIES: Bipolar Disorder). Nevertheless, patients should be periodically reassessed to determine the need for maintenance treatment.
Discontinuation Strategy in Bipolar Disorder:As with other AEDs, lamotrigine tablets should not be abruptly discontinued. In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse experiences following abrupt termination of lamotrigine. In clinical trials in patients with bipolar disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal.
-
Mckesson Packaging Services A Buisness Unit Of Mckesson Corporation
![Lamotrigine Tablet [Mckesson Packaging Services A Buisness Unit Of Mckesson Corporation]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Mckesson Packaging Services A Buisness Unit Of Mckesson Corporation
![Lamotrigine Tablet [Mckesson Packaging Services A Buisness Unit Of Mckesson Corporation] Lamotrigine Tablet [Mckesson Packaging Services A Buisness Unit Of Mckesson Corporation]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1. General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablets is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine tablets Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets In Women Taking Estrogen-Containing Oral Contraceptives:
Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)]. Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold, in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary. Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50%, in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)],
the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.
Discontinuation Strategy:Epilepsy: For patients receiving lamotrigine tablets in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.10)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder:
In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.10)].
2.2. Epilepsy - Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age:
Recommended dosing guidelines are summarized in Table 1.
Table 1Escalation Regimen for Lamotrigine Tablets in Patients Over 12 Years of Age With Epilepsy
For Patients TAKING Valproatea
For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidoneb, or Valproatea
For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Week 5 onwards to maintenance
Increase by 25 to 50 mg/day every 1 to 2 weeks
Increase by 50 mg/day every 1 to 2 weeks
Increase by 100 mg/day every 1 to 2 weeks.
Usual Maintenance Dose
100 to 200 mg/day with valproate alone
100 to 400 mg/day
with valproate and other drugs that induce glucuronication
( in 1 or 2 divided doses)
225 to 375 mg/day
(in 2 divided doses).
300 to 500 mg/day
(in 2 divided doses).
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7) Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestions that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2Escalation Regimen for Lamotrigine Tablets in Patients 2 to 12 Years of Age With Epilepsy
For Patients TAKING Valproatea
For Patients
NOT TAKING Carbamazepine,
Phenytoin,
Phenobarbital,
Primidoneb, or Valproatea
For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea
Weeks 1 and 2
0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide).
0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet.
0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet.
Weeks 3 and 4
0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide).
0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet.
1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet.
Week 5 onwards to maintenance
The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose.
The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
Usual Maintenance Dose
1 to 5 mg/kg/day(maximum 200 mg/day in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone
4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses)
5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses)
Maintenance dose in patients less than 30 kg
May need to be increased by as much as 50%, based on clinical response
May need to be increased by as much as 50%, based on clinical response
May need to be increased by as much as 50%, based on clinical response
Note: Only whole tablets should be used for dosing
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7) Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)].
Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)].
Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 3The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy
If the patient’s weight is
Give this daily dose, using the most appropriate combination of lamotrigine tablets 2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Maintenance Dose for Epilepsy:
The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3. Epilepsy - Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablet under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablet.
The recommended maintenance dose of lamotrigine tablet as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy with Lamotrigine Tablets: After achieving a dose of 500 mg/day of lamotrigine tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy with Valproate to Monotherapy with Lamotrigine Tablets: The conversion regimen involves 4 steps outline in Table 4.
Table 4Conversion From Adjunctive Therapy with Valproate to Monotherapy with Lamotrigine Tablets in Patients ≥16 Years of Age with Epilepsy
Lamotrigine Tablets
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than 500 mg/day per week and then maintain the dose of 500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4. Bipolar DisorderThe goal of maintenance treatment with lamotrigine tablet is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucoronidation, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablet may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablet [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Table 5 Escalation Regimen for Lamotrigine Tablets for Patients with Bipolar Disorder
For Patients TAKING Valproatea
For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidoneb, or Valproatea
For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 6Dosage Adjustments to Lamotrigine Tablets for Patients with Bipolar Disorder Following Discontinuation of Psychotropic Medications
Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidoneb, or Valproatea)
After Discontinuation of Valproatea
After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb
Current dose of Lamotrigine Tablets (mg/day) 100
Current dose of Lamotrigine Tablets (mg/day) 400
Week 1
Maintain current dose of Lamotrigine Tablets
150
400
Week 2
Maintain current dose of Lamotrigine Tablets
200
300
Week 3 onward
Maintain current dose of Lamotrigine Tablets
200
200
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine tablets was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Stat Rx Usa Llc
![Lamotrigine Tablet [Stat Rx Usa Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Stat Rx Usa Llc
![Lamotrigine Tablet [Stat Rx Usa Llc] Lamotrigine Tablet [Stat Rx Usa Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablets is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be increased, by as much as 2 fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2 fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (seeTable 1 orTable 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2 week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2 fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1to3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine tablets in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.10)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.10)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ see Drug Interactions (7), Clinical Pharmacology (12.3)] . † These drugs induce lamotrigine glucuronidation and increase clearance [ see Drug Interactions (7) Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [ see Drug Interactions (7), Clinical Pharmacology (12.3)] . Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [ see Dosage and Administration (2.1)] . Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,† or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day (in 2 divided doses) Week 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks Usual Maintenance Dose100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses)
225 to 375 mg/day (in 2 divided doses)300 to 500 mg/day
(in 2 divided doses)
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ see Drug Interactions (7), Clinical Pharmacology (12.3)] . † These drugs induce lamotrigine glucuronidation and increase clearance [ see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [ see Drug Interactions (7), Clinical Pharmacology (12.3)] . Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [ see Dosage and Administration (2.1)] . Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,† or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Weeks 1 and 2 0.15 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet Week 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual Maintenance Dose 1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day (maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical responseNote: Only whole tablets should be used for dosing.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of lamotrigine tablets, 2 mg and 5 mg Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets: After achieving a dose of 500 mg/day of lamotrigine tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4 week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥ 16 Years of Age With Epilepsy Lamotrigine Valproate Step 1 Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day). Maintain previous stable dose. Step 2 Maintain at 200 mg/day. Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week. Step 3 Increase to 300 mg/day and maintain for 1 week. Simultaneously decrease to 250 mg/day and maintain for 1 week. Step 4 Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day. Discontinue.Conversion From Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2 week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2 week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ see Drug Interactions (7), Clinical Pharmacology (12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [ see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [ see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [ see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,† or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications * These drugs induce lamotrigine glucuronidation and increase clearance [ see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [ see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [ see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. † Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ see Drug Interactions (7), Clinical Pharmacology (12.3)]. Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone,* or Valproate†) After Discontinuation of Valproate† After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone* Current dose of Lamotrigine (mg/day) 100Current dose of Lamotrigine (mg/day)
400
Week 1 Maintain current dose of lamotrigine 150 400 Week 2 Maintain current dose of lamotrigine 200 300 Week 3 onward Maintain current dose of lamotrigine 200 200The benefit of continuing treatment in patients who had been stabilized in an 8 to 16 week open-label phase with lamotrigine tablets was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Pd-rx Pharmaceuticals, Inc.
![Lamotrigine (Lamotrigine ) Tablet [Pd-rx Pharmaceuticals, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Pd-rx Pharmaceuticals, Inc.
![Lamotrigine (Lamotrigine ) Tablet [Pd-rx Pharmaceuticals, Inc.] Lamotrigine (Lamotrigine ) Tablet [Pd-rx Pharmaceuticals, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
Lamotrigine Starter Kits provide lamotrigine at doses consistent with the recommended titration schedule for the first 5 weeks of treatment, based upon concomitant medications for patients with epilepsy (>12 years of age) and Bipolar I Disorder (≥18 years of age) and are intended to help reduce the potential for rash. The use of lamotrigine Starter Kits is recommended for appropriate patients who are starting or restarting lamotrigine [see How Supplied/Storage and Handling (16)].
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment should be necessary to the dose of lamotrigine.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, or primidone should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy * These drugs induce glucuronidation and increase clearance [see Drug Interactions (7) Pharmacokinetics (12.3)]. Other drugs, which have similar effects include estrogen-containing oral contraceptives and rifampin [see Drug Interactions (7), Pharmacokinetics (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin should follow the same dosing titration/maintenance regimen used with drugs that induce glucuronidation and increase clearance.
For Patients Taking
Valproate
For Patients Taking AEDs Other Than
Carbamazepine, Phenytoin, Phenobarbital, or
Primidone*, and Not Taking Valproate
For Patients Taking Carbamazepine,
Phenytoin, Phenobarbital, or
Primidone* and Not Taking Valproate
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Weeks 5 onwards
to maintenance
Increase by 25 to
50 mg/day every 1 to
2 weeks
Increase by 50 mg/day
every 1 to 2 weeks
Increase by
100 mg/day every 1 to
2 weeks.
Usual Maintenance
Dose
100 to 200 mg/day with
valproate alone
100 to 400 mg/day with
valproate and other
drugs that induce
glucuronication
(in 1 or 2 divided doses)
225 to 375 mg/day
(in 2 divided doses)
300 to 500 mg/day
(in 2 divided doses)
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
The smallest available strength of lamotrigine tablets is 25 mg, and only whole tablets should be administered. If the calculated dose cannot be achieved using whole tablets, the dose should be rounded down to the nearest whole tablet [see How Supplied/Storage and Handling (16) and Medication Guide].
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With EpilepsyNote: Only whole tablets should be used for dosing.
* These drugs induce glucuronidation and increase clearance [see Drug Interactions (7) Pharmacokinetics (12.3)]. Other drugs, which have similar effects include estrogen-containing oral contraceptives and rifampin [see Drug Interactions (7), Pharmacokinetics (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin should follow the same dosing titration/maintenance regimen used with drugs that induce glucuronidation.
For Patients Taking
Valproate
For Patients Taking
AEDs Other Than
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidone*, and Not
Taking Valproate
For Patients Taking
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidone* and Not
Taking Valproate
Weeks 1 and 2
0.15 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
(see Table 3 for weight
based dosing guide)
0.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
Weeks 3 and 4
0.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
(see Table 3 for weight
based dosing guide)
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
1.2 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
Weeks 5 onwards to
maintenance
The dose should be
increased every 1 to
2 weeks as follows:
calculate
0.3 mg/kg/day, round
this amount down to
the nearest whole
tablet, and add this
amount to the
previously administered
daily dose
The dose should be
increased every 1 to
2 weeks as follows:
calculate
0.6 mg/kg/day, round this
amount down to the
nearest whole tablet, and
add this amount to the
previously administered
daily dose
The dose should be
increased every 1 to
2 weeks as follows:
calculate
1.2 mg/kg/day, round
this amount down to the
nearest whole tablet, and
add this amount to the
previously administered
daily dose
Usual Maintenance
Dose
1 to 5 mg/kg/day (maximum
200 mg/day in 1 or 2
divided doses).
1 to 3 mg/kg/day with
valproate alone
4.5 to 7.5 mg/kg/day
(maximum 300 mg/day
in 2 divided doses)
5 to 15 mg/kg/day
(maximum 400 mg/day
in 2 divided doses)
Maintenance dose in
patients less than 30 kg
May need to be
increased by as much
as 50%, based on
clinical response
May need to be increased
by as much as 50%,
based on clinical
response
May need to be
increased by as much as
50%, based on clinical
response
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is
Give this daily dose, using the most appropriate combination of lamotrigine
2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age with Epilepsy
Lamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to
guidelines in Table 1 (if not already on
200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by
decrements no greater than
500 mg/day/week and then
maintain the dose of
500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1
week.
Simultaneously decrease to
250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve
maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, which increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder** See Drug Interactions (7) and Clinical Pharmacology (12.3) for a description of known drug interactions.
† Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine.
‡ Valproate has been shown to decrease the apparent clearance of lamotrigine.
For Patients Taking
Valproate‡
For Patients Not Taking Carbamazepine,
Phenytoin, Phenobarbital, Primidone, or
Rifampin† and Not Taking Valproate‡
For Patients Taking Carbamazepine, Phenytoin,
Phenobarbital, Primidone, or Rifampin† and Not
Taking Valproate‡
Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in
divided doses
Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications * Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine. † Valproate has been shown to decrease the apparent clearance of lamotrigine.
Discontinuation of Psychotropic Drugs
(excluding Carbamazepine,
After Discontinuation of Valproate†
After Discontinuation of Carbamazepine,
Phenytoin, Phenobarbital, Primidone,
or Rifampin*
Phenytoin, Phenobarbital, Primidone,
Rifampin*, or Valproate†)
Current dose of Lamotrigine
(mg/day)
100
Current dose of Lamotrigine
(mg/day)
400
Week 1
Maintain current dose of Lamotrigine
150
400
Week 2
Maintain current dose of Lamotrigine
200
300
Week 3 onward
Maintain current dose of Lamotrigine
200
200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Pd-rx Pharmaceuticals, Inc.
![Lamotrigine (Lamotrigine ) Tablet [Pd-rx Pharmaceuticals, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Pd-rx Pharmaceuticals, Inc.
![Lamotrigine (Lamotrigine ) Tablet [Pd-rx Pharmaceuticals, Inc.] Lamotrigine (Lamotrigine ) Tablet [Pd-rx Pharmaceuticals, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
Lamotrigine Starter Kits provide lamotrigine at doses consistent with the recommended titration schedule for the first 5 weeks of treatment, based upon concomitant medications for patients with epilepsy (>12 years of age) and Bipolar I Disorder (≥18 years of age) and are intended to help reduce the potential for rash. The use of lamotrigine Starter Kits is recommended for appropriate patients who are starting or restarting lamotrigine [see How Supplied/Storage and Handling (16)].
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment should be necessary to the dose of lamotrigine.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, or primidone should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy * These drugs induce glucuronidation and increase clearance [see Drug Interactions (7) Pharmacokinetics (12.3)]. Other drugs, which have similar effects include estrogen-containing oral contraceptives and rifampin [see Drug Interactions (7), Pharmacokinetics (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin should follow the same dosing titration/maintenance regimen used with drugs that induce glucuronidation and increase clearance.
For Patients Taking
Valproate
For Patients Taking AEDs Other Than
Carbamazepine, Phenytoin, Phenobarbital, or
Primidone*, and Not Taking Valproate
For Patients Taking Carbamazepine,
Phenytoin, Phenobarbital, or
Primidone* and Not Taking Valproate
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Weeks 5 onwards
to maintenance
Increase by 25 to
50 mg/day every 1 to
2 weeks
Increase by 50 mg/day
every 1 to 2 weeks
Increase by
100 mg/day every 1 to
2 weeks.
Usual Maintenance
Dose
100 to 200 mg/day with
valproate alone
100 to 400 mg/day with
valproate and other
drugs that induce
glucuronication
(in 1 or 2 divided doses)
225 to 375 mg/day
(in 2 divided doses)
300 to 500 mg/day
(in 2 divided doses)
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
The smallest available strength of lamotrigine tablets is 25 mg, and only whole tablets should be administered. If the calculated dose cannot be achieved using whole tablets, the dose should be rounded down to the nearest whole tablet [see How Supplied/Storage and Handling (16) and Medication Guide].
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With EpilepsyNote: Only whole tablets should be used for dosing.
* These drugs induce glucuronidation and increase clearance [see Drug Interactions (7) Pharmacokinetics (12.3)]. Other drugs, which have similar effects include estrogen-containing oral contraceptives and rifampin [see Drug Interactions (7), Pharmacokinetics (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin should follow the same dosing titration/maintenance regimen used with drugs that induce glucuronidation.
For Patients Taking
Valproate
For Patients Taking
AEDs Other Than
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidone*, and Not
Taking Valproate
For Patients Taking
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidone* and Not
Taking Valproate
Weeks 1 and 2
0.15 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
(see Table 3 for weight
based dosing guide)
0.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
Weeks 3 and 4
0.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
(see Table 3 for weight
based dosing guide)
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
1.2 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
Weeks 5 onwards to
maintenance
The dose should be
increased every 1 to
2 weeks as follows:
calculate
0.3 mg/kg/day, round
this amount down to
the nearest whole
tablet, and add this
amount to the
previously administered
daily dose
The dose should be
increased every 1 to
2 weeks as follows:
calculate
0.6 mg/kg/day, round this
amount down to the
nearest whole tablet, and
add this amount to the
previously administered
daily dose
The dose should be
increased every 1 to
2 weeks as follows:
calculate
1.2 mg/kg/day, round
this amount down to the
nearest whole tablet, and
add this amount to the
previously administered
daily dose
Usual Maintenance
Dose
1 to 5 mg/kg/day (maximum
200 mg/day in 1 or 2
divided doses).
1 to 3 mg/kg/day with
valproate alone
4.5 to 7.5 mg/kg/day
(maximum 300 mg/day
in 2 divided doses)
5 to 15 mg/kg/day
(maximum 400 mg/day
in 2 divided doses)
Maintenance dose in
patients less than 30 kg
May need to be
increased by as much
as 50%, based on
clinical response
May need to be increased
by as much as 50%,
based on clinical
response
May need to be
increased by as much as
50%, based on clinical
response
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is
Give this daily dose, using the most appropriate combination of lamotrigine
2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age with Epilepsy
Lamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to
guidelines in Table 1 (if not already on
200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by
decrements no greater than
500 mg/day/week and then
maintain the dose of
500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1
week.
Simultaneously decrease to
250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve
maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, which increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder** See Drug Interactions (7) and Clinical Pharmacology (12.3) for a description of known drug interactions.
† Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine.
‡ Valproate has been shown to decrease the apparent clearance of lamotrigine.
For Patients Taking
Valproate‡
For Patients Not Taking Carbamazepine,
Phenytoin, Phenobarbital, Primidone, or
Rifampin† and Not Taking Valproate‡
For Patients Taking Carbamazepine, Phenytoin,
Phenobarbital, Primidone, or Rifampin† and Not
Taking Valproate‡
Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in
divided doses
Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications * Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine. † Valproate has been shown to decrease the apparent clearance of lamotrigine.
Discontinuation of Psychotropic Drugs
(excluding Carbamazepine,
After Discontinuation of Valproate†
After Discontinuation of Carbamazepine,
Phenytoin, Phenobarbital, Primidone,
or Rifampin*
Phenytoin, Phenobarbital, Primidone,
Rifampin*, or Valproate†)
Current dose of Lamotrigine
(mg/day)
100
Current dose of Lamotrigine
(mg/day)
400
Week 1
Maintain current dose of Lamotrigine
150
400
Week 2
Maintain current dose of Lamotrigine
200
300
Week 3 onward
Maintain current dose of Lamotrigine
200
200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Pd-rx Pharmaceuticals, Inc.
![Lamotrigine (Lamotrigine ) Tablet [Pd-rx Pharmaceuticals, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Pd-rx Pharmaceuticals, Inc.
![Lamotrigine (Lamotrigine ) Tablet [Pd-rx Pharmaceuticals, Inc.] Lamotrigine (Lamotrigine ) Tablet [Pd-rx Pharmaceuticals, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
Lamotrigine Starter Kits provide lamotrigine at doses consistent with the recommended titration schedule for the first 5 weeks of treatment, based upon concomitant medications for patients with epilepsy (>12 years of age) and Bipolar I Disorder (≥18 years of age) and are intended to help reduce the potential for rash. The use of lamotrigine Starter Kits is recommended for appropriate patients who are starting or restarting lamotrigine [see How Supplied/Storage and Handling (16)].
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment should be necessary to the dose of lamotrigine.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, or primidone should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy * These drugs induce glucuronidation and increase clearance [see Drug Interactions (7) Pharmacokinetics (12.3)]. Other drugs, which have similar effects include estrogen-containing oral contraceptives and rifampin [see Drug Interactions (7), Pharmacokinetics (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin should follow the same dosing titration/maintenance regimen used with drugs that induce glucuronidation and increase clearance.
For Patients Taking
Valproate
For Patients Taking AEDs Other Than
Carbamazepine, Phenytoin, Phenobarbital, or
Primidone*, and Not Taking Valproate
For Patients Taking Carbamazepine,
Phenytoin, Phenobarbital, or
Primidone* and Not Taking Valproate
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Weeks 5 onwards
to maintenance
Increase by 25 to
50 mg/day every 1 to
2 weeks
Increase by 50 mg/day
every 1 to 2 weeks
Increase by
100 mg/day every 1 to
2 weeks.
Usual Maintenance
Dose
100 to 200 mg/day with
valproate alone
100 to 400 mg/day with
valproate and other
drugs that induce
glucuronication
(in 1 or 2 divided doses)
225 to 375 mg/day
(in 2 divided doses)
300 to 500 mg/day
(in 2 divided doses)
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
The smallest available strength of lamotrigine tablets is 25 mg, and only whole tablets should be administered. If the calculated dose cannot be achieved using whole tablets, the dose should be rounded down to the nearest whole tablet [see How Supplied/Storage and Handling (16) and Medication Guide].
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With EpilepsyNote: Only whole tablets should be used for dosing.
* These drugs induce glucuronidation and increase clearance [see Drug Interactions (7) Pharmacokinetics (12.3)]. Other drugs, which have similar effects include estrogen-containing oral contraceptives and rifampin [see Drug Interactions (7), Pharmacokinetics (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin should follow the same dosing titration/maintenance regimen used with drugs that induce glucuronidation.
For Patients Taking
Valproate
For Patients Taking
AEDs Other Than
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidone*, and Not
Taking Valproate
For Patients Taking
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidone* and Not
Taking Valproate
Weeks 1 and 2
0.15 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
(see Table 3 for weight
based dosing guide)
0.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
Weeks 3 and 4
0.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
(see Table 3 for weight
based dosing guide)
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
1.2 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
Weeks 5 onwards to
maintenance
The dose should be
increased every 1 to
2 weeks as follows:
calculate
0.3 mg/kg/day, round
this amount down to
the nearest whole
tablet, and add this
amount to the
previously administered
daily dose
The dose should be
increased every 1 to
2 weeks as follows:
calculate
0.6 mg/kg/day, round this
amount down to the
nearest whole tablet, and
add this amount to the
previously administered
daily dose
The dose should be
increased every 1 to
2 weeks as follows:
calculate
1.2 mg/kg/day, round
this amount down to the
nearest whole tablet, and
add this amount to the
previously administered
daily dose
Usual Maintenance
Dose
1 to 5 mg/kg/day (maximum
200 mg/day in 1 or 2
divided doses).
1 to 3 mg/kg/day with
valproate alone
4.5 to 7.5 mg/kg/day
(maximum 300 mg/day
in 2 divided doses)
5 to 15 mg/kg/day
(maximum 400 mg/day
in 2 divided doses)
Maintenance dose in
patients less than 30 kg
May need to be
increased by as much
as 50%, based on
clinical response
May need to be increased
by as much as 50%,
based on clinical
response
May need to be
increased by as much as
50%, based on clinical
response
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is
Give this daily dose, using the most appropriate combination of lamotrigine
2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age with Epilepsy
Lamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to
guidelines in Table 1 (if not already on
200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by
decrements no greater than
500 mg/day/week and then
maintain the dose of
500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1
week.
Simultaneously decrease to
250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve
maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, which increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder** See Drug Interactions (7) and Clinical Pharmacology (12.3) for a description of known drug interactions.
† Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine.
‡ Valproate has been shown to decrease the apparent clearance of lamotrigine.
For Patients Taking
Valproate‡
For Patients Not Taking Carbamazepine,
Phenytoin, Phenobarbital, Primidone, or
Rifampin† and Not Taking Valproate‡
For Patients Taking Carbamazepine, Phenytoin,
Phenobarbital, Primidone, or Rifampin† and Not
Taking Valproate‡
Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in
divided doses
Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications * Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine. † Valproate has been shown to decrease the apparent clearance of lamotrigine.
Discontinuation of Psychotropic Drugs
(excluding Carbamazepine,
After Discontinuation of Valproate†
After Discontinuation of Carbamazepine,
Phenytoin, Phenobarbital, Primidone,
or Rifampin*
Phenytoin, Phenobarbital, Primidone,
Rifampin*, or Valproate†)
Current dose of Lamotrigine
(mg/day)
100
Current dose of Lamotrigine
(mg/day)
400
Week 1
Maintain current dose of Lamotrigine
150
400
Week 2
Maintain current dose of Lamotrigine
200
300
Week 3 onward
Maintain current dose of Lamotrigine
200
200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Pd-rx Pharmaceuticals, Inc.
![Lamotrigine (Lamotrigine ) Tablet [Pd-rx Pharmaceuticals, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Pd-rx Pharmaceuticals, Inc.
![Lamotrigine (Lamotrigine ) Tablet [Pd-rx Pharmaceuticals, Inc.] Lamotrigine (Lamotrigine ) Tablet [Pd-rx Pharmaceuticals, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
Lamotrigine Starter Kits provide lamotrigine at doses consistent with the recommended titration schedule for the first 5 weeks of treatment, based upon concomitant medications for patients with epilepsy (>12 years of age) and Bipolar I Disorder (≥18 years of age) and are intended to help reduce the potential for rash. The use of lamotrigine Starter Kits is recommended for appropriate patients who are starting or restarting lamotrigine [see How Supplied/Storage and Handling (16)].
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment should be necessary to the dose of lamotrigine.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, or primidone should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy * These drugs induce glucuronidation and increase clearance [see Drug Interactions (7) Pharmacokinetics (12.3)]. Other drugs, which have similar effects include estrogen-containing oral contraceptives and rifampin [see Drug Interactions (7), Pharmacokinetics (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin should follow the same dosing titration/maintenance regimen used with drugs that induce glucuronidation and increase clearance.
For Patients Taking
Valproate
For Patients Taking AEDs Other Than
Carbamazepine, Phenytoin, Phenobarbital, or
Primidone*, and Not Taking Valproate
For Patients Taking Carbamazepine,
Phenytoin, Phenobarbital, or
Primidone* and Not Taking Valproate
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Weeks 5 onwards
to maintenance
Increase by 25 to
50 mg/day every 1 to
2 weeks
Increase by 50 mg/day
every 1 to 2 weeks
Increase by
100 mg/day every 1 to
2 weeks.
Usual Maintenance
Dose
100 to 200 mg/day with
valproate alone
100 to 400 mg/day with
valproate and other
drugs that induce
glucuronication
(in 1 or 2 divided doses)
225 to 375 mg/day
(in 2 divided doses)
300 to 500 mg/day
(in 2 divided doses)
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
The smallest available strength of lamotrigine tablets is 25 mg, and only whole tablets should be administered. If the calculated dose cannot be achieved using whole tablets, the dose should be rounded down to the nearest whole tablet [see How Supplied/Storage and Handling (16) and Medication Guide].
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With EpilepsyNote: Only whole tablets should be used for dosing.
* These drugs induce glucuronidation and increase clearance [see Drug Interactions (7) Pharmacokinetics (12.3)]. Other drugs, which have similar effects include estrogen-containing oral contraceptives and rifampin [see Drug Interactions (7), Pharmacokinetics (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin should follow the same dosing titration/maintenance regimen used with drugs that induce glucuronidation.
For Patients Taking
Valproate
For Patients Taking
AEDs Other Than
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidone*, and Not
Taking Valproate
For Patients Taking
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidone* and Not
Taking Valproate
Weeks 1 and 2
0.15 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
(see Table 3 for weight
based dosing guide)
0.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
Weeks 3 and 4
0.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
(see Table 3 for weight
based dosing guide)
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
1.2 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
Weeks 5 onwards to
maintenance
The dose should be
increased every 1 to
2 weeks as follows:
calculate
0.3 mg/kg/day, round
this amount down to
the nearest whole
tablet, and add this
amount to the
previously administered
daily dose
The dose should be
increased every 1 to
2 weeks as follows:
calculate
0.6 mg/kg/day, round this
amount down to the
nearest whole tablet, and
add this amount to the
previously administered
daily dose
The dose should be
increased every 1 to
2 weeks as follows:
calculate
1.2 mg/kg/day, round
this amount down to the
nearest whole tablet, and
add this amount to the
previously administered
daily dose
Usual Maintenance
Dose
1 to 5 mg/kg/day (maximum
200 mg/day in 1 or 2
divided doses).
1 to 3 mg/kg/day with
valproate alone
4.5 to 7.5 mg/kg/day
(maximum 300 mg/day
in 2 divided doses)
5 to 15 mg/kg/day
(maximum 400 mg/day
in 2 divided doses)
Maintenance dose in
patients less than 30 kg
May need to be
increased by as much
as 50%, based on
clinical response
May need to be increased
by as much as 50%,
based on clinical
response
May need to be
increased by as much as
50%, based on clinical
response
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is
Give this daily dose, using the most appropriate combination of lamotrigine
2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age with Epilepsy
Lamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to
guidelines in Table 1 (if not already on
200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by
decrements no greater than
500 mg/day/week and then
maintain the dose of
500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1
week.
Simultaneously decrease to
250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve
maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, which increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder** See Drug Interactions (7) and Clinical Pharmacology (12.3) for a description of known drug interactions.
† Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine.
‡ Valproate has been shown to decrease the apparent clearance of lamotrigine.
For Patients Taking
Valproate‡
For Patients Not Taking Carbamazepine,
Phenytoin, Phenobarbital, Primidone, or
Rifampin† and Not Taking Valproate‡
For Patients Taking Carbamazepine, Phenytoin,
Phenobarbital, Primidone, or Rifampin† and Not
Taking Valproate‡
Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in
divided doses
Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications * Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine. † Valproate has been shown to decrease the apparent clearance of lamotrigine.
Discontinuation of Psychotropic Drugs
(excluding Carbamazepine,
After Discontinuation of Valproate†
After Discontinuation of Carbamazepine,
Phenytoin, Phenobarbital, Primidone,
or Rifampin*
Phenytoin, Phenobarbital, Primidone,
Rifampin*, or Valproate†)
Current dose of Lamotrigine
(mg/day)
100
Current dose of Lamotrigine
(mg/day)
400
Week 1
Maintain current dose of Lamotrigine
150
400
Week 2
Maintain current dose of Lamotrigine
200
300
Week 3 onward
Maintain current dose of Lamotrigine
200
200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ] Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Epilepsy
Adjunctive Use:
Lamotrigine is indicated as adjunctive therapy for partial seizures and the generalized seizures of Lennox-Gastaut syndrome in adult and pediatric patients (years of age).
Monotherapy Use:
Lamotrigine tablets and lamotrigine tablets (chewable, dispersible) are indicated for conversion to monotherapy in adults with partial seizures who are receiving treatment with carbamazepine, phenytoin, phenobarbital, primidone, or valproate as the single AED.
Safety and effectiveness of lamotrigine tablets and lamotrigine tablets (chewable, dispersible)have not been established. (1) as initial monotherapy, (2) for conversion to monotherapy from AEDs other than carbamazepine, phenytoin, phenobarbital, primidone, or valproate, or (3) for simultaneous conversion to monotherapy from 2 or more concomitant AEDs.
Bipolar Disorder
Lamotrigine tablets and lamotrigine tablets (chewable, dispersible) are indicated for the maintenance treatment of Bipolar I Disorder to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The effectiveness of lamotrigine in the acute treatment of mood episodes has not been established.
General Dosing Considerations for Epilepsy and Bipolar Disorder Patients:
The risk of nonserious rash is increased when the recommended initial dose and/or the rate of dose escalation of Lamotrigine is exceeded. There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have been reported in the absence of these factors (see BOX WARNING). Therefore, it is important that the dosing recommendations be followed closely.
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed.
Lamotrigine Tablets and Lamotrigine Tablets (Chewable, Dispersible)Added to Drugs Known to Induce or Inhibit Glucuronidation:
Drugs other than those listed in PRECAUTIONS: Drug Interactionshave not been systematically evaluated in
combination with Lamotrigine. Since lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine, and doses of Lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder:
A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response.
The half-life of lamotrigine is affected by other concomitant medications (see CLINICAL PHARMACOLOGY: Pharmacokinetics and Drug Metabolism).
See also DOSAGE AND ADMINISTRATION: Special Populations.
Special Populations: Women and Oral Contraceptives: Starting Lamotrigine Tablets and LamotrigineTablets (Chewable, Dispersible)in Women Taking Oral Contraceptives
Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine (see PRECAUTIONS: Drug Interactions), no adjustments to the recommended dose escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED (see Table 11). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets and Lamotrigine Tablets (Chewable, Dispersible)
Taking Estrogen-Containing Oral Contraceptives:
For women not taking carbamazepine, phenytoin, phenobarbital, primidone,
or rifampin, the maintenance dose of Lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level (see PRECAUTIONS: Drug Interactions). (2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of Lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose will in most cases need to be increased by as much as 2-fold, in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate unless lamotrigine plasma levels or clinical response support larger increases (see Table 11, column 2,). Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse events, such as dizziness, ataxia, and diplopia (see PRECAUTIONS: Drug Interactions). If adverse events attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment should be necessary to the dose of Lamotrigine. (3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50%, in order to maintain a consistent lamotrigine plasma level. The decrease in dose of Lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise (see PRECAUTIONS: Drug Interactions). For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy:
The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment:
Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver dysfunction (see CLINICAL PHARMACOLOGY), the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without
ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Functional Impairment:
Initial doses of lamotrigine tablets and lamotrigine tablets (chewable, dispersible) should be based on patients' AED regimen (see above); reduced maintenance doses may be effective for patients with significant renal functional impairment (see CLINICAL PHARMACOLOGY). Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Epilepsy:
Adjunctive Therapy With Lamotrigine Tablets and Lamotrigine Tablets (Chewable, Dispersible) for Epilepsy:
This section provides specific dosing recommendations for patients 2 to 12 years of age and patients greater than 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED (Table 9 for patients 2 to 12 years of age and Table 11 for patients greater than 12 years of age). A weight based dosing guide for pediatric patients on concomitant valproate is provided in Table 10.
Patients 2 to 12 Years of Age:
Recommended dosing guidelines are summarized in Table 9.
Note that some of the starting doses and dose escalations listed in Table 9 are different than those used in clinical trials; however, the maintenance doses are the same as in clinical trials. Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestions that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 9. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy
*Rifampin and estrogen-containing oral contraceptives have also been shown to increase the apparent clearance of lamotrigine (see PRECAUTIONS: Drug Interactions).For Patients Taking Valproate (see Table 10 for weight- based dosing guide)For Patients Taking AEDs Other Than Carbamazepine, Phenytoi n, Phenobarbital, Primidone *, or ValproateFor Patients Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone *and Not Taking ValproateWeeks 1 and 20.15 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 10 for weight-based dosing guide).0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet.0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet.Weeks 3 and 40.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 10 for weight-based dosing guide).0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet.1.2 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet.Weeks 5 onwards to maintenanceThe dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose.The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily doseThe dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily doseUsual Maintenance Dose1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses). 1 to 3 mg/kg/day with valproate alone4.5 to 7.5 mg/kg/day (maximum 300 mg/day in 2 divided doses)5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses)Maintenance dose in patients less than 30 kgMay need to be increased by as much as 50%, based on clinical responseMay need to be increased by as much as 50%, based on clinical responseMay need to be increased by as much as 50%, based on clinical responseNote: Only whole tablets should be used for dosing
Table 10. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy
If the patient's weight isGive this daily dose, using the most appropriate combination of lamotrigine tablets (chewable, dispersible), 5 mgGreater thanAnd less thanWeeks 1 and 2Weeks 3 and 434.1 kg40 kg5 mg every day10 mg every dayPatients Over 12 Years of Age:
Recommended dosing guidelines are summarized in Table 11.
Table 11. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy
*Rifampin and estrogen-containing oral contraceptives have also been shown to increase the apparent clearance of lamotrigine (see PRECAUTIONS: Drug Interactions).For Patients Taking ValproateFor Patients Taking AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate *For Patients Taking Carbamazepine, Phenytoin, PhenobarbitaL, Primidone *and Not Taking ValproateWeeks 1 and 225 mg every other day25 mg every day50 mg/dayWeeks 3 and 425 mg every day50 mg/day100 mg/day (in 2 divided doses)Weeks 5 onwards to maintenanceIncrease by 25 to 50 mg/ day every 1 to 2 weeksIncrease by 50 mg/ day every 1 to 2 weeksIncrease by 100 mg/ day every 1 to 2 weeks.Usual Maintenance Dose100 to 400 mg/day (1 or 2 divided doses) 100 to 200 mg/day with Valproate alone225 to 375 mg/day (in 2 divided doses).300 to 500 mg/day (in 2 divided doses).Conversion from Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate as the Single AED to Monotherapy With Lamotrigine in PatientsYears of Age With Epilepsy:
The goal of the transition regimen is to effect the conversion to monotherapy with Lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded (see BOX WARNING).
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine:
After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 11, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine The conversion regimen involves 4 steps (see Table 12).
Table 12. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in PatientsYears of Age With Epilepsy
LamotrigineValproateStep 1Achieve a dose of 200 mg/day according to guidelines in Table 11 (if not already on 200 mg/ day).Maintain previous stable dose.Step 2Maintain at 200 mg/day.Decrease to 500 mg/day by decrements no greater than 500 mg/day per week and then maintain the dose of 500 mg/day for 1 week.Step 3Increase to 300 mg/day and maintain for 1 week.Simultaneously decrease to 250 mg/day and maintain for 1 week.Step 4Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.Discontinue.Conversion from Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine:
No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
Usual Maintenance Dose for Epilepsy
The usual maintenance doses identified in Tables 9-11 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive Lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive Lamotrigine as high as 200 mg/ day have been used. The advantage of using doses above those recommended in Tables 9-12 has not been established in controlled trials.
Discontinuation Strategy for Patients With Epilepsy:
For patients receiving lamotrigine in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse experiences is observed.
If a decision is made to discontinue therapy with Lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal (see PRECAUTIONS).
Discontinuing carbamazepine, phenytoin, phenobarbital, or primidone should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder
The goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate,which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, which increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated, however, no additional benefit was seen at 400 mg/day compared to 200 mg/day (see CLINICAL STUDIES: Bipolar Disorder). Accordingly, doses above 200 mg/ day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 13. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 14). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 14). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
Dosage adjustments will be necessary in most patients who start or stop estrogen-containing oral contraceptives while taking lamotrigine (see DOSAGE AND ADMINISTRATION: Special Populations: Women and Oral Contraceptives: Adjustments to the Maintenace Dose of Lamotrigine).
If other drugs are subsequently introduced, the dose of Lamotrigine may need to be adjusted.
In particular, the introduction of valproate requires reduction in the dose of Lamotrigine (see CLINICAL PHARMACOLOGY: Drug Interactions). To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded (see BOX WARNING).
Table 13. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder *
*See CLINICAL PHARMACOLOGY: Drug Interactions:and PRECAUTIONS: Drug Interactionsfor a description of known drug interactions. Carbamazepine, phenytoin, phenobarbital, primidone, rifampin, have been shown to increase the apparent clearance of lamotrigine. Valproate has been shown to decrease the apparent clearance of lamotrigine.For Patients Not Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone or Rifampin and Not Taking Valproate For Patients Taking Valproate For Patients Taking Carbamazepine (or Other Enzyme-Inducing Drugs) and Not Taking Valproate Weeks 1 and 225 mg daily25 mg every other day50 mg dailyWeeks 3 and 450 mg daily25 mg daily100 mg daily, in divided dosesWeek 5100 mg daily50 mg daily200 mg daily, in divided dosesWeek 6200 mg daily100 mg daily300 mg daily, in divided dosesWeek 7200 mg daily100 mg dailyup to 400 mg daily, in divided doses
Table 14. Adjustments to Lamotrigine Dosing for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications *
*See CLINICAL PHARMACOLOGY: Drug Interactions:and PRECAUTIONS: Drug Interactionsfor a description of known drug interactions. Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine. Valproate has been shown to decrease the apparent clearance of lamotrigine.Discontinuation of Psychotropic Drugs (excluding Valproate , Carbamazepine, or Other Enzyme-Inducing Drugs )After Discontinuation of Valproate After Discontinuation of Carbamazepine or Other Enzyme-Inducing Drugs Current Lamotrigine dose (mg/day) 100Current Lamotrigine dose (mg/day) 400Week 1Maintain current lamotrigine dose150400Week 2Maintain current lamotrigine dose200300Week 3 onwardMaintain current lamotrigine dose200200There is no body of evidence available to answer the question of how long the patient should remain on lamotrigine therapy. Systematic evaluation of the efficacy of lamotrigine in patients with either depression or mania who responded to standard therapy during an acute 8 to 16 week treatment phase and were then randomized to lamotrigine or placebo for up to 76 weeks of observation for affective relapse demonstrated a benefit of such maintenance treatment (see CLINICAL STUDIES: Bipolar Disorder). Nevertheless, patients should be periodically reassessed to determine the need for maintenance treatment.
Discontinuation Strategy in Bipolar Disorder:
As with other AEDs, lamotrigine should not be abruptly discontinued. In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse experiences following abrupt termination of lamotrigine. In clinical trials in patients with bipolar disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal.
Administration of Lamotrigine Tablets (Chewable, Dispersible)
Lamotrigine tablets (Chewable, Dispersible) may be swallowed whole, chewed, or dispersed in water or diluted fruit juice. If the tablets are chewed, consume a small amount of water or diluted fruit juice to aid in swallowing.
To disperse lamotrigine tablets (chewable, dispersible), add the tablets to a small amount of liquid (1 teaspoon, or enough to cover the medication). Approximately 1 minute later, when the tablets are completely dispersed, swirl the solution and consume the entire quantity immediately.
No attempt should be made to administer partial quantities of the dispersed tablets.
-
Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ] Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Epilepsy
Adjunctive Use:
Lamotrigine is indicated as adjunctive therapy for partial seizures and the generalized seizures of Lennox-Gastaut syndrome in adult and pediatric patients (years of age).
Monotherapy Use:
Lamotrigine tablets and lamotrigine tablets (chewable, dispersible) are indicated for conversion to monotherapy in adults with partial seizures who are receiving treatment with carbamazepine, phenytoin, phenobarbital, primidone, or valproate as the single AED.
Safety and effectiveness of lamotrigine tablets and lamotrigine tablets (chewable, dispersible)have not been established. (1) as initial monotherapy, (2) for conversion to monotherapy from AEDs other than carbamazepine, phenytoin, phenobarbital, primidone, or valproate, or (3) for simultaneous conversion to monotherapy from 2 or more concomitant AEDs.
Bipolar Disorder
Lamotrigine tablets and lamotrigine tablets (chewable, dispersible) are indicated for the maintenance treatment of Bipolar I Disorder to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The effectiveness of lamotrigine in the acute treatment of mood episodes has not been established.
General Dosing Considerations for Epilepsy and Bipolar Disorder Patients:
The risk of nonserious rash is increased when the recommended initial dose and/or the rate of dose escalation of Lamotrigine is exceeded. There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have been reported in the absence of these factors (see BOX WARNING). Therefore, it is important that the dosing recommendations be followed closely.
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed.
Lamotrigine Tablets and Lamotrigine Tablets (Chewable, Dispersible)Added to Drugs Known to Induce or Inhibit Glucuronidation:
Drugs other than those listed in PRECAUTIONS: Drug Interactionshave not been systematically evaluated in
combination with Lamotrigine. Since lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine, and doses of Lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder:
A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response.
The half-life of lamotrigine is affected by other concomitant medications (see CLINICAL PHARMACOLOGY: Pharmacokinetics and Drug Metabolism).
See also DOSAGE AND ADMINISTRATION: Special Populations.
Special Populations: Women and Oral Contraceptives: Starting Lamotrigine Tablets and LamotrigineTablets (Chewable, Dispersible)in Women Taking Oral Contraceptives
Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine (see PRECAUTIONS: Drug Interactions), no adjustments to the recommended dose escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED (see Table 11). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets and Lamotrigine Tablets (Chewable, Dispersible)
1. Taking Estrogen-Containing Oral Contraceptives:
For women not taking carbamazepine, phenytoin, phenobarbital, primidone,
or rifampin, the maintenance dose of Lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level (see PRECAUTIONS: Drug Interactions). (2) Starting Estrogen-Containing Oral Contraceptives:In women taking a stable dose of Lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose will in most cases need to be increased by as much as 2-fold, in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate unless lamotrigine plasma levels or clinical response support larger increases (see Table 11, column 2,). Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse events, such as dizziness, ataxia, and diplopia (see PRECAUTIONS: Drug Interactions). If adverse events attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment should be necessary to the dose of Lamotrigine. ( 3) Stopping Estrogen-Containing Oral Contraceptives:For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50%, in order to maintain a consistent lamotrigine plasma level. The decrease in dose of Lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise (see PRECAUTIONS: Drug Interactions). For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy:
The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment:
Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver dysfunction (see CLINICAL PHARMACOLOGY), the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without
ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Functional Impairment:
Initial doses of lamotrigine tablets and lamotrigine tablets (chewable, dispersible) should be based on patients' AED regimen (see above); reduced maintenance doses may be effective for patients with significant renal functional impairment (see CLINICAL PHARMACOLOGY). Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Epilepsy:
Adjunctive Therapy With Lamotrigine Tablets and Lamotrigine Tablets (Chewable, Dispersible) for Epilepsy:
This section provides specific dosing recommendations for patients 2 to 12 years of age and patients greater than 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED (Table 9 for patients 2 to 12 years of age and Table 11 for patients greater than 12 years of age). A weight based dosing guide for pediatric patients on concomitant valproate is provided in Table 10.
Patients 2 to 12 Years of Age:
Recommended dosing guidelines are summarized in Table 9.
Note that some of the starting doses and dose escalations listed in Table 9 are different than those used in clinical trials; however, the maintenance doses are the same as in clinical trials. Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestions that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 9. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy
*Rifampin and estrogen-containing oral contraceptives have also been shown to increase the apparent clearance of lamotrigine (see PRECAUTIONS: Drug Interactions).For Patients Taking Valproate (see Table 10 for weight- based dosing guide)For Patients Taking AEDs Other Than Carbamazepine, Phenytoi n, Phenobarbital, Primidone *, or ValproateFor Patients Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone *and Not Taking ValproateWeeks 1 and 20.15 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 10 for weight-based dosing guide).0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet.0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet.Weeks 3 and 40.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 10 for weight-based dosing guide).0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet.1.2 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet.Weeks 5 onwards to maintenanceThe dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose.The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily doseThe dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily doseUsual Maintenance Dose1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses). 1 to 3 mg/kg/day with valproate alone4.5 to 7.5 mg/kg/day (maximum 300 mg/day in 2 divided doses)5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses)Maintenance dose in patients less than 30 kgMay need to be increased by as much as 50%, based on clinical responseMay need to be increased by as much as 50%, based on clinical responseMay need to be increased by as much as 50%, based on clinical responseNote: Only whole tablets should be used for dosing
Table 10. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy
If the patient's weight isGive this daily dose, using the most appropriate combination of lamotrigine tablets (chewable, dispersible), 5 mgGreater thanAnd less thanWeeks 1 and 2Weeks 3 and 434.1 kg40 kg5 mg every day10 mg every dayPatients Over 12 Years of Age:
Recommended dosing guidelines are summarized in Table 11.
Table 11. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy
*Rifampin and estrogen-containing oral contraceptives have also been shown to increase the apparent clearance of lamotrigine (see PRECAUTIONS: Drug Interactions).For Patients Taking ValproateFor Patients Taking AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate *For Patients Taking Carbamazepine, Phenytoin, PhenobarbitaL, Primidone *and Not Taking ValproateWeeks 1 and 225 mg every other day25 mg every day50 mg/dayWeeks 3 and 425 mg every day50 mg/day100 mg/day (in 2 divided doses)Weeks 5 onwards to maintenanceIncrease by 25 to 50 mg/ day every 1 to 2 weeksIncrease by 50 mg/ day every 1 to 2 weeksIncrease by 100 mg/ day every 1 to 2 weeks.Usual Maintenance Dose100 to 400 mg/day (1 or 2 divided doses) 100 to 200 mg/day with Valproate alone225 to 375 mg/day (in 2 divided doses).300 to 500 mg/day (in 2 divided doses).Conversion from Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate as the Single AED to Monotherapy With Lamotrigine in PatientsYears of Age With Epilepsy:
The goal of the transition regimen is to effect the conversion to monotherapy with Lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded (see BOX WARNING).
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine:
After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 11, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine The conversion regimen involves 4 steps (see Table 12).
Table 12. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in PatientsYears of Age With Epilepsy
LamotrigineValproateStep 1Achieve a dose of 200 mg/day according to guidelines in Table 11 (if not already on 200 mg/ day).Maintain previous stable dose.Step 2Maintain at 200 mg/day.Decrease to 500 mg/day by decrements no greater than 500 mg/day per week and then maintain the dose of 500 mg/day for 1 week.Step 3Increase to 300 mg/day and maintain for 1 week.Simultaneously decrease to 250 mg/day and maintain for 1 week.Step 4Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.Discontinue. Conversion from Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine:
No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
Usual Maintenance Dose for Epilepsy
The usual maintenance doses identified in Tables 9-11 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive Lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive Lamotrigine as high as 200 mg/ day have been used. The advantage of using doses above those recommended in Tables 9-12 has not been established in controlled trials.
Discontinuation Strategy for Patients With Epilepsy:
For patients receiving lamotrigine in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse experiences is observed.
If a decision is made to discontinue therapy with Lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal (see PRECAUTIONS).
Discontinuing carbamazepine, phenytoin, phenobarbital, or primidone should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder
The goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate,which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, which increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated, however, no additional benefit was seen at 400 mg/day compared to 200 mg/day (see CLINICAL STUDIES: Bipolar Disorder). Accordingly, doses above 200 mg/ day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 13. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 14). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 14). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
Dosage adjustments will be necessary in most patients who start or stop estrogen-containing oral contraceptives while taking lamotrigine (see DOSAGE AND ADMINISTRATION: Special Populations: Women and Oral Contraceptives: Adjustments to the Maintenace Dose of Lamotrigine).
If other drugs are subsequently introduced, the dose of Lamotrigine may need to be adjusted.
In particular, the introduction of valproate requires reduction in the dose of Lamotrigine (see CLINICAL PHARMACOLOGY: Drug Interactions). To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded (see BOX WARNING).
Table 13. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder *
*See CLINICAL PHARMACOLOGY: Drug Interactions:and PRECAUTIONS: Drug Interactionsfor a description of known drug interactions. Carbamazepine, phenytoin, phenobarbital, primidone, rifampin, have been shown to increase the apparent clearance of lamotrigine. Valproate has been shown to decrease the apparent clearance of lamotrigine.For Patients Not Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone or Rifampin and Not Taking Valproate For Patients Taking Valproate For Patients Taking Carbamazepine (or Other Enzyme-Inducing Drugs) and Not Taking Valproate Weeks 1 and 225 mg daily25 mg every other day50 mg dailyWeeks 3 and 450 mg daily25 mg daily100 mg daily, in divided dosesWeek 5100 mg daily50 mg daily200 mg daily, in divided dosesWeek 6200 mg daily100 mg daily300 mg daily, in divided dosesWeek 7200 mg daily100 mg dailyup to 400 mg daily, in divided doses
Table 14. Adjustments to Lamotrigine Dosing for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications *
*See CLINICAL PHARMACOLOGY: Drug Interactions:and PRECAUTIONS: Drug Interactionsfor a description of known drug interactions. Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine. Valproate has been shown to decrease the apparent clearance of lamotrigine.Discontinuation of Psychotropic Drugs (excluding Valproate , Carbamazepine, or Other Enzyme-Inducing Drugs )After Discontinuation of Valproate After Discontinuation of Carbamazepine or Other Enzyme-Inducing Drugs Current Lamotrigine dose (mg/day) 100Current Lamotrigine dose (mg/day) 400Week 1Maintain current lamotrigine dose150400Week 2Maintain current lamotrigine dose200300Week 3 onwardMaintain current lamotrigine dose200200There is no body of evidence available to answer the question of how long the patient should remain on lamotrigine therapy. Systematic evaluation of the efficacy of lamotrigine in patients with either depression or mania who responded to standard therapy during an acute 8 to 16 week treatment phase and were then randomized to lamotrigine or placebo for up to 76 weeks of observation for affective relapse demonstrated a benefit of such maintenance treatment (see CLINICAL STUDIES: Bipolar Disorder). Nevertheless, patients should be periodically reassessed to determine the need for maintenance treatment.
Discontinuation Strategy in Bipolar Disorder:
As with other AEDs, lamotrigine should not be abruptly discontinued. In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse experiences following abrupt termination of lamotrigine. In clinical trials in patients with bipolar disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal.
Administration of Lamotrigine Tablets (Chewable, Dispersible)
Lamotrigine tablets (Chewable, Dispersible) may be swallowed whole, chewed, or dispersed in water or diluted fruit juice. If the tablets are chewed, consume a small amount of water or diluted fruit juice to aid in swallowing.
To disperse lamotrigine tablets (chewable, dispersible), add the tablets to a small amount of liquid (1 teaspoon, or enough to cover the medication). Approximately 1 minute later, when the tablets are completely dispersed, swirl the solution and consume the entire quantity immediately.
No attempt should be made to administer partial quantities of the dispersed tablets.
-
Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ] Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Epilepsy
Adjunctive Use:
Lamotrigine is indicated as adjunctive therapy for partial seizures and the generalized seizures of Lennox-Gastaut syndrome in adult and pediatric patients (years of age).
Monotherapy Use:
Lamotrigine tablets and lamotrigine tablets (chewable, dispersible) are indicated for conversion to monotherapy in adults with partial seizures who are receiving treatment with carbamazepine, phenytoin, phenobarbital, primidone, or valproate as the single AED.
Safety and effectiveness of lamotrigine tablets and lamotrigine tablets (chewable, dispersible)have not been established. (1) as initial monotherapy, (2) for conversion to monotherapy from AEDs other than carbamazepine, phenytoin, phenobarbital, primidone, or valproate, or (3) for simultaneous conversion to monotherapy from 2 or more concomitant AEDs.
Bipolar Disorder
Lamotrigine tablets and lamotrigine tablets (chewable, dispersible) are indicated for the maintenance treatment of Bipolar I Disorder to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The effectiveness of lamotrigine in the acute treatment of mood episodes has not been established.
General Dosing Considerations for Epilepsy and Bipolar Disorder Patients:
The risk of nonserious rash is increased when the recommended initial dose and/or the rate of dose escalation of Lamotrigine is exceeded. There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have been reported in the absence of these factors (see BOX WARNING). Therefore, it is important that the dosing recommendations be followed closely.
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed.
Lamotrigine Tablets and Lamotrigine Tablets (Chewable, Dispersible)Added to Drugs Known to Induce or Inhibit Glucuronidation:
Drugs other than those listed in PRECAUTIONS: Drug Interactionshave not been systematically evaluated in
combination with Lamotrigine. Since lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine, and doses of Lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder:
A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response.
The half-life of lamotrigine is affected by other concomitant medications (see CLINICAL PHARMACOLOGY: Pharmacokinetics and Drug Metabolism).
See also DOSAGE AND ADMINISTRATION: Special Populations.
Special Populations: Women and Oral Contraceptives: Starting Lamotrigine Tablets and LamotrigineTablets (Chewable, Dispersible)in Women Taking Oral Contraceptives
Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine (see PRECAUTIONS: Drug Interactions), no adjustments to the recommended dose escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED (see Table 11). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets and Lamotrigine Tablets (Chewable, Dispersible)
Taking Estrogen-Containing Oral Contraceptives:
For women not taking carbamazepine, phenytoin, phenobarbital, primidone,
or rifampin, the maintenance dose of Lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level (see PRECAUTIONS: Drug Interactions). (2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of Lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose will in most cases need to be increased by as much as 2-fold, in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate unless lamotrigine plasma levels or clinical response support larger increases (see Table 11, column 2,). Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse events, such as dizziness, ataxia, and diplopia (see PRECAUTIONS: Drug Interactions). If adverse events attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment should be necessary to the dose of Lamotrigine. (3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50%, in order to maintain a consistent lamotrigine plasma level. The decrease in dose of Lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise (see PRECAUTIONS: Drug Interactions). For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy:
The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment:
Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver dysfunction (see CLINICAL PHARMACOLOGY), the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without
ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Functional Impairment:
Initial doses of lamotrigine tablets and lamotrigine tablets (chewable, dispersible) should be based on patients' AED regimen (see above); reduced maintenance doses may be effective for patients with significant renal functional impairment (see CLINICAL PHARMACOLOGY). Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Epilepsy:
Adjunctive Therapy With Lamotrigine Tablets and Lamotrigine Tablets (Chewable, Dispersible) for Epilepsy:
This section provides specific dosing recommendations for patients 2 to 12 years of age and patients greater than 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED (Table 9 for patients 2 to 12 years of age and Table 11 for patients greater than 12 years of age). A weight based dosing guide for pediatric patients on concomitant valproate is provided in Table 10.
Patients 2 to 12 Years of Age:
Recommended dosing guidelines are summarized in Table 9.
Note that some of the starting doses and dose escalations listed in Table 9 are different than those used in clinical trials; however, the maintenance doses are the same as in clinical trials. Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestions that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 9. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy
*Rifampin and estrogen-containing oral contraceptives have also been shown to increase the apparent clearance of lamotrigine (see PRECAUTIONS: Drug Interactions).For Patients Taking Valproate (see Table 10 for weight- based dosing guide)For Patients Taking AEDs Other Than Carbamazepine, Phenytoi n, Phenobarbital, Primidone *, or ValproateFor Patients Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone *and Not Taking ValproateWeeks 1 and 20.15 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 10 for weight-based dosing guide).0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet.0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet.Weeks 3 and 40.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 10 for weight-based dosing guide).0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet.1.2 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet.Weeks 5 onwards to maintenanceThe dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose.The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily doseThe dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily doseUsual Maintenance Dose1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses). 1 to 3 mg/kg/day with valproate alone4.5 to 7.5 mg/kg/day (maximum 300 mg/day in 2 divided doses)5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses)Maintenance dose in patients less than 30 kgMay need to be increased by as much as 50%, based on clinical responseMay need to be increased by as much as 50%, based on clinical responseMay need to be increased by as much as 50%, based on clinical responseNote: Only whole tablets should be used for dosing
Table 10. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy
If the patient's weight isGive this daily dose, using the most appropriate combination of lamotrigine tablets (chewable, dispersible), 5 mgGreater thanAnd less thanWeeks 1 and 2Weeks 3 and 434.1 kg40 kg5 mg every day10 mg every dayPatients Over 12 Years of Age:
Recommended dosing guidelines are summarized in Table 11.
Table 11. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy
*Rifampin and estrogen-containing oral contraceptives have also been shown to increase the apparent clearance of lamotrigine (see PRECAUTIONS: Drug Interactions).For Patients Taking ValproateFor Patients Taking AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate *For Patients Taking Carbamazepine, Phenytoin, PhenobarbitaL, Primidone *and Not Taking ValproateWeeks 1 and 225 mg every other day25 mg every day50 mg/dayWeeks 3 and 425 mg every day50 mg/day100 mg/day (in 2 divided doses)Weeks 5 onwards to maintenanceIncrease by 25 to 50 mg/ day every 1 to 2 weeksIncrease by 50 mg/ day every 1 to 2 weeksIncrease by 100 mg/ day every 1 to 2 weeks.Usual Maintenance Dose100 to 400 mg/day (1 or 2 divided doses) 100 to 200 mg/day with Valproate alone225 to 375 mg/day (in 2 divided doses).300 to 500 mg/day (in 2 divided doses).Conversion from Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate as the Single AED to Monotherapy With Lamotrigine in PatientsYears of Age With Epilepsy:
The goal of the transition regimen is to effect the conversion to monotherapy with Lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded (see BOX WARNING).
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine:
After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 11, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine The conversion regimen involves 4 steps (see Table 12).
Table 12. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in PatientsYears of Age With Epilepsy
LamotrigineValproateStep 1Achieve a dose of 200 mg/day according to guidelines in Table 11 (if not already on 200 mg/ day).Maintain previous stable dose.Step 2Maintain at 200 mg/day.Decrease to 500 mg/day by decrements no greater than 500 mg/day per week and then maintain the dose of 500 mg/day for 1 week.Step 3Increase to 300 mg/day and maintain for 1 week.Simultaneously decrease to 250 mg/day and maintain for 1 week.Step 4Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.Discontinue.Conversion from Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine:
No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
Usual Maintenance Dose for Epilepsy
The usual maintenance doses identified in Tables 9-11 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive Lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive Lamotrigine as high as 200 mg/ day have been used. The advantage of using doses above those recommended in Tables 9-12 has not been established in controlled trials.
Discontinuation Strategy for Patients With Epilepsy:
For patients receiving lamotrigine in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse experiences is observed.
If a decision is made to discontinue therapy with Lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal (see PRECAUTIONS).
Discontinuing carbamazepine, phenytoin, phenobarbital, or primidone should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder
The goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate,which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, which increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated, however, no additional benefit was seen at 400 mg/day compared to 200 mg/day (see CLINICAL STUDIES: Bipolar Disorder). Accordingly, doses above 200 mg/ day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 13. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 14). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 14). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
Dosage adjustments will be necessary in most patients who start or stop estrogen-containing oral contraceptives while taking lamotrigine (see DOSAGE AND ADMINISTRATION: Special Populations: Women and Oral Contraceptives: Adjustments to the Maintenace Dose of Lamotrigine).
If other drugs are subsequently introduced, the dose of Lamotrigine may need to be adjusted.
In particular, the introduction of valproate requires reduction in the dose of Lamotrigine (see CLINICAL PHARMACOLOGY: Drug Interactions). To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded (see BOX WARNING).
Table 13. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder *
*See CLINICAL PHARMACOLOGY: Drug Interactions:and PRECAUTIONS: Drug Interactionsfor a description of known drug interactions. Carbamazepine, phenytoin, phenobarbital, primidone, rifampin, have been shown to increase the apparent clearance of lamotrigine. Valproate has been shown to decrease the apparent clearance of lamotrigine.For Patients Not Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone or Rifampin and Not Taking Valproate For Patients Taking Valproate For Patients Taking Carbamazepine (or Other Enzyme-Inducing Drugs) and Not Taking Valproate Weeks 1 and 225 mg daily25 mg every other day50 mg dailyWeeks 3 and 450 mg daily25 mg daily100 mg daily, in divided dosesWeek 5100 mg daily50 mg daily200 mg daily, in divided dosesWeek 6200 mg daily100 mg daily300 mg daily, in divided dosesWeek 7200 mg daily100 mg dailyup to 400 mg daily, in divided doses
Table 14. Adjustments to Lamotrigine Dosing for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications *
*See CLINICAL PHARMACOLOGY: Drug Interactions:and PRECAUTIONS: Drug Interactionsfor a description of known drug interactions. Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine. Valproate has been shown to decrease the apparent clearance of lamotrigine.Discontinuation of Psychotropic Drugs (excluding Valproate , Carbamazepine, or Other Enzyme-Inducing Drugs )After Discontinuation of Valproate After Discontinuation of Carbamazepine or Other Enzyme-Inducing Drugs Current Lamotrigine dose (mg/day) 100Current Lamotrigine dose (mg/day) 400Week 1Maintain current lamotrigine dose150400Week 2Maintain current lamotrigine dose200300Week 3 onwardMaintain current lamotrigine dose200200There is no body of evidence available to answer the question of how long the patient should remain on lamotrigine therapy. Systematic evaluation of the efficacy of lamotrigine in patients with either depression or mania who responded to standard therapy during an acute 8 to 16 week treatment phase and were then randomized to lamotrigine or placebo for up to 76 weeks of observation for affective relapse demonstrated a benefit of such maintenance treatment (see CLINICAL STUDIES: Bipolar Disorder). Nevertheless, patients should be periodically reassessed to determine the need for maintenance treatment.
Discontinuation Strategy in Bipolar Disorder:
As with other AEDs, lamotrigine should not be abruptly discontinued. In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse experiences following abrupt termination of lamotrigine. In clinical trials in patients with bipolar disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal.
Administration of Lamotrigine Tablets (Chewable, Dispersible)
Lamotrigine tablets (Chewable, Dispersible) may be swallowed whole, chewed, or dispersed in water or diluted fruit juice. If the tablets are chewed, consume a small amount of water or diluted fruit juice to aid in swallowing.
To disperse lamotrigine tablets (chewable, dispersible), add the tablets to a small amount of liquid (1 teaspoon, or enough to cover the medication). Approximately 1 minute later, when the tablets are completely dispersed, swirl the solution and consume the entire quantity immediately.
No attempt should be made to administer partial quantities of the dispersed tablets.
-
Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ] Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Epilepsy
Adjunctive Use:
Lamotrigine is indicated as adjunctive therapy for partial seizures and the generalized seizures of Lennox-Gastaut syndrome in adult and pediatric patients (years of age).
Monotherapy Use:
Lamotrigine tablets and lamotrigine tablets (chewable, dispersible) are indicated for conversion to monotherapy in adults with partial seizures who are receiving treatment with carbamazepine, phenytoin, phenobarbital, primidone, or valproate as the single AED.
Safety and effectiveness of lamotrigine tablets and lamotrigine tablets (chewable, dispersible)have not been established. (1) as initial monotherapy, (2) for conversion to monotherapy from AEDs other than carbamazepine, phenytoin, phenobarbital, primidone, or valproate, or (3) for simultaneous conversion to monotherapy from 2 or more concomitant AEDs.
Bipolar Disorder
Lamotrigine tablets and lamotrigine tablets (chewable, dispersible) are indicated for the maintenance treatment of Bipolar I Disorder to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The effectiveness of lamotrigine in the acute treatment of mood episodes has not been established.
General Dosing Considerations for Epilepsy and Bipolar Disorder Patients:
The risk of nonserious rash is increased when the recommended initial dose and/or the rate of dose escalation of Lamotrigine is exceeded. There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have been reported in the absence of these factors (see BOX WARNING). Therefore, it is important that the dosing recommendations be followed closely.
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed.
Lamotrigine Tablets and Lamotrigine Tablets (Chewable, Dispersible)Added to Drugs Known to Induce or Inhibit Glucuronidation:
Drugs other than those listed in PRECAUTIONS: Drug Interactionshave not been systematically evaluated in
combination with Lamotrigine. Since lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine, and doses of Lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder:
A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response.
The half-life of lamotrigine is affected by other concomitant medications (see CLINICAL PHARMACOLOGY: Pharmacokinetics and Drug Metabolism).
See also DOSAGE AND ADMINISTRATION: Special Populations.
Special Populations: Women and Oral Contraceptives: Starting Lamotrigine Tablets and LamotrigineTablets (Chewable, Dispersible)in Women Taking Oral Contraceptives
Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine (see PRECAUTIONS: Drug Interactions), no adjustments to the recommended dose escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED (see Table 11). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets and Lamotrigine Tablets (Chewable, Dispersible)
1. Taking Estrogen-Containing Oral Contraceptives:
For women not taking carbamazepine, phenytoin, phenobarbital, primidone,
or rifampin, the maintenance dose of Lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level (see PRECAUTIONS: Drug Interactions). (2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of Lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose will in most cases need to be increased by as much as 2-fold, in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate unless lamotrigine plasma levels or clinical response support larger increases (see Table 11, column 2,). Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse events, such as dizziness, ataxia, and diplopia (see PRECAUTIONS: Drug Interactions). If adverse events attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment should be necessary to the dose of Lamotrigine. (3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50%, in order to maintain a consistent lamotrigine plasma level. The decrease in dose of Lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise (see PRECAUTIONS: Drug Interactions). For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy:
The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment:
Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver dysfunction (see CLINICAL PHARMACOLOGY), the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without
ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Functional Impairment:
Initial doses of lamotrigine tablets and lamotrigine tablets (chewable, dispersible) should be based on patients' AED regimen (see above); reduced maintenance doses may be effective for patients with significant renal functional impairment (see CLINICAL PHARMACOLOGY). Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Epilepsy:
Adjunctive Therapy With Lamotrigine Tablets and Lamotrigine Tablets (Chewable, Dispersible) for Epilepsy:
This section provides specific dosing recommendations for patients 2 to 12 years of age and patients greater than 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED (Table 9 for patients 2 to 12 years of age and Table 11 for patients greater than 12 years of age). A weight based dosing guide for pediatric patients on concomitant valproate is provided in Table 10.
Patients 2 to 12 Years of Age:
Recommended dosing guidelines are summarized in Table 9.
Note that some of the starting doses and dose escalations listed in Table 9 are different than those used in clinical trials; however, the maintenance doses are the same as in clinical trials. Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestions that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 9. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy
*Rifampin and estrogen-containing oral contraceptives have also been shown to increase the apparent clearance of lamotrigine (see PRECAUTIONS: Drug Interactions).For Patients Taking Valproate (see Table 10 for weight- based dosing guide)For Patients Taking AEDs Other Than Carbamazepine, Phenytoi n, Phenobarbital, Primidone *, or ValproateFor Patients Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone *and Not Taking ValproateWeeks 1 and 20.15 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 10 for weight-based dosing guide).0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet.0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet.Weeks 3 and 40.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 10 for weight-based dosing guide).0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet.1.2 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet.Weeks 5 onwards to maintenanceThe dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose.The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily doseThe dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily doseUsual Maintenance Dose1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses). 1 to 3 mg/kg/day with valproate alone4.5 to 7.5 mg/kg/day (maximum 300 mg/day in 2 divided doses)5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses)Maintenance dose in patients less than 30 kgMay need to be increased by as much as 50%, based on clinical responseMay need to be increased by as much as 50%, based on clinical responseMay need to be increased by as much as 50%, based on clinical responseNote: Only whole tablets should be used for dosing
Table 10. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy
If the patient's weight isGive this daily dose, using the most appropriate combination of lamotrigine tablets (chewable, dispersible), 5 mgGreater thanAnd less thanWeeks 1 and 2Weeks 3 and 434.1 kg40 kg5 mg every day10 mg every dayPatients Over 12 Years of Age:
Recommended dosing guidelines are summarized in Table 11.
Table 11. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy
*Rifampin and estrogen-containing oral contraceptives have also been shown to increase the apparent clearance of lamotrigine (see PRECAUTIONS: Drug Interactions).For Patients Taking ValproateFor Patients Taking AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate *For Patients Taking Carbamazepine, Phenytoin, PhenobarbitaL, Primidone *and Not Taking ValproateWeeks 1 and 225 mg every other day25 mg every day50 mg/dayWeeks 3 and 425 mg every day50 mg/day100 mg/day (in 2 divided doses)Weeks 5 onwards to maintenanceIncrease by 25 to 50 mg/ day every 1 to 2 weeksIncrease by 50 mg/ day every 1 to 2 weeksIncrease by 100 mg/ day every 1 to 2 weeks.Usual Maintenance Dose100 to 400 mg/day (1 or 2 divided doses) 100 to 200 mg/day with Valproate alone225 to 375 mg/day (in 2 divided doses).300 to 500 mg/day (in 2 divided doses). Conversion from Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate as the Single AED to Monotherapy With Lamotrigine in PatientsYears of Age With Epilepsy:
The goal of the transition regimen is to effect the conversion to monotherapy with Lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded (see BOX WARNING).
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine:
After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 11, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With LamotrigineThe conversion regimen involves 4 steps (see Table 12).
Table 12. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in PatientsYears of Age With Epilepsy
LamotrigineValproateStep 1Achieve a dose of 200 mg/day according to guidelines in Table 11 (if not already on 200 mg/ day).Maintain previous stable dose.Step 2Maintain at 200 mg/day.Decrease to 500 mg/day by decrements no greater than 500 mg/day per week and then maintain the dose of 500 mg/day for 1 week.Step 3Increase to 300 mg/day and maintain for 1 week.Simultaneously decrease to 250 mg/day and maintain for 1 week.Step 4Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.Discontinue. Conversion from Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine:
No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
Usual Maintenance Dose for Epilepsy
The usual maintenance doses identified in Tables 9-11 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive Lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive Lamotrigine as high as 200 mg/ day have been used. The advantage of using doses above those recommended in Tables 9-12 has not been established in controlled trials.
Discontinuation Strategy for Patients With Epilepsy:
For patients receiving lamotrigine in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse experiences is observed.
If a decision is made to discontinue therapy with Lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal (see PRECAUTIONS).
Discontinuing carbamazepine, phenytoin, phenobarbital, or primidone should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder
The goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate,which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, which increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated, however, no additional benefit was seen at 400 mg/day compared to 200 mg/day (see CLINICAL STUDIES: Bipolar Disorder). Accordingly, doses above 200 mg/ day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 13. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 14). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 14). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
Dosage adjustments will be necessary in most patients who start or stop estrogen-containing oral contraceptives while taking lamotrigine (see DOSAGE AND ADMINISTRATION: Special Populations: Women and Oral Contraceptives: Adjustments to the Maintenace Dose of Lamotrigine).
If other drugs are subsequently introduced, the dose of Lamotrigine may need to be adjusted.
In particular, the introduction of valproate requires reduction in the dose of Lamotrigine (see CLINICAL PHARMACOLOGY: Drug Interactions). To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded (see BOX WARNING).
Table 13. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder*
*See CLINICAL PHARMACOLOGY: Drug Interactions:and PRECAUTIONS: Drug Interactionsfor a description of known drug interactions. Carbamazepine, phenytoin, phenobarbital, primidone, rifampin, have been shown to increase the apparent clearance of lamotrigine. Valproate has been shown to decrease the apparent clearance of lamotrigine.For Patients Not Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone or Rifampin and Not Taking Valproate For Patients Taking Valproate For Patients Taking Carbamazepine (or Other Enzyme-Inducing Drugs) and Not Taking Valproate Weeks 1 and 225 mg daily25 mg every other day50 mg dailyWeeks 3 and 450 mg daily25 mg daily100 mg daily, in divided dosesWeek 5100 mg daily50 mg daily200 mg daily, in divided dosesWeek 6200 mg daily100 mg daily300 mg daily, in divided dosesWeek 7200 mg daily100 mg dailyup to 400 mg daily, in divided doses
Table 14. Adjustments to Lamotrigine Dosing for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications *
*See CLINICAL PHARMACOLOGY: Drug Interactions:and PRECAUTIONS: Drug Interactionsfor a description of known drug interactions. Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine. Valproate has been shown to decrease the apparent clearance of lamotrigine.Discontinuation of Psychotropic Drugs (excluding Valproate , Carbamazepine, or Other Enzyme-Inducing Drugs )After Discontinuation of Valproate After Discontinuation of Carbamazepine or Other Enzyme-Inducing Drugs Current Lamotrigine dose (mg/day) 100Current Lamotrigine dose (mg/day) 400Week 1Maintain current lamotrigine dose150400Week 2Maintain current lamotrigine dose200300Week 3 onwardMaintain current lamotrigine dose200200There is no body of evidence available to answer the question of how long the patient should remain on lamotrigine therapy. Systematic evaluation of the efficacy of lamotrigine in patients with either depression or mania who responded to standard therapy during an acute 8 to 16 week treatment phase and were then randomized to lamotrigine or placebo for up to 76 weeks of observation for affective relapse demonstrated a benefit of such maintenance treatment (see CLINICAL STUDIES: Bipolar Disorder). Nevertheless, patients should be periodically reassessed to determine the need for maintenance treatment.
Discontinuation Strategy in Bipolar Disorder:
As with other AEDs, lamotrigine should not be abruptly discontinued. In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse experiences following abrupt termination of lamotrigine. In clinical trials in patients with bipolar disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal.
Administration of Lamotrigine Tablets (Chewable, Dispersible)
Lamotrigine tablets (Chewable, Dispersible) may be swallowed whole, chewed, or dispersed in water or diluted fruit juice. If the tablets are chewed, consume a small amount of water or diluted fruit juice to aid in swallowing.
To disperse lamotrigine tablets (chewable, dispersible), add the tablets to a small amount of liquid (1 teaspoon, or enough to cover the medication). Approximately 1 minute later, when the tablets are completely dispersed, swirl the solution and consume the entire quantity immediately.
No attempt should be made to administer partial quantities of the dispersed tablets.
-
Remedyrepack Inc.
![Lamotrigine Tablet, Chewable [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Remedyrepack Inc.
![Lamotrigine Tablet, Chewable [Remedyrepack Inc. ] Lamotrigine Tablet, Chewable [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Epilepsy
Adjunctive Use:
Lamotrigine is indicated as adjunctive therapy for partial seizures and the generalized seizures of Lennox-Gastaut syndrome in adult and pediatric patients (years of age).
Monotherapy Use:
Lamotrigine tablets and lamotrigine tablets (chewable, dispersible) are indicated for conversion to monotherapy in adults with partial seizures who are receiving treatment with carbamazepine, phenytoin, phenobarbital, primidone, or valproate as the single AED.
Safety and effectiveness of lamotrigine tablets and lamotrigine tablets (chewable, dispersible)have not been established. (1) as initial monotherapy, (2) for conversion to monotherapy from AEDs other than carbamazepine, phenytoin, phenobarbital, primidone, or valproate, or (3) for simultaneous conversion to monotherapy from 2 or more concomitant AEDs.
Bipolar Disorder
Lamotrigine tablets and lamotrigine tablets (chewable, dispersible) are indicated for the maintenance treatment of Bipolar I Disorder to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The effectiveness of lamotrigine in the acute treatment of mood episodes has not been established.
General Dosing Considerations for Epilepsy and Bipolar Disorder Patients:
The risk of nonserious rash is increased when the recommended initial dose and/or the rate of dose escalation of Lamotrigine is exceeded. There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have been reported in the absence of these factors (see BOX WARNING). Therefore, it is important that the dosing recommendations be followed closely.
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed.
Lamotrigine Tablets and Lamotrigine Tablets (Chewable, Dispersible)Added to Drugs Known to Induce or Inhibit Glucuronidation:
Drugs other than those listed in PRECAUTIONS: Drug Interactionshave not been systematically evaluated in
combination with Lamotrigine. Since lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine, and doses of Lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder:
A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response.
The half-life of lamotrigine is affected by other concomitant medications (see CLINICAL PHARMACOLOGY: Pharmacokinetics and Drug Metabolism).
See also DOSAGE AND ADMINISTRATION: Special Populations.
Special Populations: Women and Oral Contraceptives: Starting Lamotrigine Tablets and LamotrigineTablets (Chewable, Dispersible)in Women Taking Oral Contraceptives
Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine (see PRECAUTIONS: Drug Interactions), no adjustments to the recommended dose escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED (see Table 11). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets and Lamotrigine Tablets (Chewable, Dispersible)
Taking Estrogen-Containing Oral Contraceptives:
For women not taking carbamazepine, phenytoin, phenobarbital, primidone,
or rifampin, the maintenance dose of Lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level (see PRECAUTIONS: Drug Interactions). (2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of Lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose will in most cases need to be increased by as much as 2-fold, in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate unless lamotrigine plasma levels or clinical response support larger increases (see Table 11, column 2,). Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse events, such as dizziness, ataxia, and diplopia (see PRECAUTIONS: Drug Interactions). If adverse events attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment should be necessary to the dose of Lamotrigine. (3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50%, in order to maintain a consistent lamotrigine plasma level. The decrease in dose of Lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise (see PRECAUTIONS: Drug Interactions). For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy:
The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment:
Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver dysfunction (see CLINICAL PHARMACOLOGY), the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without
ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Functional Impairment:
Initial doses of lamotrigine tablets and lamotrigine tablets (chewable, dispersible) should be based on patients' AED regimen (see above); reduced maintenance doses may be effective for patients with significant renal functional impairment (see CLINICAL PHARMACOLOGY). Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Epilepsy:
Adjunctive Therapy With Lamotrigine Tablets and Lamotrigine Tablets (Chewable, Dispersible) for Epilepsy:
This section provides specific dosing recommendations for patients 2 to 12 years of age and patients greater than 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED (Table 9 for patients 2 to 12 years of age and Table 11 for patients greater than 12 years of age). A weight based dosing guide for pediatric patients on concomitant valproate is provided in Table 10.
Patients 2 to 12 Years of Age:
Recommended dosing guidelines are summarized in Table 9.
Note that some of the starting doses and dose escalations listed in Table 9 are different than those used in clinical trials; however, the maintenance doses are the same as in clinical trials. Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestions that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 9. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy
*Rifampin and estrogen-containing oral contraceptives have also been shown to increase the apparent clearance of lamotrigine (see PRECAUTIONS: Drug Interactions).For Patients Taking Valproate (see Table 10 for weight- based dosing guide)For Patients Taking AEDs Other Than Carbamazepine, Phenytoi n, Phenobarbital, Primidone *, or ValproateFor Patients Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone *and Not Taking ValproateWeeks 1 and 20.15 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 10 for weight-based dosing guide).0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet.0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet.Weeks 3 and 40.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 10 for weight-based dosing guide).0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet.1.2 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet.Weeks 5 onwards to maintenanceThe dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose.The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily doseThe dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily doseUsual Maintenance Dose1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses). 1 to 3 mg/kg/day with valproate alone4.5 to 7.5 mg/kg/day (maximum 300 mg/day in 2 divided doses)5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses)Maintenance dose in patients less than 30 kgMay need to be increased by as much as 50%, based on clinical responseMay need to be increased by as much as 50%, based on clinical responseMay need to be increased by as much as 50%, based on clinical responseNote: Only whole tablets should be used for dosing
Table 10. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy
If the patient's weight isGive this daily dose, using the most appropriate combination of lamotrigine tablets (chewable, dispersible), 5 mgGreater thanAnd less thanWeeks 1 and 2Weeks 3 and 434.1 kg40 kg5 mg every day10 mg every dayPatients Over 12 Years of Age:
Recommended dosing guidelines are summarized in Table 11.
Table 11. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy
*Rifampin and estrogen-containing oral contraceptives have also been shown to increase the apparent clearance of lamotrigine (see PRECAUTIONS: Drug Interactions).For Patients Taking ValproateFor Patients Taking AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate *For Patients Taking Carbamazepine, Phenytoin, PhenobarbitaL, Primidone *and Not Taking ValproateWeeks 1 and 225 mg every other day25 mg every day50 mg/dayWeeks 3 and 425 mg every day50 mg/day100 mg/day (in 2 divided doses)Weeks 5 onwards to maintenanceIncrease by 25 to 50 mg/ day every 1 to 2 weeksIncrease by 50 mg/ day every 1 to 2 weeksIncrease by 100 mg/ day every 1 to 2 weeks.Usual Maintenance Dose100 to 400 mg/day (1 or 2 divided doses) 100 to 200 mg/day with Valproate alone225 to 375 mg/day (in 2 divided doses).300 to 500 mg/day (in 2 divided doses).Conversion from Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate as the Single AED to Monotherapy With Lamotrigine in PatientsYears of Age With Epilepsy:
The goal of the transition regimen is to effect the conversion to monotherapy with Lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded (see BOX WARNING).
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine:
After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 11, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine The conversion regimen involves 4 steps (see Table 12).
Table 12. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in PatientsYears of Age With Epilepsy
LamotrigineValproateStep 1Achieve a dose of 200 mg/day according to guidelines in Table 11 (if not already on 200 mg/ day).Maintain previous stable dose.Step 2Maintain at 200 mg/day.Decrease to 500 mg/day by decrements no greater than 500 mg/day per week and then maintain the dose of 500 mg/day for 1 week.Step 3Increase to 300 mg/day and maintain for 1 week.Simultaneously decrease to 250 mg/day and maintain for 1 week.Step 4Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.Discontinue.Conversion from Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine:
No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
Usual Maintenance Dose for Epilepsy
The usual maintenance doses identified in Tables 9-11 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive Lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive Lamotrigine as high as 200 mg/ day have been used. The advantage of using doses above those recommended in Tables 9-12 has not been established in controlled trials.
Discontinuation Strategy for Patients With Epilepsy:
For patients receiving lamotrigine in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse experiences is observed.
If a decision is made to discontinue therapy with Lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal (see PRECAUTIONS).
Discontinuing carbamazepine, phenytoin, phenobarbital, or primidone should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder
The goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate,which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, which increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated, however, no additional benefit was seen at 400 mg/day compared to 200 mg/day (see CLINICAL STUDIES: Bipolar Disorder). Accordingly, doses above 200 mg/ day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 13. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 14). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 14). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
Dosage adjustments will be necessary in most patients who start or stop estrogen-containing oral contraceptives while taking lamotrigine (see DOSAGE AND ADMINISTRATION: Special Populations: Women and Oral Contraceptives: Adjustments to the Maintenace Dose of Lamotrigine).
If other drugs are subsequently introduced, the dose of Lamotrigine may need to be adjusted.
In particular, the introduction of valproate requires reduction in the dose of Lamotrigine (see CLINICAL PHARMACOLOGY: Drug Interactions). To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded (see BOX WARNING).
Table 13. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder *
*See CLINICAL PHARMACOLOGY: Drug Interactions:and PRECAUTIONS: Drug Interactionsfor a description of known drug interactions. Carbamazepine, phenytoin, phenobarbital, primidone, rifampin, have been shown to increase the apparent clearance of lamotrigine. Valproate has been shown to decrease the apparent clearance of lamotrigine.For Patients Not Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone or Rifampin and Not Taking Valproate For Patients Taking Valproate For Patients Taking Carbamazepine (or Other Enzyme-Inducing Drugs) and Not Taking Valproate Weeks 1 and 225 mg daily25 mg every other day50 mg dailyWeeks 3 and 450 mg daily25 mg daily100 mg daily, in divided dosesWeek 5100 mg daily50 mg daily200 mg daily, in divided dosesWeek 6200 mg daily100 mg daily300 mg daily, in divided dosesWeek 7200 mg daily100 mg dailyup to 400 mg daily, in divided doses
Table 14. Adjustments to Lamotrigine Dosing for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications *
*See CLINICAL PHARMACOLOGY: Drug Interactions:and PRECAUTIONS: Drug Interactionsfor a description of known drug interactions. Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine. Valproate has been shown to decrease the apparent clearance of lamotrigine.Discontinuation of Psychotropic Drugs (excluding Valproate , Carbamazepine, or Other Enzyme-Inducing Drugs )After Discontinuation of Valproate After Discontinuation of Carbamazepine or Other Enzyme-Inducing Drugs Current Lamotrigine dose (mg/day) 100Current Lamotrigine dose (mg/day) 400Week 1Maintain current lamotrigine dose150400Week 2Maintain current lamotrigine dose200300Week 3 onwardMaintain current lamotrigine dose200200There is no body of evidence available to answer the question of how long the patient should remain on lamotrigine therapy. Systematic evaluation of the efficacy of lamotrigine in patients with either depression or mania who responded to standard therapy during an acute 8 to 16 week treatment phase and were then randomized to lamotrigine or placebo for up to 76 weeks of observation for affective relapse demonstrated a benefit of such maintenance treatment (see CLINICAL STUDIES: Bipolar Disorder). Nevertheless, patients should be periodically reassessed to determine the need for maintenance treatment.
Discontinuation Strategy in Bipolar Disorder:
As with other AEDs, lamotrigine should not be abruptly discontinued. In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse experiences following abrupt termination of lamotrigine. In clinical trials in patients with bipolar disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal.
Administration of Lamotrigine Tablets (Chewable, Dispersible)
Lamotrigine tablets (Chewable, Dispersible) may be swallowed whole, chewed, or dispersed in water or diluted fruit juice. If the tablets are chewed, consume a small amount of water or diluted fruit juice to aid in swallowing.
To disperse lamotrigine tablets (chewable, dispersible), add the tablets to a small amount of liquid (1 teaspoon, or enough to cover the medication). Approximately 1 minute later, when the tablets are completely dispersed, swirl the solution and consume the entire quantity immediately.
No attempt should be made to administer partial quantities of the dispersed tablets.
-
Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ] Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Epilepsy
Adjunctive Use:
Lamotrigine is indicated as adjunctive therapy for partial seizures and the generalized seizures of Lennox-Gastaut syndrome in adult and pediatric patients (years of age).
Monotherapy Use:
Lamotrigine tablets and lamotrigine tablets (chewable, dispersible) are indicated for conversion to monotherapy in adults with partial seizures who are receiving treatment with carbamazepine, phenytoin, phenobarbital, primidone, or valproate as the single AED.
Safety and effectiveness of lamotrigine tablets and lamotrigine tablets (chewable, dispersible)have not been established. (1) as initial monotherapy, (2) for conversion to monotherapy from AEDs other than carbamazepine, phenytoin, phenobarbital, primidone, or valproate, or (3) for simultaneous conversion to monotherapy from 2 or more concomitant AEDs.
Bipolar Disorder
Lamotrigine tablets and lamotrigine tablets (chewable, dispersible) are indicated for the maintenance treatment of Bipolar I Disorder to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The effectiveness of lamotrigine in the acute treatment of mood episodes has not been established.
General Dosing Considerations for Epilepsy and Bipolar Disorder Patients:
The risk of nonserious rash is increased when the recommended initial dose and/or the rate of dose escalation of Lamotrigine is exceeded. There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have been reported in the absence of these factors (see BOX WARNING). Therefore, it is important that the dosing recommendations be followed closely.
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed.
Lamotrigine Tablets and Lamotrigine Tablets (Chewable, Dispersible)Added to Drugs Known to Induce or Inhibit Glucuronidation:
Drugs other than those listed in PRECAUTIONS: Drug Interactionshave not been systematically evaluated in
combination with Lamotrigine. Since lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine, and doses of Lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder:
A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response.
The half-life of lamotrigine is affected by other concomitant medications (see CLINICAL PHARMACOLOGY: Pharmacokinetics and Drug Metabolism).
See also DOSAGE AND ADMINISTRATION: Special Populations.
Special Populations: Women and Oral Contraceptives: Starting Lamotrigine Tablets and LamotrigineTablets (Chewable, Dispersible)in Women Taking Oral Contraceptives
Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine (see PRECAUTIONS: Drug Interactions), no adjustments to the recommended dose escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED (see Table 11). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets and Lamotrigine Tablets (Chewable, Dispersible)
1. Taking Estrogen-Containing Oral Contraceptives:
For women not taking carbamazepine, phenytoin, phenobarbital, primidone,
or rifampin, the maintenance dose of Lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level (see PRECAUTIONS: Drug Interactions). (2) Starting Estrogen-Containing Oral Contraceptives:In women taking a stable dose of Lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose will in most cases need to be increased by as much as 2-fold, in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate unless lamotrigine plasma levels or clinical response support larger increases (see Table 11, column 2,). Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse events, such as dizziness, ataxia, and diplopia (see PRECAUTIONS: Drug Interactions). If adverse events attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment should be necessary to the dose of Lamotrigine. (3) Stopping Estrogen-Containing Oral Contraceptives:For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50%, in order to maintain a consistent lamotrigine plasma level. The decrease in dose of Lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise (see PRECAUTIONS: Drug Interactions). For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy:
The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment:
Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver dysfunction (see CLINICAL PHARMACOLOGY), the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without
ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Functional Impairment:
Initial doses of lamotrigine tablets and lamotrigine tablets (chewable, dispersible) should be based on patients' AED regimen (see above); reduced maintenance doses may be effective for patients with significant renal functional impairment (see CLINICAL PHARMACOLOGY). Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Epilepsy:
Adjunctive Therapy With Lamotrigine Tablets and Lamotrigine Tablets (Chewable, Dispersible) for Epilepsy:
This section provides specific dosing recommendations for patients 2 to 12 years of age and patients greater than 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED (Table 9 for patients 2 to 12 years of age and Table 11 for patients greater than 12 years of age). A weight based dosing guide for pediatric patients on concomitant valproate is provided in Table 10.
Patients 2 to 12 Years of Age:
Recommended dosing guidelines are summarized in Table 9.
Note that some of the starting doses and dose escalations listed in Table 9 are different than those used in clinical trials; however, the maintenance doses are the same as in clinical trials. Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestions that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 9. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy
*Rifampin and estrogen-containing oral contraceptives have also been shown to increase the apparent clearance of lamotrigine (see PRECAUTIONS: Drug Interactions).For Patients Taking Valproate (see Table 10 for weight- based dosing guide)For Patients Taking AEDs Other Than Carbamazepine, Phenytoi n, Phenobarbital, Primidone *, or ValproateFor Patients Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone *and Not Taking ValproateWeeks 1 and 20.15 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 10 for weight-based dosing guide).0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet.0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet.Weeks 3 and 40.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 10 for weight-based dosing guide).0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet.1.2 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet.Weeks 5 onwards to maintenanceThe dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose.The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily doseThe dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily doseUsual Maintenance Dose1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses). 1 to 3 mg/kg/day with valproate alone4.5 to 7.5 mg/kg/day (maximum 300 mg/day in 2 divided doses)5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses)Maintenance dose in patients less than 30 kgMay need to be increased by as much as 50%, based on clinical responseMay need to be increased by as much as 50%, based on clinical responseMay need to be increased by as much as 50%, based on clinical response Note: Only whole tablets should be used for dosing
Table 10. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy
If the patient's weight isGive this daily dose, using the most appropriate combination of lamotrigine tablets (chewable, dispersible), 5 mgGreater thanAnd less thanWeeks 1 and 2Weeks 3 and 434.1 kg40 kg5 mg every day10 mg every day Patients Over 12 Years of Age:
Recommended dosing guidelines are summarized in Table 11.
Table 11. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy
*Rifampin and estrogen-containing oral contraceptives have also been shown to increase the apparent clearance of lamotrigine (see PRECAUTIONS: Drug Interactions).For Patients Taking ValproateFor Patients Taking AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate *For Patients Taking Carbamazepine, Phenytoin, PhenobarbitaL, Primidone *and Not Taking ValproateWeeks 1 and 225 mg every other day25 mg every day50 mg/dayWeeks 3 and 425 mg every day50 mg/day100 mg/day (in 2 divided doses)Weeks 5 onwards to maintenanceIncrease by 25 to 50 mg/ day every 1 to 2 weeksIncrease by 50 mg/ day every 1 to 2 weeksIncrease by 100 mg/ day every 1 to 2 weeks.Usual Maintenance Dose100 to 400 mg/day (1 or 2 divided doses) 100 to 200 mg/day with Valproate alone225 to 375 mg/day (in 2 divided doses).300 to 500 mg/day (in 2 divided doses). Conversion from Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate as the Single AED to Monotherapy With Lamotrigine in PatientsYears of Age With Epilepsy:
The goal of the transition regimen is to effect the conversion to monotherapy with Lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded (see BOX WARNING).
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine:
After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 11, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With LamotrigineThe conversion regimen involves 4 steps (see Table 12).
Table 12. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in PatientsYears of Age With Epilepsy
LamotrigineValproateStep 1Achieve a dose of 200 mg/day according to guidelines in Table 11 (if not already on 200 mg/ day).Maintain previous stable dose.Step 2Maintain at 200 mg/day.Decrease to 500 mg/day by decrements no greater than 500 mg/day per week and then maintain the dose of 500 mg/day for 1 week.Step 3Increase to 300 mg/day and maintain for 1 week.Simultaneously decrease to 250 mg/day and maintain for 1 week.Step 4Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.Discontinue. Conversion from Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine:
No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
Usual Maintenance Dose for Epilepsy
The usual maintenance doses identified in Tables 9-11 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive Lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive Lamotrigine as high as 200 mg/ day have been used. The advantage of using doses above those recommended in Tables 9-12 has not been established in controlled trials.
Discontinuation Strategy for Patients With Epilepsy:
For patients receiving lamotrigine in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse experiences is observed.
If a decision is made to discontinue therapy with Lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal (see PRECAUTIONS).
Discontinuing carbamazepine, phenytoin, phenobarbital, or primidone should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder
The goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate,which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, which increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated, however, no additional benefit was seen at 400 mg/day compared to 200 mg/day (see CLINICAL STUDIES: Bipolar Disorder). Accordingly, doses above 200 mg/ day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 13. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 14). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 14). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
Dosage adjustments will be necessary in most patients who start or stop estrogen-containing oral contraceptives while taking lamotrigine (see DOSAGE AND ADMINISTRATION: Special Populations: Women and Oral Contraceptives: Adjustments to the Maintenace Dose of Lamotrigine).
If other drugs are subsequently introduced, the dose of Lamotrigine may need to be adjusted.
In particular, the introduction of valproate requires reduction in the dose of Lamotrigine (see CLINICAL PHARMACOLOGY: Drug Interactions). To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded (see BOX WARNING).
Table 13. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder *
*See CLINICAL PHARMACOLOGY: Drug Interactions:and PRECAUTIONS: Drug Interactionsfor a description of known drug interactions. Carbamazepine, phenytoin, phenobarbital, primidone, rifampin, have been shown to increase the apparent clearance of lamotrigine. Valproate has been shown to decrease the apparent clearance of lamotrigine.For Patients Not Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone or Rifampin and Not Taking Valproate For Patients Taking Valproate For Patients Taking Carbamazepine (or Other Enzyme-Inducing Drugs) and Not Taking Valproate Weeks 1 and 225 mg daily25 mg every other day50 mg dailyWeeks 3 and 450 mg daily25 mg daily100 mg daily, in divided dosesWeek 5100 mg daily50 mg daily200 mg daily, in divided dosesWeek 6200 mg daily100 mg daily300 mg daily, in divided dosesWeek 7200 mg daily100 mg dailyup to 400 mg daily, in divided doses
Table 14. Adjustments to Lamotrigine Dosing for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications *
*See CLINICAL PHARMACOLOGY: Drug Interactions:and PRECAUTIONS: Drug Interactionsfor a description of known drug interactions. Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine. Valproate has been shown to decrease the apparent clearance of lamotrigine.Discontinuation of Psychotropic Drugs (excluding Valproate , Carbamazepine, or Other Enzyme-Inducing Drugs )After Discontinuation of Valproate After Discontinuation of Carbamazepine or Other Enzyme-Inducing Drugs Current Lamotrigine dose (mg/day) 100Current Lamotrigine dose (mg/day) 400Week 1Maintain current lamotrigine dose150400Week 2Maintain current lamotrigine dose200300Week 3 onwardMaintain current lamotrigine dose200200There is no body of evidence available to answer the question of how long the patient should remain on lamotrigine therapy. Systematic evaluation of the efficacy of lamotrigine in patients with either depression or mania who responded to standard therapy during an acute 8 to 16 week treatment phase and were then randomized to lamotrigine or placebo for up to 76 weeks of observation for affective relapse demonstrated a benefit of such maintenance treatment (see CLINICAL STUDIES: Bipolar Disorder). Nevertheless, patients should be periodically reassessed to determine the need for maintenance treatment.
Discontinuation Strategy in Bipolar Disorder:
As with other AEDs, lamotrigine should not be abruptly discontinued. In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse experiences following abrupt termination of lamotrigine. In clinical trials in patients with bipolar disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal.
Administration of Lamotrigine Tablets (Chewable, Dispersible)
Lamotrigine tablets (Chewable, Dispersible) may be swallowed whole, chewed, or dispersed in water or diluted fruit juice. If the tablets are chewed, consume a small amount of water or diluted fruit juice to aid in swallowing.
To disperse lamotrigine tablets (chewable, dispersible), add the tablets to a small amount of liquid (1 teaspoon, or enough to cover the medication). Approximately 1 minute later, when the tablets are completely dispersed, swirl the solution and consume the entire quantity immediately.
No attempt should be made to administer partial quantities of the dispersed tablets.
-
West-ward Pharmaceutical Corp
![Lamotrigine Tablet [West-ward Pharmaceutical Corp]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | West-ward Pharmaceutical Corp
![Lamotrigine Tablet [West-ward Pharmaceutical Corp] Lamotrigine Tablet [West-ward Pharmaceutical Corp]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives:Starting lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives:(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (pill-free week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine consistently occur during the pill-free week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the pill-free week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy:Epilepsy: For patients receiving lamotrigine in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients aged 2 to 12 years. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients aged 2 to 12 years). A weight-based dosing guide for patients aged 2 to 12 years on concomitant valproate is provided in Table 3.
Patients Greater Than 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Greater Than 12 Years of Age With Epilepsy For Patients TAKING Valproatea For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,b or Valproatea For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day100 mg/day
(in 2 divided doses) Week 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks. Usual maintenance dose100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses)225 to 375 mg/day
(in 2 divided doses)300 to 500 mg/day
(in 2 divided doses)aValproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Patients Aged 2 to 12 Years: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients Aged 2 to 12 Years With Epilepsy For Patients TAKING Valproatea For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,b or Valproatea For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproate a Weeks 1 and 20.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide)0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet
0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet
Weeks 3 and 40.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide)0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet
1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet
Week 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual maintenance dose1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses)
1 to 3 mg/kg/day with valproate alone4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical responseNote: Only whole tablets should be used for dosing.
aValproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 3. The Initial Weight-Based Dosing Guide for Patients Aged 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of lamotrigine 2-mg and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age With Epilepsy Lamotrigine Valproate Step 1 Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day).Maintain previous stable dose.
Step 2 Maintain at 200 mg/day. Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week. Step 3 Increase to 300 mg/day and maintain for 1 week. Simultaneously decrease to 250 mg/day and maintain for 1 week. Step 4 Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day. Discontinue.Conversion From Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with LAMICTAL with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder For Patients TAKING Valproatea For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,b or Valproatea For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided dosesaValproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone,b or Valproatea) After Discontinuation of Valproatea After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or PrimidonebCurrent dose of LAMICTAL (mg/day)
100Current dose of LAMICTAL (mg/day)
400 Week 1 Maintain current dose of lamotrigine 150 400 Week 2 Maintain current dose of lamotrigine 200 300 Week 3 onward Maintain current dose of lamotrigine 200 200aValproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Hikma Pharmaceutical
![Lamotrigine Tablet [Hikma Pharmaceutical]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Hikma Pharmaceutical
![Lamotrigine Tablet [Hikma Pharmaceutical] Lamotrigine Tablet [Hikma Pharmaceutical]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives:Starting lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives:(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (pill-free week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine consistently occur during the pill-free week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the pill-free week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy:Epilepsy: For patients receiving lamotrigine in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients aged 2 to 12 years. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients aged 2 to 12 years). A weight-based dosing guide for patients aged 2 to 12 years on concomitant valproate is provided in Table 3.
Patients Greater Than 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Greater Than 12 Years of Age With Epilepsy For Patients TAKING Valproatea For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,b or Valproatea For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day100 mg/day
(in 2 divided doses) Week 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks. Usual maintenance dose100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses)225 to 375 mg/day
(in 2 divided doses)300 to 500 mg/day
(in 2 divided doses)aValproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Patients Aged 2 to 12 Years: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients Aged 2 to 12 Years With Epilepsy For Patients TAKING Valproatea For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,b or Valproatea For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproate a Weeks 1 and 20.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide)0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet
0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet
Weeks 3 and 40.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide)0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet
1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet
Week 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual maintenance dose1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses)
1 to 3 mg/kg/day with valproate alone4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical responseNote: Only whole tablets should be used for dosing.
aValproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 3. The Initial Weight-Based Dosing Guide for Patients Aged 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of lamotrigine 2-mg and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age With Epilepsy Lamotrigine Valproate Step 1 Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day).Maintain previous stable dose.
Step 2 Maintain at 200 mg/day. Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week. Step 3 Increase to 300 mg/day and maintain for 1 week. Simultaneously decrease to 250 mg/day and maintain for 1 week. Step 4 Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day. Discontinue.Conversion From Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder For Patients TAKING Valproatea For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,b or Valproatea For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided dosesaValproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone,b or Valproatea) After Discontinuation of Valproatea After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or PrimidonebCurrent dose of LAMICTAL (mg/day)
100Current dose of LAMICTAL (mg/day)
400 Week 1 Maintain current dose of lamotrigine 150 400 Week 2 Maintain current dose of lamotrigine 200 300 Week 3 onward Maintain current dose of lamotrigine 200 200aValproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Ncs Healthcare Of Ky, Inc Dba Vangard Labs
![Lamotrigine Tablet [Ncs Healthcare Of Ky, Inc Dba Vangard Labs]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Ncs Healthcare Of Ky, Inc Dba Vangard Labs
![Lamotrigine Tablet [Ncs Healthcare Of Ky, Inc Dba Vangard Labs] Lamotrigine Tablet [Ncs Healthcare Of Ky, Inc Dba Vangard Labs]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablets is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine tablets will in most cases need to be increased, by as much as 2 fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (112.3)], the maintenance dose will in most cases need to be increased by as much as 2 fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other druds such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2 week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2 fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1 to 3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine tablets in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, or primidone should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ see Drug Interactions (7), Clinical Pharmacology (12.3)] . † These drugs induce lamotrigine glucuronidation and increase clearance [ see Drug Interactions (7) Clinical Pharmacology (12.3)]. Other drugs, which have similar effects include estrogen-containing oral contraceptives [ see Drug Interactions (7), Clinical Pharmacology (12.3)] . Other drugs which have similar effects include estrogen containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacologu (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [ see Dosage and Administration (2.1)] . Patients on rifampin, or other drugs that induce lamitrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsdants that have this effect. For Patients Taking Valproate* For Patients Taking AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, or Primidone†, and Not Taking Valproate For Patients Taking Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and Not Taking Valproate Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day (in 2 divided doses) Weeks 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks Usual Maintenance Dose100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronication
(in 1 or 2 divided doses)
225 to 375 mg/day (in 2 divided doses)300 to 500 mg/day
(in 2 divided doses)
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ see Drug Interactions (7), Pharmacokinetics (12.3)] . † These drugs induce glucuronidation and increase clearance [see Drug Interactions (7) Pharmacokinetics (12.3)]. Other drugs, which have similar effects include estrogen-containing oral contraceptives and rifampin [ see Drug Interactions (7), Pharmacokinetics (12.3)] . Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [ see Dosage and Administration (2.1)] . Patients on rifampin should follow the same dosing titration/maintenance regimen used with drugs that induce glucuronidation. For Patients Taking Valproate* For Patients Taking AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, or Primidone†, and Not Taking Valproate For Patients Taking Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and Not Taking Valproate Weeks 1 and 2 0.15 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet Weeks 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual Maintenance Dose 1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day (maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical responseNote: Only whole tablets should be used for dosing.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of lamotrigine tablets, 2 mg and 5 mg Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets: After achieving a dose of 500 mg/day of lamotrigine tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4 week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥ 16 Years of Age With Epilepsy Lamotrigine Valproate Step 1 Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day). Maintain previous stable dose. Step 2 Maintain at 200 mg/day. Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week. Step 3 Increase to 300 mg/day and maintain for 1 week. Simultaneously decrease to 250 mg/day and maintain for 1 week. Step 4 Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day. Discontinue.Conversion From Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, which increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2 week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2 week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder* * See Drug Interactions (7) and Clinical Pharmacology (12.3) for a description of known drug interactions. † Valproate has been shown to decrease the apparent clearance of lamotrigine. ‡ Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine. For Patients Taking Valproate† For Patients Not Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Rifampin‡ and Not Taking Valproate† For Patients Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Rifampin‡ and Not Taking Valproate† Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications* * See Drug Interactions (7) and Clinical Pharmacology (12.3) for a description of known drug interactions. † Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine. ‡ Valproate has been shown to decrease the apparent clearance of lamotrigine. Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone, Rifampin†, or Valproate‡) After Discontinuation of Valproate‡ After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Rifampin† Current dose of Lamotrigine (mg/day) 100Current dose of Lamotrigine (mg/day)
400
Week 1 Maintain current dose of lamotrigine 150 400 Week 2 Maintain current dose of lamotrigine 200 300 Week 3 onward Maintain current dose of lamotrigine 200 200The benefit of continuing treatment in patients who had been stabilized in an 8 to 16 week open-label phase with lamotrigine tablets was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ] Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Epilepsy
Adjunctive Use:
Lamotrigine is indicated as adjunctive therapy for partial seizures and the generalized seizures of Lennox-Gastaut syndrome in adult and pediatric patients (years of age).
Monotherapy Use:
Lamotrigine tablets and lamotrigine tablets (chewable, dispersible) are indicated for conversion to monotherapy in adults with partial seizures who are receiving treatment with carbamazepine, phenytoin, phenobarbital, primidone, or valproate as the single AED.
Safety and effectiveness of lamotrigine tablets and lamotrigine tablets (chewable, dispersible)have not been established. (1) as initial monotherapy, (2) for conversion to monotherapy from AEDs other than carbamazepine, phenytoin, phenobarbital, primidone, or valproate, or (3) for simultaneous conversion to monotherapy from 2 or more concomitant AEDs.
Bipolar Disorder
Lamotrigine tablets and lamotrigine tablets (chewable, dispersible) are indicated for the maintenance treatment of Bipolar I Disorder to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The effectiveness of lamotrigine in the acute treatment of mood episodes has not been established.
General Dosing Considerations for Epilepsy and Bipolar Disorder Patients:
The risk of nonserious rash is increased when the recommended initial dose and/or the rate of dose escalation of Lamotrigine is exceeded. There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have been reported in the absence of these factors (see BOX WARNING). Therefore, it is important that the dosing recommendations be followed closely.
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed.
Lamotrigine Tablets and Lamotrigine Tablets (Chewable, Dispersible)Added to Drugs Known to Induce or Inhibit Glucuronidation:
Drugs other than those listed in PRECAUTIONS: Drug Interactionshave not been systematically evaluated in
combination with Lamotrigine. Since lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine, and doses of Lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder:
A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response.
The half-life of lamotrigine is affected by other concomitant medications (see CLINICAL PHARMACOLOGY: Pharmacokinetics and Drug Metabolism).
See also DOSAGE AND ADMINISTRATION: Special Populations.
Special Populations: Women and Oral Contraceptives: Starting Lamotrigine Tablets and LamotrigineTablets (Chewable, Dispersible)in Women Taking Oral Contraceptives
Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine (see PRECAUTIONS: Drug Interactions), no adjustments to the recommended dose escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED (see Table 11). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets and Lamotrigine Tablets (Chewable, Dispersible)
1. Taking Estrogen-Containing Oral Contraceptives:
For women not taking carbamazepine, phenytoin, phenobarbital, primidone,
or rifampin, the maintenance dose of Lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level (see PRECAUTIONS: Drug Interactions). (2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of Lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose will in most cases need to be increased by as much as 2-fold, in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate unless lamotrigine plasma levels or clinical response support larger increases (see Table 11, column 2,). Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse events, such as dizziness, ataxia, and diplopia (see PRECAUTIONS: Drug Interactions). If adverse events attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment should be necessary to the dose of Lamotrigine. (3) Stopping Estrogen-Containing Oral Contraceptives:For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50%, in order to maintain a consistent lamotrigine plasma level. The decrease in dose of Lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise (see PRECAUTIONS: Drug Interactions). For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy:
The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment:
Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver dysfunction (see CLINICAL PHARMACOLOGY), the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without
ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Functional Impairment:
Initial doses of lamotrigine tablets and lamotrigine tablets (chewable, dispersible) should be based on patients' AED regimen (see above); reduced maintenance doses may be effective for patients with significant renal functional impairment (see CLINICAL PHARMACOLOGY). Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Epilepsy:
Adjunctive Therapy With Lamotrigine Tablets and Lamotrigine Tablets (Chewable, Dispersible) for Epilepsy:
This section provides specific dosing recommendations for patients 2 to 12 years of age and patients greater than 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED (Table 9 for patients 2 to 12 years of age and Table 11 for patients greater than 12 years of age). A weight based dosing guide for pediatric patients on concomitant valproate is provided in Table 10.
Patients 2 to 12 Years of Age:
Recommended dosing guidelines are summarized in Table 9.
Note that some of the starting doses and dose escalations listed in Table 9 are different than those used in clinical trials; however, the maintenance doses are the same as in clinical trials. Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestions that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 9. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy
*Rifampin and estrogen-containing oral contraceptives have also been shown to increase the apparent clearance of lamotrigine (see PRECAUTIONS: Drug Interactions).For Patients Taking Valproate (see Table 10 for weight- based dosing guide)For Patients Taking AEDs Other Than Carbamazepine, Phenytoi n, Phenobarbital, Primidone *, or ValproateFor Patients Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone *and Not Taking ValproateWeeks 1 and 20.15 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 10 for weight-based dosing guide).0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet.0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet.Weeks 3 and 40.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 10 for weight-based dosing guide).0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet.1.2 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet.Weeks 5 onwards to maintenanceThe dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose.The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily doseThe dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily doseUsual Maintenance Dose1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses). 1 to 3 mg/kg/day with valproate alone4.5 to 7.5 mg/kg/day (maximum 300 mg/day in 2 divided doses)5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses)Maintenance dose in patients less than 30 kgMay need to be increased by as much as 50%, based on clinical responseMay need to be increased by as much as 50%, based on clinical responseMay need to be increased by as much as 50%, based on clinical responseNote: Only whole tablets should be used for dosing
Table 10. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy
If the patient's weight isGive this daily dose, using the most appropriate combination of lamotrigine tablets (chewable, dispersible), 5 mgGreater thanAnd less thanWeeks 1 and 2Weeks 3 and 434.1 kg40 kg5 mg every day10 mg every dayPatients Over 12 Years of Age:
Recommended dosing guidelines are summarized in Table 11.
Table 11. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy
*Rifampin and estrogen-containing oral contraceptives have also been shown to increase the apparent clearance of lamotrigine (see PRECAUTIONS: Drug Interactions).For Patients Taking ValproateFor Patients Taking AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate *For Patients Taking Carbamazepine, Phenytoin, PhenobarbitaL, Primidone *and Not Taking ValproateWeeks 1 and 225 mg every other day25 mg every day50 mg/dayWeeks 3 and 425 mg every day50 mg/day100 mg/day (in 2 divided doses)Weeks 5 onwards to maintenanceIncrease by 25 to 50 mg/ day every 1 to 2 weeksIncrease by 50 mg/ day every 1 to 2 weeksIncrease by 100 mg/ day every 1 to 2 weeks.Usual Maintenance Dose100 to 400 mg/day (1 or 2 divided doses) 100 to 200 mg/day with Valproate alone225 to 375 mg/day (in 2 divided doses).300 to 500 mg/day (in 2 divided doses).Conversion from Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate as the Single AED to Monotherapy With Lamotrigine in PatientsYears of Age With Epilepsy:
The goal of the transition regimen is to effect the conversion to monotherapy with Lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded (see BOX WARNING).
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine:
After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 11, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine The conversion regimen involves 4 steps (see Table 12).
Table 12. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in PatientsYears of Age With Epilepsy
LamotrigineValproateStep 1Achieve a dose of 200 mg/day according to guidelines in Table 11 (if not already on 200 mg/ day).Maintain previous stable dose.Step 2Maintain at 200 mg/day.Decrease to 500 mg/day by decrements no greater than 500 mg/day per week and then maintain the dose of 500 mg/day for 1 week.Step 3Increase to 300 mg/day and maintain for 1 week.Simultaneously decrease to 250 mg/day and maintain for 1 week.Step 4Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.Discontinue. Conversion from Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine:
No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
Usual Maintenance Dose for Epilepsy
The usual maintenance doses identified in Tables 9-11 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive Lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive Lamotrigine as high as 200 mg/ day have been used. The advantage of using doses above those recommended in Tables 9-12 has not been established in controlled trials.
Discontinuation Strategy for Patients With Epilepsy:
For patients receiving lamotrigine in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse experiences is observed.
If a decision is made to discontinue therapy with Lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal (see PRECAUTIONS).
Discontinuing carbamazepine, phenytoin, phenobarbital, or primidone should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder
The goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate,which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, which increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated, however, no additional benefit was seen at 400 mg/day compared to 200 mg/day (see CLINICAL STUDIES: Bipolar Disorder). Accordingly, doses above 200 mg/ day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 13. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 14). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 14). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
Dosage adjustments will be necessary in most patients who start or stop estrogen-containing oral contraceptives while taking lamotrigine (see DOSAGE AND ADMINISTRATION: Special Populations: Women and Oral Contraceptives: Adjustments to the Maintenace Dose of Lamotrigine).
If other drugs are subsequently introduced, the dose of Lamotrigine may need to be adjusted.
In particular, the introduction of valproate requires reduction in the dose of Lamotrigine (see CLINICAL PHARMACOLOGY: Drug Interactions). To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded (see BOX WARNING).
Table 13. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder *
*See CLINICAL PHARMACOLOGY: Drug Interactions:and PRECAUTIONS: Drug Interactionsfor a description of known drug interactions. Carbamazepine, phenytoin, phenobarbital, primidone, rifampin, have been shown to increase the apparent clearance of lamotrigine. Valproate has been shown to decrease the apparent clearance of lamotrigine.For Patients Not Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone or Rifampin and Not Taking Valproate For Patients Taking Valproate For Patients Taking Carbamazepine (or Other Enzyme-Inducing Drugs) and Not Taking Valproate Weeks 1 and 225 mg daily25 mg every other day50 mg dailyWeeks 3 and 450 mg daily25 mg daily100 mg daily, in divided dosesWeek 5100 mg daily50 mg daily200 mg daily, in divided dosesWeek 6200 mg daily100 mg daily300 mg daily, in divided dosesWeek 7200 mg daily100 mg dailyup to 400 mg daily, in divided doses
Table 14. Adjustments to Lamotrigine Dosing for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications *
*See CLINICAL PHARMACOLOGY: Drug Interactions:and PRECAUTIONS: Drug Interactionsfor a description of known drug interactions. Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine. Valproate has been shown to decrease the apparent clearance of lamotrigine.Discontinuation of Psychotropic Drugs (excluding Valproate , Carbamazepine, or Other Enzyme-Inducing Drugs )After Discontinuation of Valproate After Discontinuation of Carbamazepine or Other Enzyme-Inducing Drugs Current Lamotrigine dose (mg/day) 100Current Lamotrigine dose (mg/day) 400Week 1Maintain current lamotrigine dose150400Week 2Maintain current lamotrigine dose200300Week 3 onwardMaintain current lamotrigine dose200200There is no body of evidence available to answer the question of how long the patient should remain on lamotrigine therapy. Systematic evaluation of the efficacy of lamotrigine in patients with either depression or mania who responded to standard therapy during an acute 8 to 16 week treatment phase and were then randomized to lamotrigine or placebo for up to 76 weeks of observation for affective relapse demonstrated a benefit of such maintenance treatment (see CLINICAL STUDIES: Bipolar Disorder). Nevertheless, patients should be periodically reassessed to determine the need for maintenance treatment.
Discontinuation Strategy in Bipolar Disorder:
As with other AEDs, lamotrigine should not be abruptly discontinued. In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse experiences following abrupt termination of lamotrigine. In clinical trials in patients with bipolar disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal.
Administration of Lamotrigine Tablets (Chewable, Dispersible)
Lamotrigine tablets (Chewable, Dispersible) may be swallowed whole, chewed, or dispersed in water or diluted fruit juice. If the tablets are chewed, consume a small amount of water or diluted fruit juice to aid in swallowing.
To disperse lamotrigine tablets (chewable, dispersible), add the tablets to a small amount of liquid (1 teaspoon, or enough to cover the medication). Approximately 1 minute later, when the tablets are completely dispersed, swirl the solution and consume the entire quantity immediately.
No attempt should be made to administer partial quantities of the dispersed tablets.
-
Rebel Distributors Corp
![Lamotrigine Tablet [Rebel Distributors Corp]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Rebel Distributors Corp
![Lamotrigine Tablet [Rebel Distributors Corp] Lamotrigine Tablet [Rebel Distributors Corp]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of LAMOTRIGINE with valproate, (2) exceeding the recommended initial dose of LAMOTRIGINE, or (3) exceeding the recommended dose escalation for LAMOTRIGINE. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of LAMOTRIGINE is exceeded and in patients with a history of allergy or rash to other AEDs.
LAMOTRIGINE Starter Kits provide LAMOTRIGINE at doses consistent with the recommended titration schedule for the first 5 weeks of treatment, based upon concomitant medications for patients with epilepsy (>12 years of age) and Bipolar I Disorder (≥18 years of age) and are intended to help reduce the potential for rash. The use of LAMOTRIGINE Starter Kits is recommended for appropriate patients who are starting or restarting LAMOTRIGINE [see How Supplied/Storage and Handling (16)].
It is recommended that LAMOTRIGINE not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
LAMOTRIGINE Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of LAMOTRIGINE may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of LAMOTRIGINE should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting LAMOTRIGINE in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for LAMOTRIGINE should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with LAMOTRIGINE based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of LAMOTRIGINE in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of LAMOTRIGINE In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of LAMOTRIGINE will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of LAMOTRIGINE and not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to LAMOTRIGINE consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking LAMOTRIGINE in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment should be necessary to the dose of LAMOTRIGINE.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of LAMOTRIGINE will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of LAMOTRIGINE should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking LAMOTRIGINE in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment to the dose of LAMOTRIGINE should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of LAMOTRIGINE in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of LAMOTRIGINE should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with LAMOTRIGINE. Because there is inadequate experience in this population, LAMOTRIGINE should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving LAMOTRIGINE in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with LAMOTRIGINE, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, or primidone should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of LAMOTRIGINE. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of LAMOTRIGINE. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of LAMOTRIGINE should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for LAMOTRIGINE in Patients Over 12 Years of Age With Epilepsy For Patients Taking Valproate * For Patients Taking AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, or Primidone†, and Not Taking Valproate For Patients Taking Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and Not Taking Valproate * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Pharmacokinetics (12.3)]. † These drugs induce glucuronidation and increase clearance [see Drug Interactions (7), Pharmacokinetics (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives and rifampin [see Drug Interactions (7), Pharmacokinetics (12.3)]. Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day
(in 2 divided doses) Weeks 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks. Usual Maintenance Dose 100 to 200 mg/day with valproate alone 100 to 400 mg/day with valproate and other drugs that induce glucuronication
(in 1 or 2 divided doses) 225 to 375 mg/day
(in 2 divided doses) 300 to 500 mg/day
(in 2 divided doses)Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin should follow the same dosing titration/maintenance regimen used with drugs that induce glucuronidation and increase clearance.
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for LAMOTRIGINE in Patients 2 to 12 Years of Age With Epilepsy For Patients Taking Valproate * For Patients Taking AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, or Primidone†, and Not Taking Valproate For Patients Taking Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and Not Taking Valproate Note: Only whole tablets should be used for dosing. * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Pharmacokinetics (12.3)]. † These drugs induce glucuronidation and increase clearance [see Drug Interactions (7), Pharmacokinetics (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives and rifampin [see Drug Interactions (7), Pharmacokinetics (12.3)]. Weeks 1 and 2 0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual Maintenance Dose 1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses). 1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day
(maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical responseDosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin should follow the same dosing titration/maintenance regimen used with drugs that induce glucuronidation and increase clearance.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient's weight is Give this daily dose, using the most appropriate combination of LAMOTRIGINE 2-mg and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of LAMOTRIGINE was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive LAMOTRIGINE as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive LAMOTRIGINE as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with LAMOTRIGINE under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of LAMOTRIGINE.
The recommended maintenance dose of LAMOTRIGINE as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of LAMOTRIGINE should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With LAMOTRIGINE: After achieving a dose of 500 mg/day of LAMOTRIGINE according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With LAMOTRIGINE: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With LAMOTRIGINE in Patients ≥16 Years of Age with Epilepsy LAMOTRIGINE Valproate Step 1 Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on200 mg/day). Maintain previous stable dose. Step 2 Maintain at 200 mg/day. Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week. Step 3 Increase to 300 mg/day and maintain for 1 week. Simultaneously decrease to 250 mg/day and maintain for 1 week. Step 4 Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day. Discontinue.Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With LAMOTRIGINE: No specific dosing guidelines can be provided for conversion to monotherapy with LAMOTRIGINE with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with LAMOTRIGINE is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of LAMOTRIGINE is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, which increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with LAMOTRIGINE is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of LAMOTRIGINE should be adjusted. For patients discontinuing valproate, the dose of LAMOTRIGINE should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the dose of LAMOTRIGINE should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of LAMOTRIGINE may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of LAMOTRIGINE may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of LAMOTRIGINE [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of LAMOTRIGINE should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for LAMOTRIGINE for Patients With Bipolar Disorder* For Patients Taking Valproate† For Patients Not Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Rifampin‡ and Not Taking Valproate† For Patients Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Rifampin‡ and Not Taking Valproate† * See Drug Interactions (7) and Clinical Pharmacology (12.3) for a description of known drug interactions. † Valproate has been shown to decrease the apparent clearance of lamotrigine. ‡ Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine. Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to LAMOTRIGINE for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications* Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone, Rifampin†, or Valproate‡) After Discontinuation of Valproate‡ After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Rifampin† Current dose of LAMOTRIGINE (mg/day) 100 Current dose of LAMOTRIGINE (mg/day) 400 * See Drug Interactions (7) and Clinical Pharmacology (12.3) for a description of known drug interactions. † Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine. ‡ Valproate has been shown to decrease the apparent clearance of lamotrigine. Week 1 Maintain current dose of LAMOTRIGINE 150 400 Week 2 Maintain current dose of LAMOTRIGINE 200 300 Week 3 onward Maintain current dose of LAMOTRIGINE 200 200The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with LAMOTRIGINE was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with LAMOTRIGINE has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Lake Erie Medical & Surgical Supply Dba Quality Care Products Llc
![Lamotrigine Tablet [Lake Erie Medical & Surgical Supply Dba Quality Care Products Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Lake Erie Medical & Surgical Supply Dba Quality Care Products Llc
![Lamotrigine Tablet [Lake Erie Medical & Surgical Supply Dba Quality Care Products Llc] Lamotrigine Tablet [Lake Erie Medical & Surgical Supply Dba Quality Care Products Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
Lamotrigine Starter Kits provide lamotrigine at doses consistent with the recommended titration schedule for the first 5 weeks of treatment, based upon concomitant medications for patients with epilepsy (>12 years of age) and Bipolar I Disorder (≥18 years of age) and are intended to help reduce the potential for rash. The use of Lamotrigine Starter Kits is recommended for appropriate patients who are starting or restarting lamotrigine [see How Supplied/Storage and Handling (16)].
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.10)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.10)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy For Patients TAKING Valproate * For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day
(in 2 divided doses) Week 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks Usual Maintenance Dose 100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses) 225 to 375 mg/day
(in 2 divided doses) 300 to 500 mg/day
(in 2 divided doses)Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy For Patients TAKING Valproate * For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Note: Only whole tablets should be used for dosing. * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Weeks 1 and 2 0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Week 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual Maintenance Dose 1 to 5 mg/kg/day
(maximum 200 mg/day in 1 or 2 divided doses)
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day
(maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical responseDosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient's weight is Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age With Epilepsy Lamotrigine Valproate Step 1 Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day). Maintain previous stable dose. Step 2 Maintain at 200 mg/day. Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week. Step 3 Increase to 300 mg/day and maintain for 1 week. Simultaneously decrease to 250 mg/day and maintain for 1 week. Step 4 Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day. Discontinue.Conversion From Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone†, and NOT TAKING Valproate* * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone*, or Valproate†) After Discontinuation of Valproate† After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital or Primidone* Current dose of Lamotrigine (mg/day) 100 Current dose of Lamotrigine (mg/day) 400 * These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. † Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Week 1 Maintain current dose of Lamotrigine 150 400 Week 2 Maintain current dose of Lamotrigine 200 300 Week 3 onward Maintain current dose of Lamotrigine 200 200The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Mylan Pharmaceuticals Inc.
![Lamotrigine Tablet, Chewable [Mylan Pharmaceuticals Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Mylan Pharmaceuticals Inc.
![Lamotrigine Tablet, Chewable [Mylan Pharmaceuticals Inc.] Lamotrigine Tablet, Chewable [Mylan Pharmaceuticals Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
The dose of zaleplon capsules should be individualized. The recommended dose of zaleplon capsules for most non-elderly adults is 10 mg. For certain low weight individuals, 5 mg may be a sufficient dose. Although the risk of certain adverse events associated with the use of zaleplon capsules appears to be dose dependent, the 20 mg dose has been shown to be adequately tolerated and may be considered for the occasional patient who does not benefit from a trial of a lower dose. Doses above 20 mg have not been adequately evaluated and are not recommended.
Zaleplon capsules should be taken immediately before bedtime or after the patient has gone to bed and has experienced difficulty falling asleep (see PRECAUTIONS). Taking zaleplon capsules with or immediately after a heavy, high fat meal results in slower absorption and would be expected to reduce the effect of zaleplon on sleep latency (see CLINICAL PHARMACOLOGY: Pharmacokinetics).
Special PopulationsElderly patients and debilitated patients appear to be more sensitive to the effects of hypnotics, and respond to 5 mg of zaleplon. The recommended dose for these patients is therefore 5 mg. Doses over 10 mg are not recommended.
Hepatic InsufficiencyPatients with mild to moderate hepatic impairment should be treated with zaleplon capsules 5 mg because clearance is reduced in this population. Zaleplon capsules are not recommended for use in patients with severe hepatic impairment.
Renal InsufficiencyNo dose adjustment is necessary in patients with mild to moderate renal impairment. Zaleplon capsules have not been adequately studied in patients with severe renal impairment.
An initial dose of 5 mg should be given to patients concomitantly taking cimetidine because zaleplon clearance is reduced in this population (see PRECAUTIONS: Drug Interactions).
-
Cadila Healthcare Limited
![Lamotrigine Tablet Lamotrigine Tablet, Chewable [Cadila Healthcare Limited]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Cadila Healthcare Limited
![Lamotrigine Tablet Lamotrigine Tablet, Chewable [Cadila Healthcare Limited] Lamotrigine Tablet Lamotrigine Tablet, Chewable [Cadila Healthcare Limited]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash
There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see BOXED WARNING]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see CLINICAL PHARMACOLOGY (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation
Drugs other than those listed in the Clinical Pharmacology section [see CLINICAL PHARMACOLOGY (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients with Epilepsy or Bipolar Disorder
A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response [see CLINICAL PHARMACOLOGY (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives
Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives
Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see CLINICAL PHARMACOLOGY (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives
(1) Taking Estrogen-Containing Oral Contraceptives
For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see DRUG INTERACTIONS (7), CLINICAL PHARMACOLOGY (12.3)], the maintenance dose of lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see CLINICAL PHARMACOLOGY (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives
In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see DRUG INTERACTIONS (7), CLINICAL PHARMACOLOGY (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see DRUG INTERACTIONS (7), CLINICAL PHARMACOLOGY (12.3)], no adjustment to the dose of lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives
For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see DRUG INTERACTIONS (7), CLINICAL PHARMACOLOGY (12.3)], the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see CLINICAL PHARMACOLOGY (12.3)]. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see DRUG INTERACTIONS (7), CLINICAL PHARMACOLOGY (12.3)], no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy
The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients with Hepatic Impairment
Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see USE IN SPECIFIC POPULATIONS (8.6), CLINICAL PHARMACOLOGY (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients with Renal Impairment
Initial doses of lamotrigine should be based on patients’ concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see USE IN SPECIFIC POPULATIONS (8.6), CLINICAL PHARMACOLOGY (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy
Epilepsy
For patients receiving lamotrigine in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see WARNINGS AND PRECAUTIONS (5.10)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder
In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see WARNINGS AND PRECAUTIONS (5.10)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age
Recommended dosing guidelines are summarized in Table 1.
Table 1 Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy
For Patients Taking Valproate*
For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate*
For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate*
* Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see DRUG INTERACTIONS ( 7), CLINICAL PHARMACOLOGY ( 12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [see DRUG INTERACTIONS ( 7), CLINICAL PHARMACOLOGY ( 12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see DRUG INTERACTIONS ( 7), CLINICAL PHARMACOLOGY ( 12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see DOSAGE AND ADMINISTRATION ( 2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Week 5 onwards to maintenance
Increase by 25 to 50 mg/day every 1 to 2 weeks
Increase by 50 mg/day every 1 to 2 weeks
Increase by 100 mg/day every 1 to 2 weeks.
Usual Maintenance Dose
100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses)
225 to 375 mg/day
(in 2 divided doses)
300 to 500 mg/day
(in 2 divided doses)
Patients 2 to 12 Years of Age
Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2 Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy
For Patients TAKING Valproatea
For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb, or Valproatea
For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea
Note: Only whole tablets should be used for dosing.
*Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see DRUG INTERACTIONS (7), Pharmacokinetics (12.3)].
bThese drugs induce lamotrigine glucuronidation and increase clearance [see DRUG INTERACTIONS (7), CLINICAL PHARMACOLOGY (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see DRUG INTERACTIONS (7), CLINICAL PHARMACOLOGY (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see DOSAGE AND ADMINISTRATION (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Weeks 1 and 2
0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest
whole tablet (see Table 3 for weight based dosing guide)
0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet
0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet
Weeks 3 and 4
0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest
whole tablet (see Table 3 for weight based dosing guide)
0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet
1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet
Weeks 5 onwards to maintenance
The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
Usual Maintenance Dose
1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses)
1 to 3 mg/kg/day with valproate alone
4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses)
5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses)
Maintenance dose in patients less than 30 kg
May need to be increased by as much as 50%,
based on clinical response
May need to be increased by as much as 50%,
based on clinical response
May need to be increased by as much as 50%,
based on clinical response
Table 3 The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is
Give this daily dose, using the most appropriate combination of Lamotrigine 5 mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy
The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion from Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see BOXED WARNING].
Conversion from Adjunctive Therapy with Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy with Lamotrigine
After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy with Valproate to Monotherapy with Lamotrigine
The conversion regimen involves 4 steps outlined in Table 4.
Table 4 Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age With Epilepsy
Lamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to
guidelines in Table 1 (if not already on 200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and
then maintain the dose of 500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy with AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy with Lamotrigine
No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see DRUG INTERACTIONS (7), CLINICAL PHARMACOLOGY (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see BOXED WARNING].
Table 5 Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see DRUG INTERACTIONS ( 7), CLINICAL PHARMACOLOGY ( 12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [see DRUG INTERACTIONS (7), CLINICAL PHARMACOLOGY ( 12.3)]. Other drugs which have similar effects include estrogen containing oral contraceptives [see DRUG INTERACTIONS ( 7), CLINICAL PHARMACOLOGY ( 12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see DOSAGE AND ADMINISTRATION ( 2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
For Patients TAKING Valproate*
For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate*
For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate*
Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
Table 6 Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications * These drugs induce lamotrigine glucuronidation and increase clearance [see DRUG INTERACTIONS ( 7), CLINICAL PHARMACOLOGY ( 12.3)]. Other drugs which have similar effects include estrogen containing oral contraceptives [see DRUG INTERACTIONS ( 7), CLINICAL PHARMACOLOGY ( 12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see DOSAGE AND ADMINISTRATION ( 2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. † Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see DRUG INTERACTIONS ( 7), CLINICAL PHARMACOLOGY ( 12.3)].
Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone*, or Valproate†)
After Discontinuation of Valproate†
After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone*
Current dose of Lamotrigine (mg/day)
100
Current dose of Lamotrigine (mg/day)
400
Week 1
Maintain current dose of Lamotrigine
150
400
Week 2
Maintain current dose of Lamotrigine
200
300
Week 3 onward
Maintain current dose of Lamotrigine
200
200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
2.5 Administration of Lamotrigine Tablets (Chewable, Dispersible)Lamotrigine Tablets (Chewable, Dispersible) may be swallowed whole, chewed, or dispersed in water or diluted fruit juice. If the tablets are chewed, consume a small amount of water or diluted fruit juice to aid in swallowing.
To disperse Lamotrigine Tablets (Chewable, Dispersible), add the tablets to a small amount of liquid (1 teaspoon, or enough to cover the medication). Approximately 1 minute later, when the tablets are completely dispersed, swirl the solution and consume the entire quantity immediately. No attempt should be made to administer partial quantities of the dispersed tablets.
-
Unichem Pharmaceuticals (Usa), Inc.
![Lamotrigine Tablet [Unichem Pharmaceuticals (Usa), Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Unichem Pharmaceuticals (usa), Inc.
![Lamotrigine Tablet [Unichem Pharmaceuticals (Usa), Inc.] Lamotrigine Tablet [Unichem Pharmaceuticals (Usa), Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning ]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablet is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3) ].
Lamotrigine Tablets Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3) ] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3) ].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3) ], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3) ].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3) ]. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6) , Clinical Pharmacology (12.3) ], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7) , Clinical Pharmacology (12.3) ]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.
Discontinuation Strategy:
Epilepsy: For patients receiving lamotrigine tablets in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9) ].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9) ].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine Tablets in Patients Over 12 Years of Age With Epilepsya Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
For
For Patients NOT TAKING
For Patients
Patients
Carbamazepine,
TAKING
TAKING
Phenytoin,
Carbamazepine,
Valproatea
Phenobarbital,
Phenytoin,
or Primidoneb,
Phenobarbital,
or Valproatea
or Primidoneb
and NOT TAKING
Valproatea
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Weeks 5 onwards to
maintenance
Increase by 25 to
50 mg/day every 1 to 2 weeks
Increase by 50
mg/day every 1
to 2 weeks
Increase by
100 mg/day every
1 to 2 weeks.
Usual maintenance
dose
100 to 200 mg/day
with valproate alone
225 to 375 mg/day
(in 2 divided doses).
300 to 500 mg/day
(in 2 divided doses).
100 to 400 mg/day
with valproate
and other drugs that induce glucuronidation
(in 1 or 2 divided doses)
Patients 2 to 12 Years Of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine Tablets in Patients 2 to 12 Years of Age With EpilepsyNote: Only whole tablets should be used for dosing.
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
For Patients TAKING
Valproatea
For Patients NOT
TAKING Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea
For Patients TAKING
Carbamazepine, Phenytoin, Phenobarbital, or
Primidoneb and NOT
TAKING Valproatea
Weeks 1 and 2
0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the
nearest whole tablet (see Table 3 for weight
based dosing guide).
0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the
nearest whole tablet.
0.6 mg/kg/day
in 2 divided doses, rounded down to the
nearest whole tablet.
Weeks 3 and 4
0.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
(see Table 3 for weight
based dosing guide).
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet.
1.2 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet.
Weeks 5
onwards to
maintenance
The dose should be increased every
1 to 2 weeks as follows:
calculate 0.3 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose.
The dose should be increased every
1 to 2 weeks as follows:
calculate 0.6 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose
The dose should be increased every
1 to 2 weeks as follows:
calculate 1.2 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose
Usual
Maintenance
Dose
1 to 5 mg/kg/day
(maximum 200 mg/day
in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone
4.5 to 7.5 mg/kg/day
(maximum 300 mg/day
in 2 divided doses)
5 to 15 mg/kg/day
(maximum 400 mg/day
in 2 divided doses)
Maintenance dose in
patients
less than 30 kg
May need to be increased
by as much as 50%,
based on clinical response
May need to be increased
by as much as 50%,
based on clinical response
May need to be increased
by as much as 50%, based
on clinical response
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is
Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in two divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets: After achieving a dose of 500 mg/day of lamotrigine tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets:
The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets in Patients ≥16 Years of Age with Epilepsy
Lamotrigine Tablets
Valproate
Step 1
Achieve a dose of 200 mg/day according to
guidelines in Table 1
(if not already on 200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than
500 mg/day/week and then maintain the dose of
500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to
250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every
week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2) ]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7) , Clinical Pharmacology (12.3) ].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning ].
Table 5. Escalation Regimen for Lamotrigine Tablets for Patients With Bipolar Disordera Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
For Patients TAKING
Valproatea
For Patients NOT TAKING
Carbamazepine, Phenytoin, Phenobarbital,
Primidoneb, or Valproatea
For Patients TAKING
Carbamazepine, Phenytoin,
Phenobarbital, or Primidoneb and NOT TAKING
Valproatea
Weeks 1 and 2
25 mg every
other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
Table 6. Dosage Adjustments to Lamotrigine Tablets for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications
Discontinuation of Psychotropic Drugs
(excluding Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea)
After Discontinuation of
Valproatea
After Discontinuation of
Carbamazepine, Phenytoin,
Phenobarbital, or Primidoneb
Current dose of lamotrigine tablets
(mg/day)
100
Current dose of lamotrigine tablets
(mg/day)
400
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Week 1
Maintain current dose of lamotrigine tablets
150
400
Week 2
Maintain current dose of lamotrigine tablets
200
300
Week 3 onward
Maintain current dose of lamotrigine tablets
200
200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine tablets was established in two randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2) ]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Cardinal Health
![Lamotrigine Tablet [Cardinal Health]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Cardinal Health
![Lamotrigine Tablet [Cardinal Health] Lamotrigine Tablet [Cardinal Health]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablets is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine tablets will in most cases need to be increased, by as much as 2 fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose will in most cases need to be increased by as much as 2 fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment should be necessary to the dose of lamotrigine tablets.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2 week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2 fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1 to 3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine tablets in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, or primidone should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ see Drug Interactions (7), Pharmacokinetics (12.3)] . † These drugs induce glucuronidation and increase clearance [ see Drug Interactions (7) Pharmacokinetics (12.3)]. Other drugs, which have similar effects include estrogen-containing oral contraceptives and rifampin [ see Drug Interactions (7), Pharmacokinetics (12.3)] . Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [ see Dosage and Administration (2.1)] . Patients on rifampin should follow the same dosing titration/maintenance regimen used with drugs that induce glucuronidation and increase clearance. For Patients Taking Valproate* For Patients Taking AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, or Primidone†, and Not Taking Valproate For Patients Taking Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and Not Taking Valproate Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day (in 2 divided doses) Weeks 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks Usual Maintenance Dose100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronication
(in 1 or 2 divided doses)
225 to 375 mg/day (in 2 divided doses)300 to 500 mg/day
(in 2 divided doses)
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ see Drug Interactions (7), Pharmacokinetics (12.3)] . † These drugs induce glucuronidation and increase clearance [see Drug Interactions (7) Pharmacokinetics (12.3)]. Other drugs, which have similar effects include estrogen-containing oral contraceptives and rifampin [ see Drug Interactions (7), Pharmacokinetics (12.3)] . Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [ see Dosage and Administration (2.1)] . Patients on rifampin should follow the same dosing titration/maintenance regimen used with drugs that induce glucuronidation. For Patients Taking Valproate* For Patients Taking AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, or Primidone†, and Not Taking Valproate For Patients Taking Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and Not Taking Valproate Weeks 1 and 2 0.15 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet Weeks 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual Maintenance Dose 1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day (maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical responseNOTE: Only whole tablets should be used for dosing.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of lamotrigine 2 mg and 5 mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets: After achieving a dose of 500 mg/day of lamotrigine tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4 week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥ 16 Years of Age With Epilepsy Lamotrigine Valproate Step 1 Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day). Maintain previous stable dose. Step 2 Maintain at 200 mg/day. Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week. Step 3 Increase to 300 mg/day and maintain for 1 week. Simultaneously decrease to 250 mg/day and maintain for 1 week. Step 4 Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day. Discontinue.Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, which increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2 week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2 week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder* * See Drug Interactions (7) and Clinical Pharmacology (12.3) for a description of known drug interactions. † Valproate has been shown to decrease the apparent clearance of lamotrigine. ‡ Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine. For Patients Taking Valproate† For Patients Not Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Rifampin‡ and Not Taking Valproate† For Patients Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Rifampin‡ and Not Taking Valproate† Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications* * See Drug Interactions (7) and Clinical Pharmacology (12.3) for a description of known drug interactions. † Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine. ‡ Valproate has been shown to decrease the apparent clearance of lamotrigine. Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone, Rifampin†, or Valproate‡) After Discontinuation of Valproate‡ After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Rifampin† Current dose of Lamotrigine (mg/day) 100Current dose of Lamotrigine (mg/day)
400
Week 1 Maintain current dose of lamotrigine 150 400 Week 2 Maintain current dose of lamotrigine 200 300 Week 3 onward Maintain current dose of lamotrigine 200 200The benefit of continuing treatment in patients who had been stabilized in an 8 to 16 week open-label phase with lamotrigine tablets was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Unit Dose Services
![Lamotrigine Tablet [Unit Dose Services]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Unit Dose Services
![Lamotrigine Tablet [Unit Dose Services] Lamotrigine Tablet [Unit Dose Services]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing Considerations: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of Lamotrigine with valproate, (2) exceeding the recommended initial dose of Lamotrigine, or (3) exceeding the recommended dose escalation for Lamotrigine. However, cases have occurred in the absence of these factors . Therefore, it is important that the dosing recommendations be followed closely. Rash[seeBoxed Warning]
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of Lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that Lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with Lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued Lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued Lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of Lamotrigine is affected by other concomitant medications . [see Clinical Pharmacology (12.3)]
: Drugs other than those listed in the Clinical Pharmacology section have not been systematically evaluated in combination with Lamotrigine. Because Lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of Lamotrigine and doses of Lamotrigine may require adjustment based on clinical response. Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation[see Clinical Pharmacology (12.3)]
A therapeutic plasma concentration range has not been established for Lamotrigine. Dosing of Lamotrigine should be based on therapeutic response . Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder:[see Clinical Pharmacology (12.3)]
: Although estrogen-containing oral contraceptives have been shown to increase the clearance of Lamotrigine , no adjustments to the recommended dose-escalation guidelines for Lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with Lamotrigine based on the concomitant AED or other concomitant medications (see or ). See below for adjustments to maintenance doses of Lamotrigine in women taking estrogen-containing oral contraceptives. Women Taking Estrogen-Containing Oral ContraceptivesStarting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives:[see Clinical Pharmacology (12.3)]Table 1Table 5
Adjustments to the Maintenance Dose of Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives:
For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation , the maintenance dose of Lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent Lamotrigine plasma level . (1) Taking Estrogen-Containing Oral Contraceptives:[see Drug Interactions ( ), 7Clinical Pharmacology ( )] 12.3[see Clinical Pharmacology (12.3)]
In women taking a stable dose of Lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent Lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see or ) unless Lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in Lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased Lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to Lamotrigine consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation , no adjustment to the dose of Lamotrigine should be necessary. (2) Starting Estrogen-Containing Oral Contraceptives:[see Drug Interactions ( ), Clinical Pharmacology ( )], 712.3Table 1Table 5[see Drug Interactions ( ), Clinical Pharmacology ( )] 712.3
For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation , the maintenance dose of Lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent Lamotrigine plasma level. The decrease in dose of Lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or Lamotrigine plasma levels indicate otherwise . For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation , no adjustment to the dose of Lamotrigine should be necessary. (3) Stopping Estrogen-Containing Oral Contraceptives:[see Drug Interactions ( ), Clinical Pharmacology ( )] 712.3[see Clinical Pharmacology ( )] 12.3[see Drug Interactions ( ), Clinical Pharmacology ( )] 712.3
: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of Lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of Lamotrigine up to 2-fold, and the progestin-only pills had no effect on Lamotrigine plasma levels. Therefore, adjustments to the dosage of Lamotrigine in the presence of progestogens alone will likely not be needed. Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy
: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment , the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response. Patients With Hepatic Impairment[see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)]
: Initial doses of Lamotrigine should be based on patients' concomitant medications (see or ); reduced maintenance doses may be effective for patients with significant renal impairment . Few patients with severe renal impairment have been evaluated during chronic treatment with Lamotrigine. Because there is inadequate experience in this population, Lamotrigine should be used with caution in these patients. Patients With Renal ImpairmentTables 1-3Table 5[see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]
: For patients receiving Lamotrigine in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse experiences is observed. Discontinuation StrategyEpilepsy:
If a decision is made to discontinue therapy with Lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation should prolong the half-life of Lamotrigine; discontinuing valproate should shorten the half-life of Lamotrigine.
In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of Lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of Lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of Lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal . Bipolar Disorder:[see Warnings and Precautions (5.9)]
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications ( for patients greater than 12 years of age and for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in . Table 1Table 2Table 3
Recommended dosing guidelines are summarized in . Patients Over 12 Years of Age:Table 1
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine [see Drug Interactions ( 7 ), Clinical Pharmacology ( 12.3 )]. † These drugs induce Lamotrigine glucuronidation and increase clearance Other drugs, which have similar effects include estrogen-containing oral contraceptives Dosing recommendations for oral contraceptives can be found in General Dosing Considerations Patients on rifampin, or other drugs that induce Lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. [see Drug Interactions ( 7 ) Clinical Pharmacology ( 12.3 )]. [see Drug Interactions ( 7 ), Clinical Pharmacology ( 12.3 )]. [see Dosage and Administration ( 2.1 )]. For Patients TAKING Valproate * For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone ,or Valproate †* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone and NOT TAKING Valproate †* Weeks 1 and 2 25 mg every day other 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day (in 2 divided doses) 100 mg/day Weeks 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day every 1 to 2 weeks
Increase by 100 mg/day every 1 to 2 weeks Usual Maintenance Dose (in 1 or 2 divided doses) 100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronication
(in 2 divided doses) 225 to 375 mg/day
(in 2 divided doses) 300 to 500 mg/dayRecommended dosing guidelines are summarized in . Patients 2 to 12 Years of Age:Table 2
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine [see Drug Interactions ( ), Clinical Pharmacology ( )]. 712.3 † These drugs induce Lamotrigine glucuronidation and increase clearance . Other drugs, which have similar effects include estrogen-containing oral contraceptives . Dosing recommendations for oral contraceptives can be found in Patients on rifampin, or other drugs that induce Lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. [see Drug Interactions ( ) Clinical Pharmacology ( )] 712.3 [see Drug Interactions ( ) Clinical Pharmacology ( )] 712.3
General Dosing Considerations [see Dosage and Administration ( )]. 2.1 For Patients TAKING Valproate * For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone or Valproate
†
* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone and NOT TAKING Valproate †* Weeks 1 and 2 in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.3 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day
Weeks 3 and 4 in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.3 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day
Weeks 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual Maintenance Dose (maximum 200 mg/day in 1 or 2 divided doses). with valproate alone 1 to 5 mg/kg/day1 to 3 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 4.5 to 7.5 mg/kg/day
(maximum 400 mg/day in 2 divided doses) 5 to 15 mg/kg/day
Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response Note: Only whole tablets should be used for dosing. Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every day other 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayThe usual maintenance doses identified in Tables and are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of Lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone , maintenance doses of adjunctive Lamotrigine as high as 700 mg/day have been used. In patients receiving , maintenance doses of adjunctive Lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables has not been established in controlled trials. Usual Adjunctive Maintenance Dose for Epilepsy:12without valproatevalproate alone1 through 4
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with Lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of Lamotrigine.
The recommended maintenance dose of Lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded . [see ] Boxed Warning
After achieving a dose of 500 mg/day of Lamotrigine according to the guidelines in , the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial. Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine:Table 1
The conversion regimen involves 4 steps outlined in . Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine:Table 4
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age with EpilepsyLamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in (if not already on 200 mg/day). Table 1
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
No specific dosing guidelines can be provided for conversion to monotherapy with Lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate. Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine:
2.4 Bipolar Disorder
The goal of maintenance treatment with Lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of Lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of Lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin, that increase the apparent clearance of Lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day . Accordingly, doses above 200 mg/day are not recommended. Treatment with Lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in . If other psychotropic medications are withdrawn following stabilization, the dose of Lamotrigine should be adjusted. For patients discontinuing valproate, the dose of Lamotrigine should be doubled over a 2-week period in equal weekly increments (see ). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation, the dose of Lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see ). The dose of Lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated. [see Clinical Studies ( )] 14.2Table 5Table 6Table 6
If other drugs are subsequently introduced, the dose of Lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of Lamotrigine [see Drug Interactions ( ), Clinical Pharmacology ( )] 712.3.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded . [see ] Boxed Warning
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine [see Drug Interactions ( ), Clinical Pharmacology ( )]. 712.3 † These drugs induce Lamotrigine glucuronidation and increase clearance Other drugs which have similar effects include estrogen- containing oral contraceptives . Dosing recommendations for oral contraceptives can be found in General Dosing Considerations . Patients on rifampin, or other drugs that induce Lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/ maintenance regimen as that used with anticonvulsants that have this effect. [see Drug Interactions ( ), Clinical Pharmacology ( )]. 712.3 [see Drug Interactions ( ), Clinical Pharmacology ( )] 712.3
[see Dosage and Administration ( )] 2.1 For Patients TAKING Valproate * For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone , or Valproate †* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone and NOT TAKING Valproate †* Weeks 1 and 2 25 mg every day other 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications * These drugs induce Lamotrigine glucuronidation and increase clearance Other drugs which have similar effects include estrogen-containing oral contraceptives . Dosing recommendations for oral contraceptives can be found in General Dosing Considerations . Patients on rifampin, or other drugs that induce Lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/ maintenance regimen as that used with anticonvulsants that have this effect. [see Drug Interactions ( ), Clinical Pharmacology ( )]. 712.3 [see Drug Interactions ( ), Clinical Pharmacology ( )] 712.3 [see Dosage and Administration ( )] 2.1 † Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine [see Drug Interactions ( ), Clinical Pharmacology ( )]. 712.3Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone , or Valproate ) *†
After Discontinuation of Valproate † After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone * Current dose of Lamotrigine (mg/day) 100Current dose of Lamotrigine (mg/day) 400
Week 1 Maintain current dose of Lamotrigine 150 400 Week 2 Maintain current dose of Lamotrigine 200 300 Week 3 onward Maintain current dose of Lamotrigine 200 200The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with Lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials . However, the optimal duration of treatment with Lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment. [see Clinical Studies ( )] 14.2
-
Dr. Reddy’s Laboratories Limited
![Lamotrigine Tablet, Chewable [Dr. Reddy’s Laboratories Limited]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Dr. Reddy's Laboratories Limited
![Lamotrigine Tablet, Chewable [Dr. Reddy’s Laboratories Limited] Lamotrigine Tablet, Chewable [Dr. Reddy’s Laboratories Limited]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets (chewable, dispersible) with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets (chewable, dispersible), or (3) exceeding the recommended dose escalation for lamotrigine tablets (chewable, dispersible). However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablets (chewable, dispersible) is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets (chewable, dispersible) not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets (chewable, dispersible) may require adjustment based on clinical response.
Target Plasma Levels for Patients with Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets (chewable, dispersible) should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives:
Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets (chewable, dispersible) should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets (chewable, dispersible) based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets (chewable, dispersible) in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets (chewable, dispersible) will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets (chewable, dispersible) and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets (chewable, dispersible) consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking lamotrigine tablets (chewable, dispersible) in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets (chewable,dispersible) should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets (chewable, dispersible) will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets (chewable, dispersible) should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine tablets (chewable, dispersible) in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets (chewable, dispersible) should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets (chewable, dispersible) in the presence of progestogens alone will likely not be needed.
Patients with Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients with Renal Impairment: Initial doses of lamotrigine tablets (chewable, dispersible) should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets (chewable, dispersible). Because there is inadequate experience in this population, lamotrigine tablets (chewable, dispersible) should be used with caution in these patients.
Discontinuation Strategy:
Epilepsy: For patients receiving lamotrigine tablets (chewable, dispersible) in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets (chewable, dispersible), a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets (chewable, dispersible). In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets (chewable, dispersible). However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets (chewable, dispersible) should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions(5.9)].
2.2 Epilepsy - Adjunctive TherapymThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy
For Patients TAKING Valproatea For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidoneb, or Valproatea FFor Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day
(in 2 divided doses) Weeks 5 onwards to maintenance Increase by 25 to 50 mg/day
every 1 to 2 weeks Increase by 50 mg/day
every 1 to 2 weeks Increase by100 mg/day
every 1 to2 weeks. Usual Maintenance Dose 100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induceglucuronidation
(in 1 or 2 divided doses) 225 to 375 mg/day
(in 2 divided doses) 300 to 500 mg/day
(in 2 divided doses)a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
The smallest available strength of lamotrigine tablets (chewable, dispersible) is 2 mg, and only whole tablets should be administered. If the calculated dose cannot be achieved using whole tablets, the dose should be rounded down to the nearest whole tablet [seeHow Supplied/Storage and Handling (16) and Medication Guide].
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy
For Patients TAKING Valproatea For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidoneb, or Valproatea For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea Weeks 1 and 2 0.15 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet Weeks 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual Maintenance Dose 1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses).1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day(maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical responseNote: Only whole tablets should be used for dosing.
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy
If the patient’s weight is Give this daily dose, using the most appropriate combination of lamotrigine 2-mg and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets (chewable, dispersible) was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets (chewable, dispersible) as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets (chewable, dispersible) as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion from Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets (chewable, dispersible) under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets (chewable, dispersible).
The recommended maintenance dose of lamotrigine tablets (chewable, dispersible) as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets (chewable, dispersible) should not be exceeded [see Boxed Warning].
Conversion from Adjunctive Therapy with Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy with Lamotrigine: After achieving a dose of 500 mg/day of lamotrigine tablets (chewable, dispersible) according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy with Valproate to Monotherapy with Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age with Epilepsy
Lamotrigine Valproate Step 1 Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day). Maintain previous stable dose. Step 2 Maintain at 200 mg/day. Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week. Step 3 Increase to 300 mg/day and maintain for 1 week. Simultaneously decrease to 250 mg/day and maintain for 1 week. Step 4 Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day. Discontinue.Conversion from Adjunctive Therapy with AEDs other than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy with Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets (chewable, dispersible) with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine tablets (chewable, dispersible) is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets (chewable, dispersible) is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that which increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets (chewable, dispersible) is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets (chewable, dispersible) should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets (chewable, dispersible) should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine tablets (chewable, dispersible) should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets (chewable, dispersible) may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets (chewable, dispersible) may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets (chewable, dispersible) [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets (chewable, dispersible) should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder
For Patients TAKING Valproatea For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidoneb or Valproatea For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone and NOT TAKING Valproatea Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided dosesa Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions 7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions 7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications
Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidoneb ,or Valproatea) After Discontinuation of Valproatea After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb Current dose of lamotrigine (mg/day)
100 Current dose of lamotrigine (mg/day)
400 Week 1 Maintain current dose of lamotrigine 150 400 Week 2 Maintain current dose of lamotrigine 200 300 Week 3 onward Maintain current dose of lamotrigine 200 200a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions 7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions 7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine tablets (chewable, dispersible) was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies(14.2)]. However, the optimal duration of treatment with lamotrigine tablets (chewable, dispersible) has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
2.5 Administration of Lamotrigine Tablets (chewable, dispersible)Lamotrigine tablets (chewable, dispersible) may be swallowed whole, chewed, or dispersed in water or diluted fruit juice. If the tablets are chewed, consume a small amount of water or diluted fruit juice to aid in swallowing.
To disperse lamotrigine tablets (chewable, dispersible), add the tablets to a small amount of liquid (1 teaspoon, or enough to cover the medication). Approximately 1 minute later, when the tablets are completely dispersed, swirl the solution and consume the entire quantity immediately. No attempt should be made to administer partial quantities of the dispersed tablets.
-
Dr.reddy’s Laboratories Limited
![Lamotrigine Tablet [Dr.reddy’s Laboratories Limited]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Dr.reddy's Laboratories Limited
![Lamotrigine Tablet [Dr.reddy’s Laboratories Limited] Lamotrigine Tablet [Dr.reddy’s Laboratories Limited]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablets is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets may require adjustment based on clinical response.
Target Plasma Levels for Patients with Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives:(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.
Patients with Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients with Renal Impairment: Initial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine tablets in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy - Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy
For Patients TAKING Valproate a For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidoneb, or Valproatea For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day
(in 2 divided doses) Weeks 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks. Usual maintenance dose 100 to 200 mg/day with valproate alone 100 to 400 mg/day with valproate and other drugs that induceglucuronication
(in 1 or 2 divided doses) 225 to 375 mg/day
(in 2 divided doses) 300 to 500 mg/day
(in 2 divided doses)a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce glucuronidation and increase clearance [see Drug Interactions (7) Clinical Pharmacology (12.3)]. Other drugs, that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7),Clinical Pharmacology (12.3)].
Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect..
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2. Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy
For Patients TAKING Valproatea For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidoneb, or Valproatea For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea Weeks 1 and 2 0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide) 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide) 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual maintenance dose 1 to 5 mg/kg/day
(maximum 200 mg/day in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day
(maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as such much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical responseNote: Only whole tablets should be used for dosing.
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce glucuronidation and increase clearance [see Drug Interactions (7)Clinical Pharmacology (12.3)]. Other drugs, that have similar effects include estrogen-containing oral contraceptives and rifampin [see Drug Interactions (7),Clinical Pharmacology Pharmacokinetics (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect..
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy
If the patient’s weight is Give this daily dose, using the most appropriate combination of lamotrigine 2 mg and 5 mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy - Conversion from Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion from Adjunctive Therapy with Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy with Lamotrigine: After achieving a dose of 500 mg/day of lamotrigine tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy with Valproate to Monotherapy with Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age with Epilepsy
Lamotrigine Valproate Step 1 Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day). Maintain previous stable dose. Step 2 Maintain at 200 mg/day. Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week. Step 3 Increase to 300 mg/day and maintain for 1 week. Simultaneously decrease to 250 mg/day and maintain for 1 week. Step 4 Increase by 100 mg/day every week to achieve maintenance dose of
500 mg/day. Discontinue.Conversion from Adjunctive Therapy with Antiepileptic Drugs other than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy with Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients with Bipolar Disorder
For Patients TAKING Valproatea For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidoneb, Valproatea For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb, and NOT TAKING Valproatea Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided dosesa Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 6. Dosage Adjustments to Lamotrigine for Patients with Bipolar Disorder Following Discontinuation of Psychotropic Medications
Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidoneb, or Valproatea) After Discontinuation of Valproatea After Discontinuation of Valproatea Current dose of lamotrigine (mg/day) 100 Current dose of lamotrigine (mg/day) 400 Week 1 Maintain current dose of lamotrigine 150 400 Week 2 Maintain current dose of lamotrigine 200 300 Week 3 onward Maintain current dose of lamotrigine 200 200a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine tablets was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Bryant Ranch Prepack
![Lamotrigine Tablet [Bryant Ranch Prepack]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Bryant Ranch Prepack
![Lamotrigine Tablet [Bryant Ranch Prepack] Lamotrigine Tablet [Bryant Ranch Prepack]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablets is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine tablets will in most cases need to be increased, by as much as 2 fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose will in most cases need to be increased by as much as 2 fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (seeTable 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment should be necessary to the dose of lamotrigine tablets.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2 week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2 fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1 to 3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine tablets in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, or primidone should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ see Drug Interactions (7), Pharmacokinetics (12.3)] . † These drugs induce glucuronidation and increase clearance [ see Drug Interactions (7) Pharmacokinetics (12.3)]. Other drugs, which have similar effects include estrogen-containing oral contraceptives and rifampin [ see Drug Interactions (7), Pharmacokinetics (12.3)] . Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [ see Dosage and Administration (2.1)] . Patients on rifampin should follow the same dosing titration/maintenance regimen used with drugs that induce glucuronidation and increase clearance. For Patients Taking Valproate* For Patients Taking AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, or Primidone†, and Not Taking Valproate For Patients Taking Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and Not Taking Valproate Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day (in 2 divided doses) Weeks 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks Usual Maintenance Dose100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronication
(in 1 or 2 divided doses)
225 to 375 mg/day (in 2 divided doses)300 to 500 mg/day
(in 2 divided doses)
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy For Patients Taking Valproate* For Patients Taking AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, or Primidone† , and Not Taking Valproate For Patients Taking Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and Not Taking Valproate Weeks 1 and 2 0.15 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3for weight based dosing guide) 0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet Weeks 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual Maintenance Dose 1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day (maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical responseNote: Only whole tablets should be used for dosing .
* Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Pharmacokinetics (12.3)].
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of lamotrigine tablets, 2 mg and 5 mg Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every day
† These drugs induce glucuronidation and increase clearance [see Drug Interactions (7) Pharmacokinetics (12.3)]. Other drugs, which have similar effects include estrogen-containing oral contraceptives and rifampin [see Drug Interactions (7), Pharmacokinetics (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin should follow the same dosing titration/maintenance regimen used with drugs that induce glucuronidation.Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets: After achieving a dose of 500 mg/day of lamotrigine tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4 week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age with Epilepsy
Lamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion From Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, which increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2 week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2 week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder* * See Drug Interactions (7) and Clinical Pharmacology (12.3) for a description of known drug interactions. † Valproate has been shown to decrease the apparent clearance of lamotrigine. ‡ Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine. For Patients Taking Valproate† For Patients Not Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Rifampin‡ and Not Taking Valproate† For Patients Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Rifampin‡ and Not Taking Valproate† Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications* * See Drug Interactions (7) and Clinical Pharmacology (12.3) for a description of known drug interactions. † Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine. ‡ Valproate has been shown to decrease the apparent clearance of lamotrigine. Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone, Rifampin†, or Valproate‡) After Discontinuation of Valproate‡ After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Rifampin† Current dose of Lamotrigine (mg/day) 100Current dose of Lamotrigine (mg/day)
400
Week 1 Maintain current dose of lamotrigine 150 400 Week 2 Maintain current dose of lamotrigine 200 300 Week 3 onward Maintain current dose of lamotrigine 200 200The benefit of continuing treatment in patients who had been stabilized in an 8 to 16 week open-label phase with lamotrigine tablets was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Bryant Ranch Prepack
![Lamotrigine Tablet [Bryant Ranch Prepack]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Bryant Ranch Prepack
![Lamotrigine Tablet [Bryant Ranch Prepack] Lamotrigine Tablet [Bryant Ranch Prepack]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablets is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine tablets will in most cases need to be increased, by as much as 2 fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose will in most cases need to be increased by as much as 2 fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (seeTable 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment should be necessary to the dose of lamotrigine tablets.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2 week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2 fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1 to 3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine tablets in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, or primidone should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ see Drug Interactions (7), Pharmacokinetics (12.3)] . † These drugs induce glucuronidation and increase clearance [ see Drug Interactions (7) Pharmacokinetics (12.3)]. Other drugs, which have similar effects include estrogen-containing oral contraceptives and rifampin [ see Drug Interactions (7), Pharmacokinetics (12.3)] . Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [ see Dosage and Administration (2.1)] . Patients on rifampin should follow the same dosing titration/maintenance regimen used with drugs that induce glucuronidation and increase clearance. For Patients Taking Valproate* For Patients Taking AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, or Primidone†, and Not Taking Valproate For Patients Taking Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and Not Taking Valproate Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day (in 2 divided doses) Weeks 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks Usual Maintenance Dose100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronication
(in 1 or 2 divided doses)
225 to 375 mg/day (in 2 divided doses)300 to 500 mg/day
(in 2 divided doses)
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy For Patients Taking Valproate* For Patients Taking AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, or Primidone† , and Not Taking Valproate For Patients Taking Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and Not Taking Valproate Weeks 1 and 2 0.15 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3for weight based dosing guide) 0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet Weeks 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual Maintenance Dose 1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day (maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical responseNote: Only whole tablets should be used for dosing .
* Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Pharmacokinetics (12.3)].
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of lamotrigine tablets, 2 mg and 5 mg Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every day
† These drugs induce glucuronidation and increase clearance [see Drug Interactions (7) Pharmacokinetics (12.3)]. Other drugs, which have similar effects include estrogen-containing oral contraceptives and rifampin [see Drug Interactions (7), Pharmacokinetics (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin should follow the same dosing titration/maintenance regimen used with drugs that induce glucuronidation.Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets: After achieving a dose of 500 mg/day of lamotrigine tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4 week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age with Epilepsy
Lamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion From Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, which increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2 week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or rifampin, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2 week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder* * See Drug Interactions (7) and Clinical Pharmacology (12.3) for a description of known drug interactions. † Valproate has been shown to decrease the apparent clearance of lamotrigine. ‡ Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine. For Patients Taking Valproate† For Patients Not Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Rifampin‡ and Not Taking Valproate† For Patients Taking Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Rifampin‡ and Not Taking Valproate† Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications* * See Drug Interactions (7) and Clinical Pharmacology (12.3) for a description of known drug interactions. † Carbamazepine, phenytoin, phenobarbital, primidone, and rifampin have been shown to increase the apparent clearance of lamotrigine. ‡ Valproate has been shown to decrease the apparent clearance of lamotrigine. Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone, Rifampin†, or Valproate‡) After Discontinuation of Valproate‡ After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Rifampin† Current dose of Lamotrigine (mg/day) 100Current dose of Lamotrigine (mg/day)
400
Week 1 Maintain current dose of lamotrigine 150 400 Week 2 Maintain current dose of lamotrigine 200 300 Week 3 onward Maintain current dose of lamotrigine 200 200The benefit of continuing treatment in patients who had been stabilized in an 8 to 16 week open-label phase with lamotrigine tablets was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Wockhardt Usa Llc.
![Lamotrigine Tablet, Extended Release [Wockhardt Usa Llc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Wockhardt Usa Llc.
![Lamotrigine Tablet, Extended Release [Wockhardt Usa Llc.] Lamotrigine Tablet, Extended Release [Wockhardt Usa Llc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine extended-release tablets are taken once daily, with or without food. Tablets must be swallowed whole and must not be chewed, crushed, or divided.
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine extended-release tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine extended-release tablets, or (3) exceeding the recommended dose escalation for lamotrigine extended-release tablets. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation for lamotrigine extended-release tablet is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine extended-release tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine extended-release tablets, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Extended-Release Tablets Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine extended-release tablets may require adjustment based on clinical response.
Target Plasma Levels: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine extended-release tablets should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Extended-Release Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine extended-release tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine extended-release tablets based on the concomitant AED or other concomitant medications (see Table 1). See below for adjustments to maintenance doses of lamotrigine extended-release tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Extended-Release Tablets in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions, (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine extended-release tablets will in most cases need to be increased by as much as 2-fold over the recommended target maintenance dose in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine extended-release tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (pill-free week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine extended-release tablets consistently occur during the pill-free week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the pill-free week are not recommended. For women taking lamotrigine extended-release tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine extended-release tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine extended-release tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine extended-release tablets should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine extended-release tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine extended-release tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine extended-release tablets in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine extended-release tablets should be based on patients’ concomitant medications (see Table 1); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with immediate-release lamotrigine. Because there is inadequate experience in this population, lamotrigine extended-release tablets should be used with caution in these patients.
Discontinuation Strategy: For patients receiving lamotrigine extended-release tablets in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine extended-release tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.8)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
2.2 Adjunctive Therapy for Partial Onset SeizuresThis section provides specific dosing recommendations for patients ≥13 years of age. Specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications.
Table 1. Escalation Regimen for Lamotrigine Extended-Release Tablets in Patients ≥13 Years of Agea Valproate has been shown to inhibit glucuronidation and decrease the apparent
clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce glucuronidation and increase clearance [see Drug Interactions (7),
Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-
containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)].
Dosing recommendations for oral contraceptives can be found in General Dosing
Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs
that induce lamotrigine glucuronidation and increase clearance, should follow the same
dosing titration/maintenance regimen as that used with anticonvulsants that have this
effect.
c Dose increases at week 8 or later should not exceed 100 mg daily at weekly intervals.
For Patients TAKING
Valproatea
For Patients NOT
TAKING Carbamazepine,
Phenytoin, Phenobarbital,
Primidoneb, or
Valproatea
For Patients TAKING
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidoneb and NOT
TAKING Valproatea
Weeks 1 and 2
25 mg every
other day
25 mg every day
50 mg every day
Weeks 3 and 4
25 mg every day
50 mg every day
100 mg every day
Week 5
50 mg every day
100 mg every day
200 mg every day
Week 6
100 mg every day
150 mg every day
300 mg every day
Week 7
150 mg every day
200 mg every day
400 mg every day
Maintenance range
(week 8 and
onward)
200 to 250 mg
every dayc
300 to 400 mg
every dayc
400 to 600 mg
every dayc
2.3 2.3 2.4 Conversion From Immediate-Release Lamotrigine Tablets to Lamotrigine Extended-Release TabletsPatients may be converted directly from immediate-release lamotrigine to lamotrigine extended-release tablets. The initial dose of lamotrigine extended-release tablets should match the total daily dose of immediate-release lamotrigine. However, some subjects on concomitant enzyme-inducing agents may have lower plasma levels of lamotrigine on conversion and should be monitored [see Clinical Pharmacology (12.3)].
Following conversion to lamotrigine extended-release tablets, all patients (but especially those on drugs that induce lamotrigine glucuronidation) should be closely monitored for seizure control [see Drug Interactions (7)]. Depending on the therapeutic response after conversion, the total daily dose may need to be adjusted within the recommended dosing instructions (Table 1).
-
Wockhardt Limited
![Lamotrigine Tablet, Extended Release [Wockhardt Limited]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Wockhardt Limited
![Lamotrigine Tablet, Extended Release [Wockhardt Limited] Lamotrigine Tablet, Extended Release [Wockhardt Limited]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine extended-release tablets are taken once daily, with or without food. Tablets must be swallowed whole and must not be chewed, crushed, or divided.
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine extended-release tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine extended-release tablets, or (3) exceeding the recommended dose escalation for lamotrigine extended-release tablets. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation for lamotrigine extended-release tablet is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine extended-release tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine extended-release tablets, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Extended-Release Tablets Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine extended-release tablets may require adjustment based on clinical response.
Target Plasma Levels: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine extended-release tablets should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Extended-Release Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine extended-release tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine extended-release tablets based on the concomitant AED or other concomitant medications (see Table 1). See below for adjustments to maintenance doses of lamotrigine extended-release tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Extended-Release Tablets in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions, (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine extended-release tablets will in most cases need to be increased by as much as 2-fold over the recommended target maintenance dose in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine extended-release tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (pill-free week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine extended-release tablets consistently occur during the pill-free week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the pill-free week are not recommended. For women taking lamotrigine extended-release tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine extended-release tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine extended-release tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine extended-release tablets should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine extended-release tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine extended-release tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine extended-release tablets in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine extended-release tablets should be based on patients’ concomitant medications (see Table 1); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with immediate-release lamotrigine. Because there is inadequate experience in this population, lamotrigine extended-release tablets should be used with caution in these patients.
Discontinuation Strategy: For patients receiving lamotrigine extended-release tablets in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine extended-release tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.8)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
2.2 Adjunctive Therapy for Partial Onset SeizuresThis section provides specific dosing recommendations for patients ≥13 years of age. Specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications.
Table 1. Escalation Regimen for Lamotrigine Extended-Release Tablets in Patients ≥13 Years of Agea Valproate has been shown to inhibit glucuronidation and decrease the apparent
clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce glucuronidation and increase clearance [see Drug Interactions (7),
Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-
containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)].
Dosing recommendations for oral contraceptives can be found in General Dosing
Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs
that induce lamotrigine glucuronidation and increase clearance, should follow the same
dosing titration/maintenance regimen as that used with anticonvulsants that have this
effect.
c Dose increases at week 8 or later should not exceed 100 mg daily at weekly intervals.
For Patients TAKING
Valproatea
For Patients NOT
TAKING Carbamazepine,
Phenytoin, Phenobarbital,
Primidoneb, or
Valproatea
For Patients TAKING
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidoneb and NOT
TAKING Valproatea
Weeks 1 and 2
25 mg every
other day
25 mg every day
50 mg every day
Weeks 3 and 4
25 mg every day
50 mg every day
100 mg every day
Week 5
50 mg every day
100 mg every day
200 mg every day
Week 6
100 mg every day
150 mg every day
300 mg every day
Week 7
150 mg every day
200 mg every day
400 mg every day
Maintenance range
(week 8 and
onward)
200 to 250 mg
every dayc
300 to 400 mg
every dayc
400 to 600 mg
every dayc
2.3 2.3 2.4 Conversion From Immediate-Release Lamotrigine Tablets to Lamotrigine Extended-Release TabletsPatients may be converted directly from immediate-release lamotrigine to lamotrigine extended-release tablets. The initial dose of lamotrigine extended-release tablets should match the total daily dose of immediate-release lamotrigine. However, some subjects on concomitant enzyme-inducing agents may have lower plasma levels of lamotrigine on conversion and should be monitored [see Clinical Pharmacology (12.3)].
Following conversion to lamotrigine extended-release tablets, all patients (but especially those on drugs that induce lamotrigine glucuronidation) should be closely monitored for seizure control [see Drug Interactions (7)]. Depending on the therapeutic response after conversion, the total daily dose may need to be adjusted within the recommended dosing instructions (Table 1).
-
Upsher-smith Laboratories, Inc.
![Lamotrigine Tablet Lamotrigine Kit [Upsher-smith Laboratories, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Upsher-smith Laboratories, Inc.
![Lamotrigine Tablet Lamotrigine Kit [Upsher-smith Laboratories, Inc.] Lamotrigine Tablet Lamotrigine Kit [Upsher-smith Laboratories, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of Lamotrigine Tablets is exceeded and in patients with a history of allergy or rash to other AEDs.
Lamotrigine Tablets Starter Kits provide Lamotrigine Tablets at doses consistent with the recommended titration schedule for the first 5 weeks of treatment, based upon concomitant medications for patients with epilepsy (>12 years of age) and Bipolar I Disorder (≥18 years of age) and are intended to help reduce the potential for rash. The use of Lamotrigine Tablets Starter Kits is recommended for appropriate patients who are starting or restarting Lamotrigine Tablets [see How Supplied/Storage and Handling (16)].
It is recommended that Lamotrigine Tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Tablets Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of Lamotrigine Tablets may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of Lamotrigine Tablets should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for Lamotrigine Tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with Lamotrigine Tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of Lamotrigine Tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of Lamotrigine Tablets will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of Lamotrigine Tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to Lamotrigine Tablets consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking Lamotrigine Tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of Lamotrigine Tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of Lamotrigine Tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of Lamotrigine Tablets should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking Lamotrigine Tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of Lamotrigine Tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of Lamotrigine Tablets in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of Lamotrigine Tablets should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with Lamotrigine Tablets. Because there is inadequate experience in this population, Lamotrigine Tablets should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving Lamotrigine Tablets in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with Lamotrigine Tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of Lamotrigine Tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine Tablets in Patients Over 12 Years of Age With Epilepsy For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [ see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day
(in 2 divided doses) Week 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks Usual maintenance dose 100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation (in 1 or 2 divided doses) 225 to 375 mg/day
(in 2 divided doses) 300 to 500 mg/day
(in 2 divided doses)Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine Tablets in Patients 2 to 12 Years of Age With Epilepsy For Patients TAKING Valproate*
For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Note: Only whole tablets should be used for dosing. * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. Weeks 1 and 2 0.15 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide) 0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide) 0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet Week 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual maintenance dose 1 to 5 mg/kg/day
(maximum 200 mg/day in 1 or 2 divided doses)
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day
(maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years of Age Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient's weight is Give this daily dose, using the most appropriate combination of Lamotrigine Tablets 2 mg and 5 mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with Lamotrigine Tablets under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of Lamotrigine Tablets.
The recommended maintenance dose of Lamotrigine Tablets as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine Tablets should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets: After achieving a dose of 500 mg/day of Lamotrigine Tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets in Patients ≥16 Years of Age With Epilepsy Lamotrigine Tablets Valproate Step 1 Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day). Maintain previous stable dose. Step 2 Maintain at 200 mg/day. Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week. Step 3 Increase to 300 mg/day and maintain for 1 week. Simultaneously decrease to 250 mg/day and maintain for 1 week. Step 4 Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day. Discontinue.Conversion From Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets: No specific dosing guidelines can be provided for conversion to monotherapy with Lamotrigine Tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with Lamotrigine Tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of Lamotrigine Tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with Lamotrigine Tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of Lamotrigine Tablets should be adjusted. For patients discontinuing valproate, the dose of Lamotrigine Tablets should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of Lamotrigine Tablets should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of Lamotrigine Tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of Lamotrigine Tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of Lamotrigine Tablets [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine Tablets should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine Tablets for Patients With Bipolar Disorder For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,† or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone,† and NOT TAKING Valproate* * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to Lamotrigine Tablets for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone,* or Valproate†) After Discontinuation of Valproate† After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone* Current dose of Lamotrigine Tablets (mg/day) 100 Current dose of Lamotrigine Tablets (mg/day) 400 * These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. † Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Week 1 Maintain current dose of Lamotrigine Tablets 150 400 Week 2 Maintain current dose of Lamotrigine Tablets 200 300 Week 3 onward Maintain current dose of Lamotrigine Tablets 200 200The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Bryant Ranch Prepack
![Lamotrigine (Lamotrigine) Tablet [Bryant Ranch Prepack]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Bryant Ranch Prepack
![Lamotrigine (Lamotrigine) Tablet [Bryant Ranch Prepack] Lamotrigine (Lamotrigine) Tablet [Bryant Ranch Prepack]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of Lamotrigine with valproate, (2) exceeding the recommended initial dose of Lamotrigine, or (3) exceeding the recommended dose escalation for Lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of Lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that Lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with Lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued Lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued Lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of Lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with Lamotrigine. Because Lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of Lamotrigine and doses of Lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for Lamotrigine. Dosing of Lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of Lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for Lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with Lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of Lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of Lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent Lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of Lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent Lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless Lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in Lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased Lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to Lamotrigine consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of Lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of Lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent Lamotrigine plasma level. The decrease in dose of Lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or Lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of Lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of Lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of Lamotrigine up to 2-fold, and the progestin-only pills had no effect on Lamotrigine plasma levels. Therefore, adjustments to the dosage of Lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of Lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with Lamotrigine. Because there is inadequate experience in this population, Lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving Lamotrigine in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse experiences is observed.
If a decision is made to discontinue therapy with Lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation should prolong the half-life of Lamotrigine; discontinuing valproate should shorten the half-life of Lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of Lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of Lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of Lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine [see Drug Interactions ( 7 ), Clinical Pharmacology ( 12.3 )]. † These drugs induce Lamotrigine glucuronidation and increase clearance [see Drug Interactions ( 7 ) Clinical Pharmacology ( 12.3 )]. Other drugs, which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions ( 7 ), Clinical Pharmacology ( 12.3 )]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration ( 2.1 )]. Patients on rifampin, or other drugs that induce Lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†,or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day (in 2 divided doses) Weeks 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day
every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks Usual Maintenance Dose 100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronication
(in 1 or 2 divided doses) 225 to 375 mg/day
(in 2 divided doses) 300 to 500 mg/day (in 2 divided doses)Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine [see Drug Interactions (7 ), Clinical Pharmacology (12.3)]. † These drugs induce Lamotrigine glucuronidation and increase clearance [see Drug Interactions (7 ) Clinical Pharmacology (12.3)]. Other drugs, which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7 ) Clinical Pharmacology (12.3)].
Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce Lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine,
Phenytoin,
Phenobarbital,
Primidone† or
Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Weeks 1 and 2 0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual Maintenance Dose 1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day
(maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response Note: Only whole tablets should be used for dosing. Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of Lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive Lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive Lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with Lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of Lamotrigine.
The recommended maintenance dose of Lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of Lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age with EpilepsyLamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
2.4 Bipolar Disorder
Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with Lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.The goal of maintenance treatment with Lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of Lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of Lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin, that increase the apparent clearance of Lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with Lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of Lamotrigine should be adjusted. For patients discontinuing valproate, the dose of Lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation, the dose of Lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of Lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of Lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of Lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine [see Drug Interactions (7 ), Clinical Pharmacology (12.3)]. † These drugs induce Lamotrigine glucuronidation and increase clearance [see Drug Interactions (7 ), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen- containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)].
Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce Lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/ maintenance regimen as that used with anticonvulsants that have this effect. For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications * These drugs induce Lamotrigine glucuronidation and increase clearance [see Drug Interactions (7 ), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce Lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/ maintenance regimen as that used with anticonvulsants that have this effect. † Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone*, or Valproate†)
After Discontinuation of Valproate† After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone* Current dose of Lamotrigine (mg/day) 100Current dose of Lamotrigine (mg/day) 400
Week 1 Maintain current dose of Lamotrigine 150 400 Week 2 Maintain current dose of Lamotrigine 200 300 Week 3 onward Maintain current dose of Lamotrigine 200 200The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with Lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with Lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ] Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Rash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of Lamotrigine with valproate, (2) exceeding the recommended initial dose of Lamotrigine, or (3) exceeding the recommended dose escalation for Lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of Lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that Lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with Lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued Lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued Lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of Lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with Lamotrigine. Because Lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of Lamotrigine and doses of Lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for Lamotrigine. Dosing of Lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of Lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for Lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with Lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of Lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of Lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent Lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of Lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent Lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless Lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in Lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased Lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to Lamotrigine consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of Lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of Lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent Lamotrigine plasma level. The decrease in dose of Lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or Lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of Lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of Lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of Lamotrigine up to 2-fold, and the progestin-only pills had no effect on Lamotrigine plasma levels. Therefore, adjustments to the dosage of Lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of Lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with Lamotrigine. Because there is inadequate experience in this population, Lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving Lamotrigine in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse experiences is observed.
If a decision is made to discontinue therapy with Lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation should prolong the half-life of Lamotrigine; discontinuing valproate should shorten the half-life of Lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of Lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of Lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of Lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
This section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†,or Valproate1 For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone2 and NOT TAKING Valproate1 Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day (in 2 divided doses) Weeks 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day
every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks Usual Maintenance Dose 100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronication
(in 1 or 2 divided doses) 225 to 375 mg/day
(in 2 divided doses) 300 to 500 mg/day (in 2 divided doses)
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine,
Phenytoin,
Phenobarbital,
Primidone† or
Valproate3 For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone4 and NOT TAKING Valproate3 Weeks 1 and 2 0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual Maintenance Dose 1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day
(maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response Note: Only whole tablets should be used for dosing.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of Lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive Lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive Lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
The goal of the transition regimen is to effect the conversion to monotherapy with Lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of Lamotrigine.
The recommended maintenance dose of Lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of Lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age with EpilepsyLamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with Lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.The goal of maintenance treatment with Lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of Lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of Lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin, that increase the apparent clearance of Lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with Lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of Lamotrigine should be adjusted. For patients discontinuing valproate, the dose of Lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation, the dose of Lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of Lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of Lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of Lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate5 For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone6 and NOT TAKING Valproate5 Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses
Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic MedicationsDiscontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone*, or Valproate†)
After Discontinuation of Valproate8 After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone7 Current dose of Lamotrigine (mg/day) 100Current dose of Lamotrigine (mg/day) 400
Week 1 Maintain current dose of Lamotrigine 150 400 Week 2 Maintain current dose of Lamotrigine 200 300 Week 3 onward Maintain current dose of Lamotrigine 200 200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with Lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with Lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
1 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine 2 These drugs induce Lamotrigine glucuronidation and increase clearance 3 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine 4 These drugs induce Lamotrigine glucuronidation and increase clearance 5 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine 6 These drugs induce Lamotrigine glucuronidation and increase clearance 7 These drugs induce Lamotrigine glucuronidation and increase clearance 8 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine -
Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ] Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Rash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
Lamotrigine Starter Kits provide lamotrigine at doses consistent with the recommended titration schedule for the first 5 weeks of treatment, based upon concomitant medications for patients with epilepsy (>12 years of age) and Bipolar I Disorder (≥18 years of age) and are intended to help reduce the potential for rash. The use of Lamotrigine Starter Kits is recommended for appropriate patients who are starting or restarting lamotrigine [see How Supplied/Storage and Handling (16)].
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
This section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy For Patients TAKING Valproate * For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate1 For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone2 and NOT TAKING Valproate1 Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day
(in 2 divided doses) Week 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks Usual maintenance dose 100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses) 225 to 375 mg/day
(in 2 divided doses) 300 to 500 mg/day
(in 2 divided doses)Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy For Patients TAKING Valproate * For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate3 For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone4 and NOT TAKING Valproate3 Weeks 1 and 2 0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Week 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual maintenance dose 1 to 5 mg/kg/day
(maximum 200 mg/day in 1 or 2 divided doses)
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day
(maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical responseDosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient's weight is Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
The goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age With Epilepsy Lamotrigine Valproate Step 1 Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day). Maintain previous stable dose. Step 2 Maintain at 200 mg/day. Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week. Step 3 Increase to 300 mg/day and maintain for 1 week. Simultaneously decrease to 250 mg/day and maintain for 1 week. Step 4 Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day. Discontinue.Conversion From Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
The goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate5 For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone6, and NOT TAKING Valproate5 Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone*, or Valproate†) After Discontinuation of Valproate8 After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital or Primidone7 Current dose of Lamotrigine (mg/day) 100 Current dose of Lamotrigine (mg/day) 400 Week 1 Maintain current dose of Lamotrigine 150 400 Week 2 Maintain current dose of Lamotrigine 200 300 Week 3 onward Maintain current dose of Lamotrigine 200 200The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
1 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine 2 These drugs induce lamotrigine glucuronidation and increase clearance 3 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine 4 These drugs induce lamotrigine glucuronidation and increase clearance 5 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine 6 These drugs induce lamotrigine glucuronidation and increase clearance 7 These drugs induce lamotrigine glucuronidation and increase clearance 8 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine -
Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ] Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Rash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of Lamotrigine with valproate, (2) exceeding the recommended initial dose of Lamotrigine, or (3) exceeding the recommended dose escalation for Lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of Lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that Lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with Lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued Lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued Lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of Lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with Lamotrigine. Because Lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of Lamotrigine and doses of Lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for Lamotrigine. Dosing of Lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of Lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for Lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with Lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of Lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of Lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent Lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of Lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent Lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless Lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in Lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased Lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to Lamotrigine consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of Lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of Lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent Lamotrigine plasma level. The decrease in dose of Lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or Lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of Lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of Lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of Lamotrigine up to 2-fold, and the progestin-only pills had no effect on Lamotrigine plasma levels. Therefore, adjustments to the dosage of Lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of Lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with Lamotrigine. Because there is inadequate experience in this population, Lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving Lamotrigine in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse experiences is observed.
If a decision is made to discontinue therapy with Lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation should prolong the half-life of Lamotrigine; discontinuing valproate should shorten the half-life of Lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of Lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of Lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of Lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
This section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†,or Valproate1 For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone2 and NOT TAKING Valproate1 Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day (in 2 divided doses) Weeks 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day
every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks Usual Maintenance Dose 100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronication
(in 1 or 2 divided doses) 225 to 375 mg/day
(in 2 divided doses) 300 to 500 mg/day (in 2 divided doses)
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine,
Phenytoin,
Phenobarbital,
Primidone† or
Valproate3 For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone4 and NOT TAKING Valproate3 Weeks 1 and 2 0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual Maintenance Dose 1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day
(maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response Note: Only whole tablets should be used for dosing.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of Lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive Lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive Lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
The goal of the transition regimen is to effect the conversion to monotherapy with Lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of Lamotrigine.
The recommended maintenance dose of Lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of Lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age with EpilepsyLamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with Lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.The goal of maintenance treatment with Lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of Lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of Lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin, that increase the apparent clearance of Lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with Lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of Lamotrigine should be adjusted. For patients discontinuing valproate, the dose of Lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation, the dose of Lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of Lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of Lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of Lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate5 For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone6 and NOT TAKING Valproate5 Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses
Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic MedicationsDiscontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone*, or Valproate†)
After Discontinuation of Valproate8 After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone7 Current dose of Lamotrigine (mg/day) 100Current dose of Lamotrigine (mg/day) 400
Week 1 Maintain current dose of Lamotrigine 150 400 Week 2 Maintain current dose of Lamotrigine 200 300 Week 3 onward Maintain current dose of Lamotrigine 200 200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with Lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with Lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
1 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine 2 These drugs induce Lamotrigine glucuronidation and increase clearance 3 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine 4 These drugs induce Lamotrigine glucuronidation and increase clearance 5 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine 6 These drugs induce Lamotrigine glucuronidation and increase clearance 7 These drugs induce Lamotrigine glucuronidation and increase clearance 8 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine -
Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ] Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Rash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of Lamotrigine with valproate, (2) exceeding the recommended initial dose of Lamotrigine, or (3) exceeding the recommended dose escalation for Lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of Lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that Lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with Lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued Lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued Lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of Lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with Lamotrigine. Because Lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of Lamotrigine and doses of Lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for Lamotrigine. Dosing of Lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of Lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for Lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with Lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of Lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of Lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent Lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of Lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent Lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless Lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in Lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased Lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to Lamotrigine consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of Lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of Lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent Lamotrigine plasma level. The decrease in dose of Lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or Lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of Lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of Lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of Lamotrigine up to 2-fold, and the progestin-only pills had no effect on Lamotrigine plasma levels. Therefore, adjustments to the dosage of Lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of Lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with Lamotrigine. Because there is inadequate experience in this population, Lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving Lamotrigine in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse experiences is observed.
If a decision is made to discontinue therapy with Lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation should prolong the half-life of Lamotrigine; discontinuing valproate should shorten the half-life of Lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of Lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of Lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of Lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
This section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†,or Valproate1 For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone2 and NOT TAKING Valproate1 Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day (in 2 divided doses) Weeks 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day
every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks Usual Maintenance Dose 100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronication
(in 1 or 2 divided doses) 225 to 375 mg/day
(in 2 divided doses) 300 to 500 mg/day (in 2 divided doses)
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine,
Phenytoin,
Phenobarbital,
Primidone† or
Valproate3 For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone4 and NOT TAKING Valproate3 Weeks 1 and 2 0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual Maintenance Dose 1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day
(maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response Note: Only whole tablets should be used for dosing.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of Lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive Lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive Lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
The goal of the transition regimen is to effect the conversion to monotherapy with Lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of Lamotrigine.
The recommended maintenance dose of Lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of Lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age with EpilepsyLamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with Lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.The goal of maintenance treatment with Lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of Lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of Lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin, that increase the apparent clearance of Lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with Lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of Lamotrigine should be adjusted. For patients discontinuing valproate, the dose of Lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation, the dose of Lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of Lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of Lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of Lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate5 For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone6 and NOT TAKING Valproate5 Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses
Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic MedicationsDiscontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone*, or Valproate†)
After Discontinuation of Valproate8 After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone7 Current dose of Lamotrigine (mg/day) 100Current dose of Lamotrigine (mg/day) 400
Week 1 Maintain current dose of Lamotrigine 150 400 Week 2 Maintain current dose of Lamotrigine 200 300 Week 3 onward Maintain current dose of Lamotrigine 200 200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with Lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with Lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
1 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine 2 These drugs induce Lamotrigine glucuronidation and increase clearance 3 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine 4 These drugs induce Lamotrigine glucuronidation and increase clearance 5 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine 6 These drugs induce Lamotrigine glucuronidation and increase clearance 7 These drugs induce Lamotrigine glucuronidation and increase clearance 8 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine -
Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ] Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Rash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablets is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets may require adjustment based on clinical response.
Target Plasma Levels for Patients with Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives:(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.
Patients with Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients with Renal Impairment: Initial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine tablets in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
This section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy
For Patients TAKING Valproate a For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidoneb, or Valproatea For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day
(in 2 divided doses) Weeks 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks. Usual maintenance dose 100 to 200 mg/day with valproate alone 100 to 400 mg/day with valproate and other drugs that induceglucuronication
(in 1 or 2 divided doses) 225 to 375 mg/day
(in 2 divided doses) 300 to 500 mg/day
(in 2 divided doses)a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce glucuronidation and increase clearance [see Drug Interactions (7) Clinical Pharmacology (12.3)]. Other drugs, that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7),Clinical Pharmacology (12.3)].
Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect..
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2. Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy
For Patients TAKING Valproatea For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidoneb, or Valproatea For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea Weeks 1 and 2 0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide) 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide) 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual maintenance dose 1 to 5 mg/kg/day
(maximum 200 mg/day in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day
(maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as such much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical responseNote: Only whole tablets should be used for dosing.
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce glucuronidation and increase clearance [see Drug Interactions (7)Clinical Pharmacology (12.3)]. Other drugs, that have similar effects include estrogen-containing oral contraceptives and rifampin [see Drug Interactions (7),Clinical Pharmacology Pharmacokinetics (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect..
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy
If the patient’s weight is Give this daily dose, using the most appropriate combination of lamotrigine 2 mg and 5 mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
The goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion from Adjunctive Therapy with Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy with Lamotrigine: After achieving a dose of 500 mg/day of lamotrigine tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy with Valproate to Monotherapy with Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age with Epilepsy
Lamotrigine Valproate Step 1 Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day). Maintain previous stable dose. Step 2 Maintain at 200 mg/day. Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week. Step 3 Increase to 300 mg/day and maintain for 1 week. Simultaneously decrease to 250 mg/day and maintain for 1 week. Step 4 Increase by 100 mg/day every week to achieve maintenance dose of
500 mg/day. Discontinue.Conversion from Adjunctive Therapy with Antiepileptic Drugs other than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy with Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
The goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients with Bipolar Disorder
For Patients TAKING Valproatea For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidoneb, Valproatea For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb, and NOT TAKING Valproatea Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided dosesa Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 6. Dosage Adjustments to Lamotrigine for Patients with Bipolar Disorder Following Discontinuation of Psychotropic Medications
Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidoneb, or Valproatea) After Discontinuation of Valproatea After Discontinuation of Valproatea Current dose of lamotrigine (mg/day) 100 Current dose of lamotrigine (mg/day) 400 Week 1 Maintain current dose of lamotrigine 150 400 Week 2 Maintain current dose of lamotrigine 200 300 Week 3 onward Maintain current dose of lamotrigine 200 200a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine tablets was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ] Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Dosing is based on concomitant medications, indication, and patient age. (2.2, 2.4) To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations should not be exceeded. (2.1, 16) Do not restart Lamotrigine in patients who discontinued due to rash unless the potential benefits clearly outweigh the risks. (2.1) Adjustments to maintenance doses will in most cases be required in patients starting or stopping estrogen-containing oral contraceptives. (2.1, 5.8) Lamotrigine should be discontinued over a period of at least 2 weeks (approximately 50% reduction per week). (2.1, 5.9)Epilepsy
Adjunctive therapy—See Table 1 for patients >12 years of age and Tables 2 and 3 for patients 2 to 12 years. (2.2) Conversion to monotherapy—See Table 4. (2.3)Bipolar Disorder: See Tables 5 and 6 (2.4)
Rash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of Lamotrigine with valproate, (2) exceeding the recommended initial dose of Lamotrigine, or (3) exceeding the recommended dose escalation for Lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of Lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that Lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with Lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued Lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued Lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of Lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with Lamotrigine. Because Lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of Lamotrigine and doses of Lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for Lamotrigine. Dosing of Lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of Lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for Lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with Lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of Lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of Lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent Lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of Lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent Lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless Lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in Lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased Lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to Lamotrigine consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of Lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of Lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent Lamotrigine plasma level. The decrease in dose of Lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or Lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of Lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of Lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of Lamotrigine up to 2-fold, and the progestin-only pills had no effect on Lamotrigine plasma levels. Therefore, adjustments to the dosage of Lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of Lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with Lamotrigine. Because there is inadequate experience in this population, Lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving Lamotrigine in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse experiences is observed.
If a decision is made to discontinue therapy with Lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation should prolong the half-life of Lamotrigine; discontinuing valproate should shorten the half-life of Lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of Lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of Lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of Lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
This section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†,or Valproate1 For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone2 and NOT TAKING Valproate1 Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day (in 2 divided doses) Weeks 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day
every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks Usual Maintenance Dose 100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronication
(in 1 or 2 divided doses) 225 to 375 mg/day
(in 2 divided doses) 300 to 500 mg/day (in 2 divided doses)
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine,
Phenytoin,
Phenobarbital,
Primidone† or
Valproate3 For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone4 and NOT TAKING Valproate3 Weeks 1 and 2 0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual Maintenance Dose 1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day
(maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response Note: Only whole tablets should be used for dosing.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of Lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive Lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive Lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
The goal of the transition regimen is to effect the conversion to monotherapy with Lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of Lamotrigine.
The recommended maintenance dose of Lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of Lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age with EpilepsyLamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with Lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.The goal of maintenance treatment with Lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of Lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of Lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin, that increase the apparent clearance of Lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with Lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of Lamotrigine should be adjusted. For patients discontinuing valproate, the dose of Lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation, the dose of Lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of Lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of Lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of Lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate5 For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone6 and NOT TAKING Valproate5 Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses
Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic MedicationsDiscontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone*, or Valproate†)
After Discontinuation of Valproate8 After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone7 Current dose of Lamotrigine (mg/day) 100Current dose of Lamotrigine (mg/day) 400
Week 1 Maintain current dose of Lamotrigine 150 400 Week 2 Maintain current dose of Lamotrigine 200 300 Week 3 onward Maintain current dose of Lamotrigine 200 200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with Lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with Lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
1 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine 2 These drugs induce Lamotrigine glucuronidation and increase clearance 3 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine 4 These drugs induce Lamotrigine glucuronidation and increase clearance 5 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine 6 These drugs induce Lamotrigine glucuronidation and increase clearance 7 These drugs induce Lamotrigine glucuronidation and increase clearance 8 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine -
Avkare, Inc.
-
Remedyrepack Inc.
![Lamotrigine (Lamotrigine ) Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Remedyrepack Inc.
![Lamotrigine (Lamotrigine ) Tablet [Remedyrepack Inc. ] Lamotrigine (Lamotrigine ) Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Dosing is based on concomitant medications, indication, and patient age. (2.2, 2.4) To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations should not be exceeded. Lamotrigine Starter Kits are available for the first 5 weeks of treatment. (2.1, 16) Do not restart lamotrigine tablets, USP in patients who discontinued due to rash unless the potential benefits clearly outweigh the risks. (2.1) Adjustments to maintenance doses will in most cases be required in patients starting or stopping estrogen-containing oral contraceptives. (2.1, 5.9) Lamotrigine tablets, USP should be discontinued over a period of at least 2 weeks (approximately 50% reduction per week). (2.1, 5.10)Epilepsy
Adjunctive therapy—See Table 1 for patients >12 years of age and Tables 2 and 3 for patients 2 to 12 years. (2.2) Conversion to monotherapy—See Table 4. (2.3)Bipolar Disorder: See Tables 5 and 6. (2.4)
Rash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
Lamotrigine Starter Kits provide lamotrigine at doses consistent with the recommended titration schedule for the first 5 weeks of treatment, based upon concomitant medications for patients with epilepsy (>12 years of age) and Bipolar I Disorder (≥18 years of age) and are intended to help reduce the potential for rash. The use of lamotrigine Starter Kits is recommended for appropriate patients who are starting or restarting lamotrigine [see How Supplied/Storage and Handling (16)].
It is recommended that lamotrigine tablets, USP not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.10)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.10)].
This section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy
For Patients TAKING
Valproatea
For Patients NOT
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital,
Primidoneb, or
Valproatea
For Patients
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidoneb and
NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Week 5
onwards to
maintenance
Increase by 25 to 50
mg/day every 1 to
2 weeks
Increase by 50
mg/day every 1 to
2 weeks
Increase by 100
mg/day every 1 to
2 weeks.
Usual
Maintenance
Dose
100 to 200 mg/day
with valproate
alone
100 to 400 mg/day
with valproate and
other drugs that
induce
glucuronidation
(in 1 or 2 divided
doses)
225 to 375 mg/day
(in 2 divided doses)
300 to 500 mg/day
(in 2 divided doses)
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
The smallest available strength of lamotrigine tablets is 25 mg, and only whole tablets should be administered. If the calculated dose cannot be achieved using whole tablets, the dose should be rounded down to the nearest whole tablet [see How Supplied/Storage and Handling (16) and Medication Guide].
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy
For Patients
TAKING Valproatea
For Patients NOT
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital,
Primidoneb, or
Valproatea
For Patients TAKING
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidoneb and NOT
TAKING Valproatea
Weeks 1
and 2
0.15 mg/kg/day
in 1 or 2 divided
doses, rounded
down to the nearest
whole tablet (see
Table 3 for weight
based dosing guide)
0.3 mg/kg/day
in 1 or 2 divided
doses, rounded down
to the nearest whole
tablet
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
Weeks 3
and 4
0.3 mg/kg/day
in 1 or 2 divided
doses, rounded
down to the nearest
whole tablet (see
Table 3 for weight
based dosing guide)
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
1.2 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
Week 5
onwards to
maintenance
The dose should be
increased every 1 to
2 weeks as follows:
calculate 0.3 mg/kg/day,
round this amount
down to the nearest
whole tablet, and
add this amount to
the previously
administered daily
dose
The dose should be increased every 1 to
2 weeks as follows: calculate
0.6 mg/kg/day, round
this amount down to
the nearest whole
tablet, and add this
amount to the
previously
administered daily
dose
The dose should be increased every 1 to
2 weeks as follows: calculate
1.2 mg/kg/day, round
this amount down to
the nearest whole
tablet, and add this
amount to the
previously
administered daily
dose
Usual
Maintenance
Dose
1 to 5 mg/kg/day
(maximum
200 mg/day in 1 or 2
divided doses).
1 to 3 mg/kg/day
with valproate alone
4.5 to 7.5 mg/kg/day
(maximum 300
mg/day in 2 divided
doses)
5 to 15 mg/kg/day
(maximum 400
mg/day in 2 divided
doses)
Maintenance
dose in
patients less
than 30 kg
May need to be
increased by as
much as 50%, based
on clinical response
May need to be
increased by as much
as 50%, based on
clinical response
May need to be
increased by as much
as 50%, based on
clinical response
Note: Only whole tablets should be used for dosing.
aValproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7),
Clinical Pharmacology (12.3)].bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)].
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is
Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see
Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Give this daily dose, using the most appropriate combination of lamotrigine
2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
The goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age With Epilepsy
Lamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to
guidelines in Table 1 (if not already on
200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by
decrements no greater than
500 mg/day/week and then
maintain the dose of
500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1
week.
Simultaneously decrease to
250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve
maintenance dose of 500 mg/day.
Discontinue.
Conversion From Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
The goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder
For Patients TAKING Valproatea
For Patients NOT TAKING
Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea
For Patients TAKING
Carbamazepine, Phenytoin, Phenobarbital,
or Primidoneb and
NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in
divided doses
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications
Discontinuation of Psychotropic Drugs
(excluding Carbamazepine, Phenytoin,
After Discontinuation of Valproatea
After Discontinuation of Carbamazepine,
Phenytoin, Phenobarbital,or
Primidoneb
Phenobarbital, Primidoneb, or Valproatea)
Current dose of Lamotrigine (mg/day)
100
Current dose of Lamotrigine (mg/day)
400
Week 1
Maintain current dose of Lamotrigine
150
400
Week 2
Maintain current dose of Lamotrigine
200
300
Week 3 onward
Maintain current dose of Lamotrigine
200
200
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ] Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Dosing is based on concomitant medications, indication, and patient age. (2.2, 2.4) To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations should not be exceeded. (2.1) Do not restart lamotrigine tablets in patients who discontinued due to rash unless the potential benefits clearly outweigh the risks. (2.1) Adjustments to maintenance doses will in most cases be required in patients starting or stopping estrogen-containing oral contraceptives. (2.1, 5.8) Lamotrigine tablets should be discontinued over a period of at least 2 weeks (approximately 50% reduction per week). (2.1, 5.9)Epilepsy
Adjunctive therapy—See Table 1 for patients > 12 years of age and Tables 2and 3 for patients 2 to 12 years. (2.2) Conversion to monotherapy—See Table 4. (2.3)Bipolar Disorder: See Tables 5 and6. (2.4)
Rash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablets is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be increased, by as much as 2 fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2 fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (seeTable 1 orTable 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2 week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2 fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1to3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine tablets in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
This section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,† or Valproate1 For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone2 and NOT TAKING Valproate1 Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day (in 2 divided doses) Week 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks Usual Maintenance Dose100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses)
225 to 375 mg/day (in 2 divided doses)300 to 500 mg/day
(in 2 divided doses)
1
2
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,† or Valproate3 For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone4 and NOT TAKING Valproate3 Weeks 1 and 2 0.15 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3for weight based dosing guide) 0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet Week 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual Maintenance Dose 1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses)
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day (maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical responseNote: Only whole tablets should be used for dosing.
3
4
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years of Age Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of lamotrigine tablets, 2 mg and 5 mg Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
The goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets: After achieving a dose of 500 mg/day of lamotrigine tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4 week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥ 16 Years of Age With Epilepsy Lamotrigine Valproate Step 1 Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day). Maintain previous stable dose. Step 2 Maintain at 200 mg/day. Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week. Step 3 Increase to 300 mg/day and maintain for 1 week. Simultaneously decrease to 250 mg/day and maintain for 1 week. Step 4 Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day. Discontinue.Conversion From Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
The goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2 week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2 week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,† or Valproate5 For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone6 and NOT TAKING Valproate5 Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses
5
6
Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone,* or Valproate†) After Discontinuation of Valproate8 After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone7 Current dose of Lamotrigine (mg/day) 100Current dose of Lamotrigine (mg/day)
400
Week 1 Maintain current dose of lamotrigine 150 400 Week 2 Maintain current dose of lamotrigine 200 300 Week 3 onward Maintain current dose of lamotrigine 200 200
7
8
The benefit of continuing treatment in patients who had been stabilized in an 8 to 16 week open-label phase with lamotrigine tablets was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
1 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ 2 These drugs induce lamotrigine glucuronidation and increase clearance [ 3 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ 4 These drugs induce lamotrigine glucuronidation and increase clearance [ 5 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ 6 These drugs induce lamotrigine glucuronidation and increase clearance [ 7 These drugs induce lamotrigine glucuronidation and increase clearance [ 8 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ -
Remedyrepack Inc.
![Lamotrigine (Lamotrigine ) Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Remedyrepack Inc.
![Lamotrigine (Lamotrigine ) Tablet [Remedyrepack Inc. ] Lamotrigine (Lamotrigine ) Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Dosing is based on concomitant medications, indication, and patient age. (2.2, 2.4) To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations should not be exceeded. Lamotrigine Starter Kits are available for the first 5 weeks of treatment. (2.1, 16) Do not restart lamotrigine tablets, USP in patients who discontinued due to rash unless the potential benefits clearly outweigh the risks. (2.1) Adjustments to maintenance doses will in most cases be required in patients starting or stopping estrogen-containing oral contraceptives. (2.1, 5.9) Lamotrigine tablets, USP should be discontinued over a period of at least 2 weeks (approximately 50% reduction per week). (2.1, 5.10)Epilepsy
Adjunctive therapy—See Table 1 for patients >12 years of age and Tables 2 and 3 for patients 2 to 12 years. (2.2) Conversion to monotherapy—See Table 4. (2.3)Bipolar Disorder: See Tables 5 and 6. (2.4)
Rash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
Lamotrigine Starter Kits provide lamotrigine at doses consistent with the recommended titration schedule for the first 5 weeks of treatment, based upon concomitant medications for patients with epilepsy (>12 years of age) and Bipolar I Disorder (≥18 years of age) and are intended to help reduce the potential for rash. The use of lamotrigine Starter Kits is recommended for appropriate patients who are starting or restarting lamotrigine [see How Supplied/Storage and Handling (16)].
It is recommended that lamotrigine tablets, USP not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.10)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.10)].
This section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy
For Patients TAKING
Valproatea
For Patients NOT
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital,
Primidoneb, or
Valproatea
For Patients
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidoneb and
NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Week 5
onwards to
maintenance
Increase by 25 to 50
mg/day every 1 to
2 weeks
Increase by 50
mg/day every 1 to
2 weeks
Increase by 100
mg/day every 1 to
2 weeks.
Usual
Maintenance
Dose
100 to 200 mg/day
with valproate
alone
100 to 400 mg/day
with valproate and
other drugs that
induce
glucuronidation
(in 1 or 2 divided
doses)
225 to 375 mg/day
(in 2 divided doses)
300 to 500 mg/day
(in 2 divided doses)
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
The smallest available strength of lamotrigine tablets is 25 mg, and only whole tablets should be administered. If the calculated dose cannot be achieved using whole tablets, the dose should be rounded down to the nearest whole tablet [see How Supplied/Storage and Handling (16) and Medication Guide].
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy
For Patients
TAKING Valproatea
For Patients NOT
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital,
Primidoneb, or
Valproatea
For Patients TAKING
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidoneb and NOT
TAKING Valproatea
Weeks 1
and 2
0.15 mg/kg/day
in 1 or 2 divided
doses, rounded
down to the nearest
whole tablet (see
Table 3 for weight
based dosing guide)
0.3 mg/kg/day
in 1 or 2 divided
doses, rounded down
to the nearest whole
tablet
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
Weeks 3
and 4
0.3 mg/kg/day
in 1 or 2 divided
doses, rounded
down to the nearest
whole tablet (see
Table 3 for weight
based dosing guide)
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
1.2 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
Week 5
onwards to
maintenance
The dose should be
increased every 1 to
2 weeks as follows:
calculate 0.3 mg/kg/day,
round this amount
down to the nearest
whole tablet, and
add this amount to
the previously
administered daily
dose
The dose should be increased every 1 to
2 weeks as follows: calculate
0.6 mg/kg/day, round
this amount down to
the nearest whole
tablet, and add this
amount to the
previously
administered daily
dose
The dose should be increased every 1 to
2 weeks as follows: calculate
1.2 mg/kg/day, round
this amount down to
the nearest whole
tablet, and add this
amount to the
previously
administered daily
dose
Usual
Maintenance
Dose
1 to 5 mg/kg/day
(maximum
200 mg/day in 1 or 2
divided doses).
1 to 3 mg/kg/day
with valproate alone
4.5 to 7.5 mg/kg/day
(maximum 300
mg/day in 2 divided
doses)
5 to 15 mg/kg/day
(maximum 400
mg/day in 2 divided
doses)
Maintenance
dose in
patients less
than 30 kg
May need to be
increased by as
much as 50%, based
on clinical response
May need to be
increased by as much
as 50%, based on
clinical response
May need to be
increased by as much
as 50%, based on
clinical response
Note: Only whole tablets should be used for dosing.
aValproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7),
Clinical Pharmacology (12.3)].bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)].
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is
Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see
Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Give this daily dose, using the most appropriate combination of lamotrigine
2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
The goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age With Epilepsy
Lamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to
guidelines in Table 1 (if not already on
200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by
decrements no greater than
500 mg/day/week and then
maintain the dose of
500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1
week.
Simultaneously decrease to
250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve
maintenance dose of 500 mg/day.
Discontinue.
Conversion From Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
The goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder
For Patients TAKING Valproatea
For Patients NOT TAKING
Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea
For Patients TAKING
Carbamazepine, Phenytoin, Phenobarbital,
or Primidoneb and
NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in
divided doses
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications
Discontinuation of Psychotropic Drugs
(excluding Carbamazepine, Phenytoin,
After Discontinuation of Valproatea
After Discontinuation of Carbamazepine,
Phenytoin, Phenobarbital,or
Primidoneb
Phenobarbital, Primidoneb, or Valproatea)
Current dose of Lamotrigine (mg/day)
100
Current dose of Lamotrigine (mg/day)
400
Week 1
Maintain current dose of Lamotrigine
150
400
Week 2
Maintain current dose of Lamotrigine
200
300
Week 3 onward
Maintain current dose of Lamotrigine
200
200
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Glenmark Generics Inc., Usa
![Lamotrigine Tablet [Glenmark Generics Inc., Usa]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | G&w Laboratories, Inc.
![Lamotrigine Tablet [Glenmark Generics Inc., Usa] Lamotrigine Tablet [Glenmark Generics Inc., Usa]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Topical corticosteroids are generally applied to the affected area as a thin film from two to four times daily depending on the severity of the condition. In hairy sites, the hair should be parted to allow direct contact with the lesion.
Occlusive dressings may be used for the management of psoriasis or recalcitrant conditions. Some plastic films may be flammable and due care should be exercised in their use. Similarly, caution should be employed when such films are used on children or left in their proximity, to avoid the possibility of accidental suffocation.
If an infection develops, the use of occlusive dressings should be discontinued and appropriate antimicrobial therapy instituted. -
Remedyrepack Inc.
![Lamotrigine (Lamotrigine ) Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Remedyrepack Inc.
![Lamotrigine (Lamotrigine ) Tablet [Remedyrepack Inc. ] Lamotrigine (Lamotrigine ) Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Dosing is based on concomitant medications, indication, and patient age. (2.2, 2.4) To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations should not be exceeded. Lamotrigine Starter Kits are available for the first 5 weeks of treatment. (2.1, 16) Do not restart lamotrigine tablets, USP in patients who discontinued due to rash unless the potential benefits clearly outweigh the risks. (2.1) Adjustments to maintenance doses will in most cases be required in patients starting or stopping estrogen-containing oral contraceptives. (2.1, 5.9) Lamotrigine tablets, USP should be discontinued over a period of at least 2 weeks (approximately 50% reduction per week). (2.1, 5.10)Epilepsy
Adjunctive therapy—See Table 1 for patients >12 years of age and Tables 2 and 3 for patients 2 to 12 years. (2.2) Conversion to monotherapy—See Table 4. (2.3)Bipolar Disorder: See Tables 5 and 6. (2.4)
Rash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
Lamotrigine Starter Kits provide lamotrigine at doses consistent with the recommended titration schedule for the first 5 weeks of treatment, based upon concomitant medications for patients with epilepsy (>12 years of age) and Bipolar I Disorder (≥18 years of age) and are intended to help reduce the potential for rash. The use of lamotrigine Starter Kits is recommended for appropriate patients who are starting or restarting lamotrigine [see How Supplied/Storage and Handling (16)].
It is recommended that lamotrigine tablets, USP not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.10)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.10)].
This section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy
For Patients TAKING
Valproatea
For Patients NOT
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital,
Primidoneb, or
Valproatea
For Patients
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidoneb and
NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Week 5
onwards to
maintenance
Increase by 25 to 50
mg/day every 1 to
2 weeks
Increase by 50
mg/day every 1 to
2 weeks
Increase by 100
mg/day every 1 to
2 weeks.
Usual
Maintenance
Dose
100 to 200 mg/day
with valproate
alone
100 to 400 mg/day
with valproate and
other drugs that
induce
glucuronidation
(in 1 or 2 divided
doses)
225 to 375 mg/day
(in 2 divided doses)
300 to 500 mg/day
(in 2 divided doses)
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
The smallest available strength of lamotrigine tablets is 25 mg, and only whole tablets should be administered. If the calculated dose cannot be achieved using whole tablets, the dose should be rounded down to the nearest whole tablet [see How Supplied/Storage and Handling (16) and Medication Guide].
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy
For Patients
TAKING Valproatea
For Patients NOT
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital,
Primidoneb, or
Valproatea
For Patients TAKING
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidoneb and NOT
TAKING Valproatea
Weeks 1
and 2
0.15 mg/kg/day
in 1 or 2 divided
doses, rounded
down to the nearest
whole tablet (see
Table 3 for weight
based dosing guide)
0.3 mg/kg/day
in 1 or 2 divided
doses, rounded down
to the nearest whole
tablet
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
Weeks 3
and 4
0.3 mg/kg/day
in 1 or 2 divided
doses, rounded
down to the nearest
whole tablet (see
Table 3 for weight
based dosing guide)
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
1.2 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
Week 5
onwards to
maintenance
The dose should be
increased every 1 to
2 weeks as follows:
calculate 0.3 mg/kg/day,
round this amount
down to the nearest
whole tablet, and
add this amount to
the previously
administered daily
dose
The dose should be increased every 1 to
2 weeks as follows: calculate
0.6 mg/kg/day, round
this amount down to
the nearest whole
tablet, and add this
amount to the
previously
administered daily
dose
The dose should be increased every 1 to
2 weeks as follows: calculate
1.2 mg/kg/day, round
this amount down to
the nearest whole
tablet, and add this
amount to the
previously
administered daily
dose
Usual
Maintenance
Dose
1 to 5 mg/kg/day
(maximum
200 mg/day in 1 or 2
divided doses).
1 to 3 mg/kg/day
with valproate alone
4.5 to 7.5 mg/kg/day
(maximum 300
mg/day in 2 divided
doses)
5 to 15 mg/kg/day
(maximum 400
mg/day in 2 divided
doses)
Maintenance
dose in
patients less
than 30 kg
May need to be
increased by as
much as 50%, based
on clinical response
May need to be
increased by as much
as 50%, based on
clinical response
May need to be
increased by as much
as 50%, based on
clinical response
Note: Only whole tablets should be used for dosing.
aValproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7),
Clinical Pharmacology (12.3)].bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)].
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is
Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see
Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Give this daily dose, using the most appropriate combination of lamotrigine
2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
The goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age With Epilepsy
Lamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to
guidelines in Table 1 (if not already on
200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by
decrements no greater than
500 mg/day/week and then
maintain the dose of
500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1
week.
Simultaneously decrease to
250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve
maintenance dose of 500 mg/day.
Discontinue.
Conversion From Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
The goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder
For Patients TAKING Valproatea
For Patients NOT TAKING
Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea
For Patients TAKING
Carbamazepine, Phenytoin, Phenobarbital,
or Primidoneb and
NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in
divided doses
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications
Discontinuation of Psychotropic Drugs
(excluding Carbamazepine, Phenytoin,
After Discontinuation of Valproatea
After Discontinuation of Carbamazepine,
Phenytoin, Phenobarbital,or
Primidoneb
Phenobarbital, Primidoneb, or Valproatea)
Current dose of Lamotrigine (mg/day)
100
Current dose of Lamotrigine (mg/day)
400
Week 1
Maintain current dose of Lamotrigine
150
400
Week 2
Maintain current dose of Lamotrigine
200
300
Week 3 onward
Maintain current dose of Lamotrigine
200
200
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Remedyrepack Inc.
![Lamotrigine (Lamotrigine ) Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Remedyrepack Inc.
![Lamotrigine (Lamotrigine ) Tablet [Remedyrepack Inc. ] Lamotrigine (Lamotrigine ) Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Dosing is based on concomitant medications, indication, and patient age. (2.2, 2.4) To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations should not be exceeded. Lamotrigine Starter Kits are available for the first 5 weeks of treatment. (2.1, 16) Do not restart lamotrigine tablets, USP in patients who discontinued due to rash unless the potential benefits clearly outweigh the risks. (2.1) Adjustments to maintenance doses will in most cases be required in patients starting or stopping estrogen-containing oral contraceptives. (2.1, 5.9) Lamotrigine tablets, USP should be discontinued over a period of at least 2 weeks (approximately 50% reduction per week). (2.1, 5.10)Epilepsy
Adjunctive therapy—See Table 1 for patients >12 years of age and Tables 2 and 3 for patients 2 to 12 years. (2.2) Conversion to monotherapy—See Table 4. (2.3)Bipolar Disorder: See Tables 5 and 6. (2.4)
Rash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
Lamotrigine Starter Kits provide lamotrigine at doses consistent with the recommended titration schedule for the first 5 weeks of treatment, based upon concomitant medications for patients with epilepsy (>12 years of age) and Bipolar I Disorder (≥18 years of age) and are intended to help reduce the potential for rash. The use of lamotrigine Starter Kits is recommended for appropriate patients who are starting or restarting lamotrigine [see How Supplied/Storage and Handling (16)].
It is recommended that lamotrigine tablets, USP not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.10)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.10)].
This section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy
For Patients TAKING
Valproatea
For Patients NOT
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital,
Primidoneb, or
Valproatea
For Patients
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidoneb and
NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Week 5
onwards to
maintenance
Increase by 25 to 50
mg/day every 1 to
2 weeks
Increase by 50
mg/day every 1 to
2 weeks
Increase by 100
mg/day every 1 to
2 weeks.
Usual
Maintenance
Dose
100 to 200 mg/day
with valproate
alone
100 to 400 mg/day
with valproate and
other drugs that
induce
glucuronidation
(in 1 or 2 divided
doses)
225 to 375 mg/day
(in 2 divided doses)
300 to 500 mg/day
(in 2 divided doses)
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
The smallest available strength of lamotrigine tablets is 25 mg, and only whole tablets should be administered. If the calculated dose cannot be achieved using whole tablets, the dose should be rounded down to the nearest whole tablet [see How Supplied/Storage and Handling (16) and Medication Guide].
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy
For Patients
TAKING Valproatea
For Patients NOT
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital,
Primidoneb, or
Valproatea
For Patients TAKING
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidoneb and NOT
TAKING Valproatea
Weeks 1
and 2
0.15 mg/kg/day
in 1 or 2 divided
doses, rounded
down to the nearest
whole tablet (see
Table 3 for weight
based dosing guide)
0.3 mg/kg/day
in 1 or 2 divided
doses, rounded down
to the nearest whole
tablet
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
Weeks 3
and 4
0.3 mg/kg/day
in 1 or 2 divided
doses, rounded
down to the nearest
whole tablet (see
Table 3 for weight
based dosing guide)
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
1.2 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
Week 5
onwards to
maintenance
The dose should be
increased every 1 to
2 weeks as follows:
calculate 0.3 mg/kg/day,
round this amount
down to the nearest
whole tablet, and
add this amount to
the previously
administered daily
dose
The dose should be increased every 1 to
2 weeks as follows: calculate
0.6 mg/kg/day, round
this amount down to
the nearest whole
tablet, and add this
amount to the
previously
administered daily
dose
The dose should be increased every 1 to
2 weeks as follows: calculate
1.2 mg/kg/day, round
this amount down to
the nearest whole
tablet, and add this
amount to the
previously
administered daily
dose
Usual
Maintenance
Dose
1 to 5 mg/kg/day
(maximum
200 mg/day in 1 or 2
divided doses).
1 to 3 mg/kg/day
with valproate alone
4.5 to 7.5 mg/kg/day
(maximum 300
mg/day in 2 divided
doses)
5 to 15 mg/kg/day
(maximum 400
mg/day in 2 divided
doses)
Maintenance
dose in
patients less
than 30 kg
May need to be
increased by as
much as 50%, based
on clinical response
May need to be
increased by as much
as 50%, based on
clinical response
May need to be
increased by as much
as 50%, based on
clinical response
Note: Only whole tablets should be used for dosing.
aValproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7),
Clinical Pharmacology (12.3)].bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)].
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is
Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see
Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Give this daily dose, using the most appropriate combination of lamotrigine
2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
The goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age With Epilepsy
Lamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to
guidelines in Table 1 (if not already on
200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by
decrements no greater than
500 mg/day/week and then
maintain the dose of
500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1
week.
Simultaneously decrease to
250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve
maintenance dose of 500 mg/day.
Discontinue.
Conversion From Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
The goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder
For Patients TAKING Valproatea
For Patients NOT TAKING
Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea
For Patients TAKING
Carbamazepine, Phenytoin, Phenobarbital,
or Primidoneb and
NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in
divided doses
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications
Discontinuation of Psychotropic Drugs
(excluding Carbamazepine, Phenytoin,
After Discontinuation of Valproatea
After Discontinuation of Carbamazepine,
Phenytoin, Phenobarbital,or
Primidoneb
Phenobarbital, Primidoneb, or Valproatea)
Current dose of Lamotrigine (mg/day)
100
Current dose of Lamotrigine (mg/day)
400
Week 1
Maintain current dose of Lamotrigine
150
400
Week 2
Maintain current dose of Lamotrigine
200
300
Week 3 onward
Maintain current dose of Lamotrigine
200
200
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ] Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Dosing is based on concomitant medications, indication, and patient age. (2.2, 2.4) To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations should not be exceeded. (2.1, 16) Do not restart Lamotrigine in patients who discontinued due to rash unless the potential benefits clearly outweigh the risks. (2.1) Adjustments to maintenance doses will in most cases be required in patients starting or stopping estrogen-containing oral contraceptives. (2.1, 5.8) Lamotrigine should be discontinued over a period of at least 2 weeks (approximately 50% reduction per week). (2.1, 5.9)Epilepsy
Adjunctive therapy—See Table 1 for patients >12 years of age and Tables 2 and 3 for patients 2 to 12 years. (2.2) Conversion to monotherapy—See Table 4. (2.3)Bipolar Disorder: See Tables 5 and 6 (2.4)
Rash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of Lamotrigine with valproate, (2) exceeding the recommended initial dose of Lamotrigine, or (3) exceeding the recommended dose escalation for Lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of Lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that Lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with Lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued Lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued Lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of Lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with Lamotrigine. Because Lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of Lamotrigine and doses of Lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for Lamotrigine. Dosing of Lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of Lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for Lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with Lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of Lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of Lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent Lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of Lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent Lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless Lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in Lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased Lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to Lamotrigine consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of Lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of Lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent Lamotrigine plasma level. The decrease in dose of Lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or Lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of Lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of Lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of Lamotrigine up to 2-fold, and the progestin-only pills had no effect on Lamotrigine plasma levels. Therefore, adjustments to the dosage of Lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of Lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with Lamotrigine. Because there is inadequate experience in this population, Lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving Lamotrigine in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse experiences is observed.
If a decision is made to discontinue therapy with Lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation should prolong the half-life of Lamotrigine; discontinuing valproate should shorten the half-life of Lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of Lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of Lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of Lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
This section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†,or Valproate1 For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone2 and NOT TAKING Valproate1 Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day (in 2 divided doses) Weeks 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day
every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks Usual Maintenance Dose 100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronication
(in 1 or 2 divided doses) 225 to 375 mg/day
(in 2 divided doses) 300 to 500 mg/day (in 2 divided doses)
1
2
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine,
Phenytoin,
Phenobarbital,
Primidone† or
Valproate3 For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone4 and NOT TAKING Valproate3 Weeks 1 and 2 0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual Maintenance Dose 1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day
(maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response Note: Only whole tablets should be used for dosing.
3
4
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of Lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive Lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive Lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
The goal of the transition regimen is to effect the conversion to monotherapy with Lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of Lamotrigine.
The recommended maintenance dose of Lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of Lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age with EpilepsyLamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with Lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.The goal of maintenance treatment with Lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of Lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of Lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin, that increase the apparent clearance of Lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with Lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of Lamotrigine should be adjusted. For patients discontinuing valproate, the dose of Lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation, the dose of Lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of Lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of Lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of Lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate5 For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone6 and NOT TAKING Valproate5 Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses
5
6
Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic MedicationsDiscontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone*, or Valproate†)
After Discontinuation of Valproate8 After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone7 Current dose of Lamotrigine (mg/day) 100Current dose of Lamotrigine (mg/day) 400
Week 1 Maintain current dose of Lamotrigine 150 400 Week 2 Maintain current dose of Lamotrigine 200 300 Week 3 onward Maintain current dose of Lamotrigine 200 200
7
8
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with Lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with Lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
1 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine 2 These drugs induce Lamotrigine glucuronidation and increase clearance 3 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine 4 These drugs induce Lamotrigine glucuronidation and increase clearance 5 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine 6 These drugs induce Lamotrigine glucuronidation and increase clearance 7 These drugs induce Lamotrigine glucuronidation and increase clearance 8 Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine -
Mckesson Contract Packaging
![Lamotrigine Tablet [Mckesson Contract Packaging]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Mckesson Contract Packaging
![Lamotrigine Tablet [Mckesson Contract Packaging] Lamotrigine Tablet [Mckesson Contract Packaging]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning ]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablets is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be increased, by as much as 2 fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2 fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (seeTable 1 orTable 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2 week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2 fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1to3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine tablets in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ see Drug Interactions (7), Clinical Pharmacology (12.3)] . † These drugs induce lamotrigine glucuronidation and increase clearance [ see Drug Interactions (7) Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [ see Drug Interactions (7), Clinical Pharmacology (12.3)] . Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [ see Dosage and Administration (2.1)] . Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,† or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day (in 2 divided doses) Week 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks Usual Maintenance Dose100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses)
225 to 375 mg/day (in 2 divided doses)300 to 500 mg/day
(in 2 divided doses)
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ see Drug Interactions (7), Clinical Pharmacology (12.3)] . † These drugs induce lamotrigine glucuronidation and increase clearance [ see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [ see Drug Interactions (7), Clinical Pharmacology (12.3)] . Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [ see Dosage and Administration (2.1)] . Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,† or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Weeks 1 and 2 0.15 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3for weight based dosing guide) 0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet Week 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual Maintenance Dose 1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day (maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical responseNote: Only whole tablets should be used for dosing.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of lamotrigine tablets, 2 mg and 5 mg Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning ].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets: After achieving a dose of 500 mg/day of lamotrigine tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4 week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥ 16 Years of Age With Epilepsy Lamotrigine Valproate Step 1 Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day). Maintain previous stable dose. Step 2 Maintain at 200 mg/day. Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week. Step 3 Increase to 300 mg/day and maintain for 1 week. Simultaneously decrease to 250 mg/day and maintain for 1 week. Step 4 Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day. Discontinue.Conversion From Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2 week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2 week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning ].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ see Drug Interactions (7), Clinical Pharmacology (12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [ see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [ see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [ see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,† or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications * These drugs induce lamotrigine glucuronidation and increase clearance [ see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [ see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [ see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. † Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ see Drug Interactions (7), Clinical Pharmacology (12.3)]. Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone,* or Valproate†) After Discontinuation of Valproate† After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone* Current dose of Lamotrigine (mg/day) 100Current dose of Lamotrigine (mg/day)
400
Week 1 Maintain current dose of lamotrigine 150 400 Week 2 Maintain current dose of lamotrigine 200 300 Week 3 onward Maintain current dose of lamotrigine 200 200The benefit of continuing treatment in patients who had been stabilized in an 8 to 16 week open-label phase with lamotrigine tablets was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Clinical Solutions Wholesale
![Lamotrigine Tablet [Clinical Solutions Wholesale]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Clinical Solutions Wholesale
![Lamotrigine Tablet [Clinical Solutions Wholesale] Lamotrigine Tablet [Clinical Solutions Wholesale]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
Lamotrigine Starter Kits provide lamotrigine at doses consistent with the recommended titration schedule for the first 5 weeks of treatment, based upon concomitant medications for patients with epilepsy (>12 years of age) and Bipolar I Disorder (≥18 years of age) and are intended to help reduce the potential for rash. The use of Lamotrigine Starter Kits is recommended for appropriate patients who are starting or restarting lamotrigine [see How Supplied/Storage and Handling (16)].
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy For Patients TAKING Valproate * For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day
(in 2 divided doses) Week 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks Usual maintenance dose 100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses) 225 to 375 mg/day
(in 2 divided doses) 300 to 500 mg/day
(in 2 divided doses)Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy For Patients TAKING Valproate * For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Note: Only whole tablets should be used for dosing. * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Weeks 1 and 2 0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Week 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual maintenance dose 1 to 5 mg/kg/day
(maximum 200 mg/day in 1 or 2 divided doses)
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day
(maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical responseDosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient's weight is Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age With Epilepsy Lamotrigine Valproate Step 1 Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day). Maintain previous stable dose. Step 2 Maintain at 200 mg/day. Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week. Step 3 Increase to 300 mg/day and maintain for 1 week. Simultaneously decrease to 250 mg/day and maintain for 1 week. Step 4 Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day. Discontinue.Conversion From Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone†, and NOT TAKING Valproate* * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone*, or Valproate†) After Discontinuation of Valproate† After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital or Primidone* Current dose of Lamotrigine (mg/day) 100 Current dose of Lamotrigine (mg/day) 400 * These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. † Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Week 1 Maintain current dose of Lamotrigine 150 400 Week 2 Maintain current dose of Lamotrigine 200 300 Week 3 onward Maintain current dose of Lamotrigine 200 200The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Ascend Laboratories, Llc
![Lamotrigine Tablet [Ascend Laboratories, Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Ascend Laboratories, Llc
![Lamotrigine Tablet [Ascend Laboratories, Llc] Lamotrigine Tablet [Ascend Laboratories, Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets, USP with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets, USP. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablets, USP are exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets, USP not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine tablets, USP Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets, USP may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets, USP should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives:Starting lamotrigine tablets, USP in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets, USP should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets, USP based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets, USP in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of lamotrigine tablets, USP In Women Taking Estrogen-Containing Oral Contraceptives:
(1)Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets, USP will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets, USP and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets, USP consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking lamotrigine tablets, USP in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets, USP should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets, USP will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets, USP should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine tablets, USP in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets, USP should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets, USP in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine tablets, USP should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets, USP. Because there is inadequate experience in this population, lamotrigine tablets, USP should be used with caution in these patients.
Discontinuation Strategy:Epilepsy: For patients receiving lamotrigine tablets, USP in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse experiences is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, USP, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets, USP. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets, USP. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets, USP should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine Tablets, USP in Patients Over 12 Years of Age With Epilepsy b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
For Patients TAKING Valproatea
For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidoneb, or Valproatea
For Patients TAKING
Carbamazepine, Phenytoin,
Phenobarbital, or Primidoneband NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Weeks 5 onwards
to maintenance
Increase by 25 to 50 mg/day every 1 to 2 weeks
Increase by 50 mg/day every 1 to 2 weeks
Increase by 100 mg/day every 1 to 2 weeks.
Usual
Maintenance Dose
100 to 200 mg/day with
valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
in 1 or 2 divided doses
225 to 375 mg/day
(in 2 divided doses)
300 to 500 mg/day
(in 2 divided doses)
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine Tablets, USP in Patients 2 to 12 Years of Age With Epilepsy a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen used with anticonvulsants that have this effect.
For Patients TAKING Valproatea
For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidoneb, or Valproatea
For Patients Taking Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea
Weeks 1 and 2
0.15 mg/kg/day
in 1 or 2 divided doses,
rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide)
0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet
0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet
Weeks 3 and 4
0.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide)
0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet
1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet
Weeks 5 onwards to maintenance
The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this
amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this
amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
Usual
Maintenance Dose
1 to 5 mg/kg/day
(maximum 200 mg/day in 1 or 2 divided doses).
1 to 3 mg/kg/day
with valproate alone
4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses)
5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses)
Maintenance
dose in
patients less
than 30 kg
May need to be increased
by as much as 50%, based
on clinical response
May need to be increased by as much as 50%, based on clinical response
May need to be increased by as much as 50%, based on clinical response
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is
Give this daily dose, using the most appropriate combination of lamotrigine 2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets, USP was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets, USP as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets, USP as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets, USP under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets, USP.
The recommended maintenance dose of lamotrigine tablets, USP as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets, USP should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets, USP: After achieving a dose of 500 mg/day of lamotrigine tablets, USP according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets, USP: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets, USP in Patients ≥16 Years of Age With Epilepsy
Lamotrigine Tablets, USP
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on
200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets, USP: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets, USP with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine tablets, USP are to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets, USP are 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets, USP are introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets, USP should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets, USP should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine tablets, USP should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets, USP may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets, USP may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets, USP [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets, USP should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine Tablets, USP for Patients With Bipolar Disorder a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
For Patients TAKING Valproatea
For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidoneb, or Valproatea
For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb, and NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 6. Dosage Adjustments to Lamotrigine Tablets, USP for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidoneb, or Valproatea)
After Discontinuation of Valproatea
After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb
Current dose of lamotrigine tablets, USP (mg/day)
100
Current dose of lamotrigine tablets, USP (mg/day)
400
Week 1
Maintain current dose of lamotrigine tablets, USP
150
400
Week 2
Maintain current dose of lamotrigine tablets, USP
200
300
Week 3 onward
Maintain current dose of lamotrigine tablets, USP
200
200
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)].Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine tablets, USP was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine tablets, USP has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Cobalt Laboratories
![Lamotrigine Tablet, Chewable [Cobalt Laboratories]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Cobalt Laboratories
![Lamotrigine Tablet, Chewable [Cobalt Laboratories] Lamotrigine Tablet, Chewable [Cobalt Laboratories]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash:There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets (chewable, dispersible) with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets (chewable, dispersible), or (3) exceeding the recommended dose escalation for lamotrigine tablets (chewable, dispersible). However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablets (chewable, dispersible) is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets (chewable, dispersible) not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Tablets (Chewable, Dispersible) Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets (chewable, dispersible) may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets (chewable, dispersible) should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives:Starting Lamotrigine Tablets (Chewable, Dispersible) in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets (chewable, dispersible) should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets (chewable, dispersible) based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets (chewable, dispersible) in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets (Chewable, Dispersible) in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives:For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets (chewable, dispersible) will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives:In women taking a stable dose of lamotrigine tablets (chewable, dispersible) and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets (chewable, dispersible) consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking lamotrigine tablets (chewable, dispersible) in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets (chewable, dispersible) should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives:For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7) , Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets (chewable, dispersible) will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets (chewable, dispersible) should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine tablets (chewable, dispersible) in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets (chewable, dispersible) should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets (chewable, dispersible) in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine tablets (chewable, dispersible) should be based on patients’ concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets (chewable, dispersible). Because there is inadequate experience in this population, lamotrigine tablets (chewable, dispersible) should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine tablets (chewable, dispersible) in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets (chewable, dispersible), a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets (chewable, dispersible). In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets (chewable, dispersible). However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets (chewable, dispersible) should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine Tablets (Chewable, Dispersible) in Patients Over 12 Years of Age With Epilepsy For Patients TAKING Valproatea For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,b or Valproatea For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day100 mg/day
(in 2 divided doses) Week 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks. Usual maintenance dose100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses)225 to 375 mg/day
(in 2 divided doses)300 to 500 mg/day
(in 2 divided doses)aValproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
The smallest available strength of lamotrigine tablets (chewable, dispersible) is 2 mg, and only whole tablets should be administered. If the calculated dose cannot be achieved using whole tablets, the dose should be rounded down to the nearest whole tablet [see How Supplied/Storage and Handling (16) and Medication Guide].
Table 2. Escalation Regimen for Lamotrigine Tablets (Chewable, Dispersible) in Patients 2 to 12 Years of Age With Epilepsy For Patients TAKING Valproatea For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,b or Valproatea For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproate a Weeks 1 and 20.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide)0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet0.6 mg/kg/day
Weeks 3 and 4
in 2 divided doses, rounded down to the nearest whole tablet0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide)0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet1.2 mg/kg/day
Week 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual maintenance dose
in 2 divided doses, rounded down to the nearest whole tablet1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses)
1 to 3 mg/kg/day with valproate alone4.5 to 7.5 mg/kg/day
5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg
(maximum 300 mg/day in 2 divided doses)May need to be increased by as much as 50%, based on clinical response
May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical responseNote: Only whole tablets should be used for dosing.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years of Age Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of lamotrigine tablets (chewable, dispersible) 2-mg and 5-mg Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every day
aValproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets (chewable, dispersible) was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets (chewable, dispersible) as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets (chewable, dispersible) as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets (chewable, dispersible) under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets (chewable, dispersible).
The recommended maintenance dose of lamotrigine tablets (chewable, dispersible) as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets (chewable, dispersible) should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets (Chewable, Dispersible): After achieving a dose of 500 mg/day of lamotrigine tablets (chewable, dispersible) according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets (Chewable, Dispersible): The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets (Chewable, Dispersible) in Patients ≥16 Years of Age With Epilepsy Lamotrigine Tablets (Chewable, Dispersible) Valproate Step 1 Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day).Maintain previous stable dose.
Step 2 Maintain at 200 mg/day. Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week. Step 3 Increase to 300 mg/day and maintain for 1 week. Simultaneously decrease to 250 mg/day and maintain for 1 week. Step 4 Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day. Discontinue.Conversion From Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets (Chewable, Dispersible): No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets (chewable, dispersible) with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine tablets (chewable, dispersible) is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets (chewable, dispersible) is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets (chewable, dispersible) is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets (chewable, dispersible) should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets (chewable, dispersible) should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine tablets (chewable, dispersible) should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets (chewable, dispersible) may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets (chewable, dispersible) may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets (chewable, dispersible) [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets (chewable, dispersible) should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine Tablets (Chewable, Dispersible) for Patients With Bipolar Disorder For Patients TAKING Valproatea For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,b or Valproatea For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided dosesaValproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine. [see Drug Interactions (7), Clinical Pharmacology (12.3)].
Table 6. Dosage Adjustments to Lamotrigine Tablets (Chewable, Dispersible) for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone,b or Valproatea) After Discontinuation of Valproatea After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb
bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.Current dose of lamotrigine tablets (chewable, dispersible) (mg/day)
100Current dose of lamotrigine tablets (chewable, dispersible) (mg/day)
400 Week 1 Maintain current dose of lamotrigine tablets (chewable, dispersible) 150 400 Week 2 Maintain current dose of lamotrigine tablets (chewable, dispersible) 200 300 Week 3 onward Maintain current dose of lamotrigine tablets (chewable, dispersible) 200 200aValproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine. [see Drug Interactions (7), Clinical Pharmacology (12.3)].
bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine tablets (chewable, dispersible) was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine tablets (chewable, dispersible) has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
2.5 Administration of Lamotrigine Tablets (Chewable, Dispersible)Lamotrigine tablets (chewable, dispersible) may be swallowed whole, chewed, or dispersed in water or diluted fruit juice. If the tablets are chewed, consume a small amount of water or diluted fruit juice to aid in swallowing.
To disperse lamotrigine tablets (chewable, dispersible), add the tablets to a small amount of liquid (1 teaspoon, or enough to cover the medication). Approximately 1 minute later, when the tablets are completely dispersed, swirl the solution and consume the entire quantity immediately. No attempt should be made to administer partial quantities of the dispersed tablets.
-
American Health Packaging
![Lamotrigine Tablet, Chewable [American Health Packaging]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | American Health Packaging
![Lamotrigine Tablet, Chewable [American Health Packaging] Lamotrigine Tablet, Chewable [American Health Packaging]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash:There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets (chewable, dispersible) with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets (chewable, dispersible), or (3) exceeding the recommended dose escalation for lamotrigine tablets (chewable, dispersible). However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablets (chewable, dispersible) is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets (chewable, dispersible) not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Tablets (Chewable, Dispersible) Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets (chewable, dispersible) may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets (chewable, dispersible) should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives:Starting Lamotrigine Tablets (Chewable, Dispersible) in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets (chewable, dispersible) should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets (chewable, dispersible) based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets (chewable, dispersible) in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets (Chewable, Dispersible) in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives:For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets (chewable, dispersible) will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives:In women taking a stable dose of lamotrigine tablets (chewable, dispersible) and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets (chewable, dispersible) consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking lamotrigine tablets (chewable, dispersible) in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets (chewable, dispersible) should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives:For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7) , Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets (chewable, dispersible) will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets (chewable, dispersible) should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine tablets (chewable, dispersible) in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets (chewable, dispersible) should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets (chewable, dispersible) in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine tablets (chewable, dispersible) should be based on patients’ concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets (chewable, dispersible). Because there is inadequate experience in this population, lamotrigine tablets (chewable, dispersible) should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine tablets (chewable, dispersible) in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets (chewable, dispersible), a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets (chewable, dispersible). In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets (chewable, dispersible). However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets (chewable, dispersible) should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine Tablets (Chewable, Dispersible) in Patients Over 12 Years of Age With EpilepsyFor Patients TAKING Valproatea
For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,b or Valproatea
For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Week 5 onwards to maintenance
Increase by 25 to 50 mg/day every 1 to 2 weeks
Increase by 50 mg/day every 1 to 2 weeks
Increase by 100 mg/day every 1 to 2 weeks.
Usual maintenance dose
100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses)
225 to 375 mg/day
(in 2 divided doses)
300 to 500 mg/day
(in 2 divided doses)
aValproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
The smallest available strength of lamotrigine tablets (chewable, dispersible) is 2 mg, and only whole tablets should be administered. If the calculated dose cannot be achieved using whole tablets, the dose should be rounded down to the nearest whole tablet [see How Supplied/Storage and Handling (16) and Medication Guide].
Table 2. Escalation Regimen for Lamotrigine Tablets (Chewable, Dispersible) in Patients 2 to 12 Years of Age With EpilepsyFor Patients TAKING Valproatea
For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,b or Valproatea
For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproate a
Weeks 1 and 2
0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide)0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tabletWeeks 3 and 4
0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide)
0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tabletWeek 5 onwards to maintenance
The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
Usual maintenance dose
1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses)
1 to 3 mg/kg/day with valproate alone4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses)5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses)
Maintenance dose in patients less than 30 kg
May need to be increased by as much as 50%, based on clinical response
May need to be increased by as much as 50%, based on clinical response
May need to be increased by as much as 50%, based on clinical response
Note: Only whole tablets should be used for dosing.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years of Age Taking Valproate (Weeks 1 to 4) With Epilepsy
aValproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.If the patient’s weight is
Give this daily dose, using the most appropriate combination of lamotrigine tablets (chewable, dispersible) 2-mg and 5-mg
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets (chewable, dispersible) was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets (chewable, dispersible) as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets (chewable, dispersible) as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets (chewable, dispersible) under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets (chewable, dispersible).
The recommended maintenance dose of lamotrigine tablets (chewable, dispersible) as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets (chewable, dispersible) should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets (Chewable, Dispersible): After achieving a dose of 500 mg/day of lamotrigine tablets (chewable, dispersible) according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets (Chewable, Dispersible): The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets (Chewable, Dispersible) in Patients ≥16 Years of Age With EpilepsyLamotrigine Tablets (Chewable, Dispersible)
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion From Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets (Chewable, Dispersible): No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets (chewable, dispersible) with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine tablets (chewable, dispersible) is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets (chewable, dispersible) is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets (chewable, dispersible) is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets (chewable, dispersible) should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets (chewable, dispersible) should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine tablets (chewable, dispersible) should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets (chewable, dispersible) may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets (chewable, dispersible) may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets (chewable, dispersible) [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets (chewable, dispersible) should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine Tablets (Chewable, Dispersible) for Patients With Bipolar DisorderFor Patients TAKING Valproatea
For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,b or Valproatea
For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
aValproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine. [see Drug Interactions (7), Clinical Pharmacology (12.3)].
Table 6. Dosage Adjustments to Lamotrigine Tablets (Chewable, Dispersible) for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications
bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone,b or Valproatea)
After Discontinuation of Valproatea
After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb
Current dose of lamotrigine tablets (chewable, dispersible) (mg/day)
100
Current dose of lamotrigine tablets (chewable, dispersible) (mg/day)
400
Week 1
Maintain current dose of lamotrigine tablets (chewable, dispersible)
150
400
Week 2
Maintain current dose of lamotrigine tablets (chewable, dispersible)
200
300
Week 3 onward
Maintain current dose of lamotrigine tablets (chewable, dispersible)
200
200
aValproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine. [see Drug Interactions (7), Clinical Pharmacology (12.3)].
bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine tablets (chewable, dispersible) was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine tablets (chewable, dispersible) has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
2.5 Administration of Lamotrigine Tablets (Chewable, Dispersible)Lamotrigine tablets (chewable, dispersible) may be swallowed whole, chewed, or dispersed in water or diluted fruit juice. If the tablets are chewed, consume a small amount of water or diluted fruit juice to aid in swallowing.
To disperse lamotrigine tablets (chewable, dispersible), add the tablets to a small amount of liquid (1 teaspoon, or enough to cover the medication). Approximately 1 minute later, when the tablets are completely dispersed, swirl the solution and consume the entire quantity immediately. No attempt should be made to administer partial quantities of the dispersed tablets.
-
Physicians Total Care, Inc.
![Lamotrigine Tablet [Physicians Total Care, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Physicians Total Care, Inc.
![Lamotrigine Tablet [Physicians Total Care, Inc.] Lamotrigine Tablet [Physicians Total Care, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablets is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be increased, by as much as 2 fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2 fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (seeTable 1 orTable 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2 week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2 fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1to3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine tablets in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ see Drug Interactions (7), Clinical Pharmacology (12.3)] . † These drugs induce lamotrigine glucuronidation and increase clearance [ see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [ see Drug Interactions (7), Clinical Pharmacology (12.3)] . Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [ see Dosage and Administration (2.1)] . Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,† or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day (in 2 divided doses) Week 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks Usual Maintenance Dose100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses)
225 to 375 mg/day (in 2 divided doses)300 to 500 mg/day
(in 2 divided doses)
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ see Drug Interactions (7), Clinical Pharmacology (12.3)] . † These drugs induce lamotrigine glucuronidation and increase clearance [ see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [ see Drug Interactions (7), Clinical Pharmacology (12.3)] . Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [ see Dosage and Administration (2.1)] . Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,† or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Weeks 1 and 2 0.15 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3for weight based dosing guide) 0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet Week 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual Maintenance Dose 1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses)
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day (maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical responseNote: Only whole tablets should be used for dosing.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years of Age Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of lamotrigine tablets, 2 mg and 5 mg Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets: After achieving a dose of 500 mg/day of lamotrigine tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4 week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥ 16 Years of Age With Epilepsy Lamotrigine Valproate Step 1 Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day). Maintain previous stable dose. Step 2 Maintain at 200 mg/day. Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week. Step 3 Increase to 300 mg/day and maintain for 1 week. Simultaneously decrease to 250 mg/day and maintain for 1 week. Step 4 Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day. Discontinue.Conversion From Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2 week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2 week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ see Drug Interactions (7), Clinical Pharmacology (12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [ see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [ see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [ see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,† or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications * These drugs induce lamotrigine glucuronidation and increase clearance [ see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [ see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [ see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. † Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ see Drug Interactions (7), Clinical Pharmacology (12.3)]. Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone,* or Valproate†) After Discontinuation of Valproate† After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone* Current dose of Lamotrigine (mg/day) 100Current dose of Lamotrigine (mg/day)
400
Week 1 Maintain current dose of lamotrigine 150 400 Week 2 Maintain current dose of lamotrigine 200 300 Week 3 onward Maintain current dose of lamotrigine 200 200The benefit of continuing treatment in patients who had been stabilized in an 8 to 16 week open-label phase with lamotrigine tablets was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Aidarex Pharmaceuticals Llc
![Lamotrigine Tablet [Aidarex Pharmaceuticals Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Aidarex Pharmaceuticals Llc
![Lamotrigine Tablet [Aidarex Pharmaceuticals Llc] Lamotrigine Tablet [Aidarex Pharmaceuticals Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning ]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablet is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3) ].
Lamotrigine Tablets Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3) ] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3) ].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3) ], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3) ].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3) ]. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6) , Clinical Pharmacology (12.3) ], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7) , Clinical Pharmacology (12.3) ]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.
Discontinuation Strategy:
Epilepsy: For patients receiving lamotrigine tablets in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9) ].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9) ].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine Tablets in Patients Over 12 Years of Age With Epilepsya Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
For
For Patients NOT TAKING
For Patients
Patients
Carbamazepine,
TAKING
TAKING
Phenytoin,
Carbamazepine,
Valproatea
Phenobarbital,
Phenytoin,
or Primidoneb,
Phenobarbital,
or Valproatea
or Primidoneb
and NOT TAKING
Valproatea
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Weeks 5 onwards to
maintenance
Increase by 25 to
50 mg/day every 1 to 2 weeks
Increase by 50
mg/day every 1
to 2 weeks
Increase by
100 mg/day every
1 to 2 weeks.
Usual maintenance
dose
100 to 200 mg/day
with valproate alone
225 to 375 mg/day
(in 2 divided doses).
300 to 500 mg/day
(in 2 divided doses).
100 to 400 mg/day
with valproate
and other drugs that induce glucuronidation
(in 1 or 2 divided doses)
Patients 2 to 12 Years Of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine Tablets in Patients 2 to 12 Years of Age With EpilepsyNote: Only whole tablets should be used for dosing.
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
For Patients TAKING
Valproatea
For Patients NOT
TAKING Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea
For Patients TAKING
Carbamazepine, Phenytoin, Phenobarbital, or
Primidoneb and NOT
TAKING Valproatea
Weeks 1 and 2
0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the
nearest whole tablet (see Table 3 for weight
based dosing guide).
0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the
nearest whole tablet.
0.6 mg/kg/day
in 2 divided doses, rounded down to the
nearest whole tablet.
Weeks 3 and 4
0.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
(see Table 3 for weight
based dosing guide).
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet.
1.2 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet.
Weeks 5
onwards to
maintenance
The dose should be increased every
1 to 2 weeks as follows:
calculate 0.3 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose.
The dose should be increased every
1 to 2 weeks as follows:
calculate 0.6 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose
The dose should be increased every
1 to 2 weeks as follows:
calculate 1.2 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose
Usual
Maintenance
Dose
1 to 5 mg/kg/day
(maximum 200 mg/day
in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone
4.5 to 7.5 mg/kg/day
(maximum 300 mg/day
in 2 divided doses)
5 to 15 mg/kg/day
(maximum 400 mg/day
in 2 divided doses)
Maintenance dose in
patients
less than 30 kg
May need to be increased
by as much as 50%,
based on clinical response
May need to be increased
by as much as 50%,
based on clinical response
May need to be increased
by as much as 50%, based
on clinical response
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is
Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in two divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets: After achieving a dose of 500 mg/day of lamotrigine tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets:
The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets in Patients ≥16 Years of Age with Epilepsy
Lamotrigine Tablets
Valproate
Step 1
Achieve a dose of 200 mg/day according to
guidelines in Table 1
(if not already on 200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than
500 mg/day/week and then maintain the dose of
500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to
250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every
week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2) ]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7) , Clinical Pharmacology (12.3) ].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning ].
Table 5. Escalation Regimen for Lamotrigine Tablets for Patients With Bipolar Disordera Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
For Patients TAKING
Valproatea
For Patients NOT TAKING
Carbamazepine, Phenytoin, Phenobarbital,
Primidoneb, or Valproatea
For Patients TAKING
Carbamazepine, Phenytoin,
Phenobarbital, or Primidoneband NOT TAKING
Valproatea
Weeks 1 and 2
25 mg every
other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
Table 6. Dosage Adjustments to Lamotrigine Tablets for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications
Discontinuation of Psychotropic Drugs
(excluding Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea)
After Discontinuation of
Valproatea
After Discontinuation of
Carbamazepine, Phenytoin,
Phenobarbital, or Primidoneb
Current dose of lamotrigine tablets
(mg/day)
100
Current dose of lamotrigine tablets
(mg/day)
400
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Week 1
Maintain current dose of lamotrigine tablets
150
400
Week 2
Maintain current dose of lamotrigine tablets
200
300
Week 3 onward
Maintain current dose of lamotrigine tablets
200
200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine tablets was established in two randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2) ]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Aidarex Pharmaceuticals Llc
![Lamotrigine Tablet [Aidarex Pharmaceuticals Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Aidarex Pharmaceuticals Llc
![Lamotrigine Tablet [Aidarex Pharmaceuticals Llc] Lamotrigine Tablet [Aidarex Pharmaceuticals Llc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of Lamotrigine with valproate, (2) exceeding the recommended initial dose of Lamotrigine, or (3) exceeding the recommended dose escalation for Lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of Lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that Lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with Lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued Lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued Lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of Lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with Lamotrigine. Because Lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of Lamotrigine and doses of Lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for Lamotrigine. Dosing of Lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of Lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for Lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with Lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of Lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of Lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent Lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of Lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent Lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless Lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in Lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased Lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to Lamotrigine consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of Lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of Lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent Lamotrigine plasma level. The decrease in dose of Lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or Lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of Lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of Lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of Lamotrigine up to 2-fold, and the progestin-only pills had no effect on Lamotrigine plasma levels. Therefore, adjustments to the dosage of Lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of Lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with Lamotrigine. Because there is inadequate experience in this population, Lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving Lamotrigine in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with Lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation should prolong the half-life of Lamotrigine; discontinuing valproate should shorten the half-life of Lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of Lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of Lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of Lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine [see Drug Interactions ( 7 ), Clinical Pharmacology ( 12.3 )]. † These drugs induce Lamotrigine glucuronidation and increase clearance [see Drug Interactions ( 7 ) Clinical Pharmacology ( 12.3 )]. Other drugs, that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions ( 7 ), Clinical Pharmacology ( 12.3 )]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration ( 2.1 )]. Patients on rifampin, or other drugs that induce Lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†,or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day (in 2 divided doses) Weeks 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day
every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks Usual Maintenance Dose 100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses) 225 to 375 mg/day
(in 2 divided doses) 300 to 500 mg/day (in 2 divided doses)Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine [see Drug Interactions (7 ), Clinical Pharmacology (12.3)]. † These drugs induce Lamotrigine glucuronidation and increase clearance [see Drug Interactions (7 ) Clinical Pharmacology (12.3)]. Other drugs, that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7 ) Clinical Pharmacology (12.3)].
Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration ( 2.1 )]. Patients on rifampin, or other drugs that induce Lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine,
Phenytoin,
Phenobarbital,
Primidone† or
Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Weeks 1 and 2 0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual Maintenance Dose 1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day
(maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response Note: Only whole tablets should be used for dosing. Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of Lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive Lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive Lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with Lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of Lamotrigine.
The recommended maintenance dose of Lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of Lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age with EpilepsyLamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
2.4 Bipolar Disorder
Conversion from Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with Lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.The goal of maintenance treatment with Lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of Lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of Lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin, that increase the apparent clearance of Lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with Lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of Lamotrigine should be adjusted. For patients discontinuing valproate, the dose of Lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation, the dose of Lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of Lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of Lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of Lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine [see Drug Interactions (7 ), Clinical Pharmacology (12.3)]. † These drugs induce Lamotrigine glucuronidation and increase clearance [see Drug Interactions (7 ), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen- containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)].
Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce Lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/ maintenance regimen as that used with anticonvulsants that have this effect. For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications * These drugs induce Lamotrigine glucuronidation and increase clearance [see Drug Interactions (7 ), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce Lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/ maintenance regimen as that used with anticonvulsants that have this effect. † Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone*, or Valproate†)
After Discontinuation of Valproate† After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone* Current dose of Lamotrigine (mg/day) 100Current dose of Lamotrigine (mg/day) 400
Week 1 Maintain current dose of Lamotrigine 150 400 Week 2 Maintain current dose of Lamotrigine 200 300 Week 3 onward Maintain current dose of Lamotrigine 200 200The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with Lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with Lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Preferred Pharmaceuticals, Inc.
![Lamotrigine Tablet [Preferred Pharmaceuticals, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Preferred Pharmaceuticals, Inc.
![Lamotrigine Tablet [Preferred Pharmaceuticals, Inc.] Lamotrigine Tablet [Preferred Pharmaceuticals, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of Lamotrigine with valproate, (2) exceeding the recommended initial dose of Lamotrigine, or (3) exceeding the recommended dose escalation for Lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of Lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that Lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with Lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued Lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued Lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of Lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with Lamotrigine. Because Lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of Lamotrigine and doses of Lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for Lamotrigine. Dosing of Lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of Lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for Lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with Lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of Lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of Lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent Lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of Lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent Lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless Lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in Lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased Lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to Lamotrigine consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of Lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of Lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent Lamotrigine plasma level. The decrease in dose of Lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or Lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of Lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of Lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of Lamotrigine up to 2-fold, and the progestin-only pills had no effect on Lamotrigine plasma levels. Therefore, adjustments to the dosage of Lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of Lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with Lamotrigine. Because there is inadequate experience in this population, Lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving Lamotrigine in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with Lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation should prolong the half-life of Lamotrigine; discontinuing valproate should shorten the half-life of Lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of Lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of Lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of Lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine [see Drug Interactions ( 7 ), Clinical Pharmacology ( 12.3 )]. † These drugs induce Lamotrigine glucuronidation and increase clearance [see Drug Interactions ( 7 ) Clinical Pharmacology ( 12.3 )]. Other drugs, that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions ( 7 ), Clinical Pharmacology ( 12.3 )]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration ( 2.1 )]. Patients on rifampin, or other drugs that induce Lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.For Patients TAKING Valproate*
For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†,or Valproate*
For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate*
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day (in 2 divided doses)
Weeks 5 onwards to maintenance
Increase by 25 to 50 mg/day every 1 to 2 weeks
Increase by 50 mg/day
every 1 to 2 weeksIncrease by 100 mg/day every 1 to 2 weeks
Usual Maintenance Dose
100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses)225 to 375 mg/day
(in 2 divided doses)300 to 500 mg/day (in 2 divided doses)
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine [see Drug Interactions (7 ), Clinical Pharmacology (12.3)]. † These drugs induce Lamotrigine glucuronidation and increase clearance [see Drug Interactions (7 ) Clinical Pharmacology (12.3)]. Other drugs, that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7 ) Clinical Pharmacology (12.3)].
Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration ( 2.1 )]. Patients on rifampin, or other drugs that induce Lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.For Patients TAKING Valproate*
For Patients NOT TAKING Carbamazepine,
Phenytoin,
Phenobarbital,
Primidone† or
Valproate*For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate*
Weeks 1 and 2
0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide)0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tabletWeeks 3 and 4
0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide)0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tabletWeeks 5 onwards to maintenance
The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
Usual Maintenance Dose
1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses)5 to 15 mg/kg/day
(maximum 400 mg/day in 2 divided doses)Maintenance dose in patients less than 30 kg
May need to be increased by as much as 50%, based on clinical response
May need to be increased by as much as 50%, based on clinical response
May need to be increased by as much as 50%, based on clinical response
Note: Only whole tablets should be used for dosing.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With EpilepsyIf the patient’s weight is
Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of Lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive Lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive Lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with Lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of Lamotrigine.
The recommended maintenance dose of Lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of Lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age with EpilepsyLamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
2.4 Bipolar Disorder
Conversion from Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with Lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.The goal of maintenance treatment with Lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of Lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of Lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin, that increase the apparent clearance of Lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with Lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of Lamotrigine should be adjusted. For patients discontinuing valproate, the dose of Lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation, the dose of Lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of Lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of Lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of Lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine [see Drug Interactions (7 ), Clinical Pharmacology (12.3)]. † These drugs induce Lamotrigine glucuronidation and increase clearance [see Drug Interactions (7 ), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen- containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)].
Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce Lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/ maintenance regimen as that used with anticonvulsants that have this effect.For Patients TAKING Valproate*
For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate*
For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate*
Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications * These drugs induce Lamotrigine glucuronidation and increase clearance [see Drug Interactions (7 ), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce Lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/ maintenance regimen as that used with anticonvulsants that have this effect. † Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone*, or Valproate†)
After Discontinuation of Valproate†
After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone*
Current dose of Lamotrigine (mg/day) 100
Current dose of Lamotrigine (mg/day) 400
Week 1
Maintain current dose of Lamotrigine
150
400
Week 2
Maintain current dose of Lamotrigine
200
300
Week 3 onward
Maintain current dose of Lamotrigine
200
200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with Lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with Lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Taro Pharmaceuticals U.s.a., Inc.
![Lamotrigine Tablet, Chewable [Taro Pharmaceuticals U.s.a., Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Pd-rx Pharmaceuticals, Inc.
![Lamotrigine Tablet, Chewable [Taro Pharmaceuticals U.s.a., Inc.] Lamotrigine Tablet, Chewable [Taro Pharmaceuticals U.s.a., Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
General Principles:
The goal of replacement therapy is to achieve and maintain a clinical and biochemical euthyroid state. The goal of suppressive therapy is to inhibit growth and/or function of abnormal thyroid tissue. The dose of Levothyroxine Sodium Tablets, USP that is adequate to achieve these goals depends on a variety of factors including the patient's age, body weight, cardiovascular status, concomitant medical conditions, including pregnancy, concomitant medications, and the specific nature of the condition being treated (see WARNINGS and PRECAUTIONS). Hence, the following recommendations serve only as dosing guidelines. Dosing must be individualized and adjustments made based on periodic assessment of the patient's clinical response and laboratory parameters (see PRECAUTIONS, Laboratory Tests).
Levothyroxine Sodium Tablets, USP should be taken in the morning on an empty stomach, at least one-half hour to one hour before any food is eaten. Levothyroxine Sodium Tablets, USP should be taken at least 4 hours apart from drugs that are known to interfere with its absorption (see PRECAUTIONS, Drug Interactions).
Due to the long half-life of levothyroxine, the peak therapeutic effect at a given dose of levothyroxine sodium may not be attained for 4-6 weeks.
Caution should be exercised when administering Levothyroxine Sodium Tablets, USP to patients with underlying cardiovascular disease, to the elderly, and to those with concomitant adrenal insufficiency (see PRECAUTIONS).
Specific Patient Populations:
Hypothyroidism in Adults and in Children in Whom Growth and Puberty are Complete (see WARNINGS and PRECAUTIONS, Laboratory Tests).
Therapy may begin at full replacement doses in otherwise healthy individuals less than 50 years old and in those older than 50 years who have been recently treated for hyperthyroidism or who have been hypothyroid for only a short time (such as a few months). The average full replacement dose of levothyroxine sodium is approximately 1.7 mcg/kg/day (e.g., 100-125 mcg/day for a 70 kg adult). Older patients may require less than 1 mcg/kg/day. Levothyroxine sodium doses greater than 200 mcg/day are seldom required. An inadequate response to daily doses ≥ 300 mcg/day is rare and may indicate poor compliance, malabsorption, and/or drug interactions.
For most patients older than 50 years or for patients under 50 years of age with underlying cardiac disease, an initial starting dose of 25-50 mcg/day of levothyroxine sodium is recommended, with gradual increments in dose at 6-8 week intervals, as needed. The recommended starting dose of levothyroxine sodium in elderly patients with cardiac disease is 12.5-25 mcg/day, with gradual dose increments at 4-6 week intervals. The levothyroxine sodium dose is generally adjusted in 12.5-25 mcg increments until the patient with primary hypothyroidism is clinically euthyroid and the serum TSH has normalized.
In patients with severe hypothyroidism, the recommended initial levothyroxine sodium dose is 12.5-25 mcg/day with increases of 25 mcg/day every 2-4 weeks, accompanied by clinical and laboratory assessment, until the TSH level is normalized.
In patients with secondary (pituitary) or tertiary (hypothalamic) hypothyroidism, the levothyroxine sodium dose should be titrated until the patient is clinically euthyroid and the serum free-T4 level is restored to the upper half of the normal range.
Pediatric Dosage - Congenital or Acquired Hypothyroidism (see PRECAUTIONS, Laboratory Tests)
General Principles
In general, levothyroxine therapy should be instituted at full replacement doses as soon as possible. Delays in diagnosis and institution of therapy may have deleterious effects on the child's intellectual and physical growth and development.
Undertreatment and overtreatment should be avoided (see PRECAUTIONS, Pediatric Use).
Levothyroxine Sodium Tablets, USP may be administered to infants and children who cannot swallow intact tablets by crushing the tablet and suspending the freshly crushed tablet in a small amount (5-10 mL or 1-2 teaspoons) of water. This suspension can be administered by spoon or dropper. DO NOT STORE THE SUSPENSION. Foods that decrease absorption of levothyroxine, such as soybean infant formula, should not be used for administering levothyroxine sodium tablets. (see PRECAUTIONS, Drug-Food Interactions).
Newborns
The recommended starting dose of levothyroxine sodium in newborn infants is 10-15 mcg/kg/day. A lower starting dose (e.g., 25 mcg/day) should be considered in infants at risk for cardiac failure, and the dose should be increased in 4-6 weeks as needed based on clinical and laboratory response to treatment. In infants with very low (< 5 mcg/dL) or undetectable serum T4 concentrations, the recommended initial starting dose is 50 mcg/day of levothyroxine sodium.
Infants and Children
Levothyroxine therapy is usually initiated at full replacement doses, with the recommended dose per body weight decreasing with age (see TABLE 3). However, in children with chronic or severe hypothyroidism, an initial dose of 25 mcg/day of levothyroxine sodium is recommended with increments of 25 mcg every 2-4 weeks until the desired effect is achieved.
Hyperactivity in an older child can be minimized if the starting dose is one-fourth of the recommended full replacement dose, and the dose is then increased on a weekly basis by an amount equal to one-fourth the full-recommended replacement dose until the full recommended replacement dose is reached.
Table 3: Levothyroxine Sodium Dosing Guidelines for Pediatric Hypothyroidism a. The dose should be adjusted based on clinical response and laboratory parameters (see PRECAUTlONS, Laboratory Tests and Pediatric Use). AGE Daily Dose Per Kg Body Weighta 0-3 months 10-15 mcg/kg/day 3-6 months 8-10 mcg/kg/day 6-12 months 6-8 mcg/kg/day 1-5 years 5-6 mcg/kg/day 6-12 years 4-5 mcg/kg/day >12 years but growth and puberty incomplete 2-3 mcg/kg/day Growth and puberty complete 1.7 mcg/kg/dayPregnancy- Pregnancy may increase levothyroxine requirements (see PREGNANCY).
Subclinical Hypothyroidism- If this condition is treated, a lower levothyroxine sodium dose (e.g., 1 mcg/kg/day) than that used for full replacement may be adequate to normalize the serum TSH level. Patients who are not treated should be monitored yearly for changes in clinical status and thyroid laboratory parameters.
TSH Suppression in Well-differentiated Thyroid Cancer and Thyroid Nodules- The target level for TSH suppression in these conditions has not been established with controlled studies. In addition, the efficacy of TSH suppression for benign nodular disease is controversial. Therefore, the dose of Levothyroxine Sodium Tablets, USP used for TSH suppression should be individualized based on the specific disease and the patient being treated.
In the treatment of well differentiated (papillary and follicular) thyroid cancer, levothyroxine is used as an adjunct to surgery and radioiodine therapy. Generally, TSH is suppressed to <0.1 mU/L, and this usually requires a levothyroxine sodium dose of greater than 2 mcg/kg/day. However, in patients with high-risk tumors, the target level for TSH suppression may be <0.01 mU/L.
In the treatment of benign nodules and nontoxic multinodular goiter, TSH is generally suppressed to a higher target (e.g., 0.1-0.5 mU/L for nodules and 0.5-1.0 mU/L for multinodular goiter) than that used for the treatment of thyroid cancer. Levothyroxine sodium is contraindicated if the serum TSH is already suppressed due to the risk of precipitating overt thyrotoxicosis (see CONTRAINDICATIONS, WARNINGS and PRECAUTIONS).
Myxedema Coma - Myxedema coma is a life-threatening emergency characterized by poor circulation and hypometabolism, and may result in unpredictable absorption of levothyroxine sodium from the gastrointestinal tract. Therefore, oral thyroid hormone drug products are not recommended to treat this condition. Thyroid hormone products formulated for intravenous administration should be administered.
-
Torrent Pharmaceuticals Limited
![Lamotrigine (Lamotrigine ) Tablet Lamotrigine (Lamotrigine) Kit [Torrent Pharmaceuticals Limited]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Torrent Pharmaceuticals Limited
![Lamotrigine (Lamotrigine ) Tablet Lamotrigine (Lamotrigine) Kit [Torrent Pharmaceuticals Limited] Lamotrigine (Lamotrigine ) Tablet Lamotrigine (Lamotrigine) Kit [Torrent Pharmaceuticals Limited]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
Lamotrigine Starter Kits provide lamotrigine at doses consistent with the recommended titration schedule for the first 5 weeks of treatment, based upon concomitant medications for patients with epilepsy (>12 years of age) and Bipolar I Disorder (≥18 years of age) and are intended to help reduce the potential for rash. The use of lamotrigine Starter Kits is recommended for appropriate patients who are starting or restarting lamotrigine [see How Supplied/Storage and Handling (16)].
It is recommended that lamotrigine tablets, USP not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsya Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
For Patients TAKING
Valproatea
For Patients NOT
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital,
Primidoneb, or
Valproatea
For Patients
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidoneb and
NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Week 5
onwards to
maintenance
Increase by 25 to 50
mg/day every 1 to
2 weeks
Increase by 50
mg/day every 1 to
2 weeks
Increase by 100
mg/day every 1 to
2 weeks.
Usual
Maintenance
Dose
100 to 200 mg/day
with valproate
alone
100 to 400 mg/day
with valproate and
other drugs that
induce
glucuronidation
(in 1 or 2 divided
doses)
225 to 375 mg/day
(in 2 divided doses)
300 to 500 mg/day
(in 2 divided doses)
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
The smallest available strength of lamotrigine tablets is 25 mg, and only whole tablets should be administered. If the calculated dose cannot be achieved using whole tablets, the dose should be rounded down to the nearest whole tablet [see How Supplied/Storage and Handling (16) and Medication Guide].
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With EpilepsyNote: Only whole tablets should be used for dosing.
aValproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7),
Clinical Pharmacology (12.3)].bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)].
Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see
Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
For Patients
TAKING Valproatea
For Patients NOT
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital,
Primidoneb, or
Valproatea
For Patients TAKING
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidoneb and NOT
TAKING Valproatea
Weeks 1
and 2
0.15 mg/kg/day
in 1 or 2 divided
doses, rounded
down to the nearest
whole tablet (see
Table 3 for weight-based dosing guide)
0.3 mg/kg/day
in 1 or 2 divided
doses, rounded down
to the nearest whole
tablet
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
Weeks 3
and 4
0.3 mg/kg/day
in 1 or 2 divided
doses, rounded
down to the nearest
whole tablet (see
Table 3 for weight-based dosing guide)
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
1.2 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
Week 5
onwards to
maintenance
The dose should be
increased every 1 to
2 weeks as follows:
calculate 0.3 mg/kg/day,
round this amount
down to the nearest
whole tablet, and
add this amount to
the previously
administered daily
dose
The dose should be increased every 1 to
2 weeks as follows: calculate
0.6 mg/kg/day, round
this amount down to
the nearest whole
tablet, and add this
amount to the
previously
administered daily
dose
The dose should be increased every 1 to
2 weeks as follows: calculate
1.2 mg/kg/day, round
this amount down to
the nearest whole
tablet, and add this
amount to the
previously
administered daily
dose
Usual
Maintenance
Dose
1 to 5 mg/kg/day
(maximum
200 mg/day in 1 or 2
divided doses).
1 to 3 mg/kg/day
with valproate alone
4.5 to 7.5 mg/kg/day
(maximum 300
mg/day in 2 divided
doses)
5 to 15 mg/kg/day
(maximum 400
mg/day in 2 divided
doses)
Maintenance
dose in
patients less
than 30 kg
May need to be
increased by as
much as 50%, based
on clinical response
May need to be
increased by as much
as 50%, based on
clinical response
May need to be
increased by as much
as 50%, based on
clinical response
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years of Age Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is
Give this daily dose, using the most appropriate combination of lamotrigine
2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age With Epilepsy
Lamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to
guidelines in Table 1 (if not already on
200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by
decrements no greater than
500 mg/day/week and then
maintain the dose of
500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1
week.
Simultaneously decrease to
250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve
maintenance dose of 500 mg/day.
Discontinue.
Conversion From Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disordera Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
For Patients TAKING Valproatea
For Patients NOT TAKING
Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea
For Patients TAKING
Carbamazepine, Phenytoin, Phenobarbital,
or Primidoneb and
NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in
divided doses
Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medicationsa Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Discontinuation of Psychotropic Drugs
(excluding Carbamazepine, Phenytoin,
After Discontinuation of Valproatea
After Discontinuation of Carbamazepine,
Phenytoin, Phenobarbital,or
Primidoneb
Phenobarbital, Primidoneb, or Valproatea)
Current dose of Lamotrigine (mg/day)
100
Current dose of Lamotrigine (mg/day)
400
Week 1
Maintain current dose of Lamotrigine
150
400
Week 2
Maintain current dose of Lamotrigine
200
300
Week 3 onward
Maintain current dose of Lamotrigine
200
200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Glenmark Generics Inc., Usa
![Lamotrigine Tablet, Chewable [Glenmark Generics Inc., Usa]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Glenmark Pharmaceuticals Inc., Usa
![Lamotrigine Tablet, Chewable [Glenmark Generics Inc., Usa] Lamotrigine Tablet, Chewable [Glenmark Generics Inc., Usa]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation for lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation:
Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine. Drugs that induce glucuronidation include carbamazepine, phenytoin, phenobarbital, primidone, rifampin, estrogen-containing oral contraceptives, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Valproate inhibits glucuronidation. For dosing considerations for lamotrigine in patients on estrogen-containing contraceptives and atazanavir/ritonavir, see below and Table 13. For dosing considerations for lamotrigine in patients on other drugs known to induce or inhibit glucuronidation, see Tables 1, 2, 5-6, and 13.Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder:
A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].Women Taking Estrogen-Containing Oral Contraceptives:Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives:
Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED or other concomitant medications (see Tables 1, 5, and 7). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.Adjustments to the Maintenance Dose of Lamotrigine In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: In women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose to maintain a consistent lamotrigine plasma level.
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Tables 1 and 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (pill-free week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine consistently occur during the pill-free week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the pill-free week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: In women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. In women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients Taking Atazanavir/Ritonavir:
While atazanavir/ritonavir does reduce the lamotrigine plasma concentration, no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of atazanavir/ritonavir. Dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on concomitant AED or other concomitant medications (see Tables 1, 2, and 5). In patients already taking maintenance doses of lamotrigine and not taking glucuronidation inducers, the dose of lamotrigine may need to be increased if atazanavir/ritonavir is added, or decreased if atazanavir/ritonavir is discontinued [see Clinical Pharmacology (12.3)].
Patients With Hepatic Impairment:Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 subjects with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment:Initial doses of lamotrigine should be based on patients' concomitant medications (see Tables 1-3 and 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy:For patients receiving lamotrigine in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.8)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder:In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In the clinical development program in adults with bipolar disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.8)].
2.2 Epilepsy - Adjunctive TherapyThis section provides specific dosing recommendations for patients older than 12 years and patients aged 2 to 12 years. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AEDs or other concomitant medications (see Table 1 for patients older than 12 years and Table 2 for patients aged 2 to 12 years). A weight-based dosing guide for patients aged 2 to 12 years on concomitant valproate is provided in Table 3.
Patients Older Than 12 Years:Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Older Than 12 Years With EpilepsyIn Patients TAKING Valproatea
In Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidoneb, or Valproatea
In Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day (in 2 divided doses)
Week 5 onward to maintenance
Increase by 25 to 50 mg/day every 1 to 2 weeks
Increase by 50 mg/day every 1 to 2 weeks
Increase by 100 mg/day every 1 to 2 weeks.
Usual Maintenance Dose
100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation (in 1 or 2 divided doses)
225 to 375 mg/day (in 2 divided doses)
300 to 500 mg/day (in 2 divided doses)
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b Drugs that induce lamotrigine glucuronidation and clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), Clinical Pharmacology (12.3)].
Patients Aged 2 to 12 Years:Recommended dosing guidelines are summarized in Table 2.
Lower starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by lower starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
The smallest available strength of lamotrigine tablets (chewable, dispersible) is 2 mg, and only whole tablets should be administered. If the calculated dose cannot be achieved using whole tablets, the dose should be rounded down to the nearest whole tablet[see How Supplied/Storage and Handling (16) and MEDICATION GUIDE].
Table 2. Escalation Regimen for Lamotrigine in Patients Aged 2 to 12 Years With EpilepsyIn Patients TAKING Valproatea
In Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidoneb, or Valproatea
In Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea
Weeks 1 and 2
0.15 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide)
0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet
0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet
Weeks 3 and 4
0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide)
0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet
1.2 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet
Week 5 onward to maintenance
The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
Usual Maintenance Dose
1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses) 1 to 3 mg/kg/day with valproate alone
4.5 to 7.5 mg/kg/day (maximum 300 mg/day in 2 divided doses)
5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses)
Maintenance dose in patients less than 30 kg
May need to be increased by as much as 50%, based on clinical response
May need to be increased by as much as 50%, based on clinical response
May need to be increased by as much as 50%, based on clinical response
Note: Only whole tablets should be used for dosing.
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)].
Table 3. The Initial Weight-Based Dosing Guide for Patients Aged 2 to 12 Years Taking Valproate (Weeks 1 to 4) With EpilepsyIf the patient’s weight is
Give this daily dose, using the most appropriate combination of lamotrigine 2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for EpilepsyThe usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive trials in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 - 4 has not been established in controlled trials.
2.3 Epilepsy - Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to attempt to maintain seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations for lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With LamotrigineAfter achieving a dose of 500 mg/day of lamotrigine using the guidelines in Table 1, the concomitant enzyme-inducing AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With LamotrigineThe conversion regimen involves the 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients Aged 16 Years and Older With EpilepsyLamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1.
Maintain established stable dose.
Step 2
Maintain at 200 mg/day.
Decrease dose by decrements no greater than 500 mg/day/week to 500 mg/day and then maintain for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With LamotrigineNo specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenytoin, phenobarbital, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy [see Indications and Usage (1)]. Patients taking lamotrigine for more than 16 weeks should be periodically reassessed to determine the need for maintenance treatment.
Adults
The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitor lopinavir/ritonavir that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended.
Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. In patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). In patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine in Adults With Bipolar DisorderIn Patients TAKING Valproatea
In Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidoneb, or Valproatea
In Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)].
Table 6. Dosage Adjustments to Lamotrigine In Adults With Bipolar Disorder Following Discontinuation of Psychotropic MedicationsDiscontinuation of Psychotropic Drugs (excluding Valproatea, Carbamazepine, Phenytoin, Phenobarbital or Primidoneb)
After Discontinuation of Valproatea
After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb
Current dose of lamotrigine (mg/day) 100
Current dose of lamotrigine (mg/day) 400
Week 1
Maintain current dose of lamotrigine
150
400
Week 2
Maintain current dose of lamotrigine
200
300
Week 3 onward
Maintain current dose of lamotrigine
200
200
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)].
2.5 Administration of Lamotrigine Tablets (chewable, dispersible)Lamotrigine tablets (chewable, dispersible) may be swallowed whole, chewed, or dispersed in water or diluted fruit juice. If the tablets are chewed, consume a small amount of water or diluted fruit juice to aid in swallowing.
To disperse lamotrigine tablets (chewable, dispersible), add the tablets to a small amount of liquid (1 teaspoon, or enough to cover the medication). Approximately 1 minute later, when the tablets are completely dispersed, swirl the solution and consume the entire quantity immediately. No attempt should be made to administer partial quantities of the dispersed tablets.
-
Taro Pharmaceuticals U.s.a., Inc.
![Lamotrigine Tablet [Taro Pharmaceuticals U.s.a., Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Taro Pharmaceuticals U.s.a., Inc.
![Lamotrigine Tablet [Taro Pharmaceuticals U.s.a., Inc.] Lamotrigine Tablet [Taro Pharmaceuticals U.s.a., Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation for lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine. Drugs that induce glucuronidation include carbamazepine, phenytoin, phenobarbital, primidone, rifampin, estrogen-containing oral contraceptives, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Valproate inhibits glucuronidation. For dosing considerations for lamotrigine in patients on estrogen-containing contraceptives and atazanavir/ritonavir, see below and Table 13. For dosing considerations for lamotrigine in patients on other drugs known to induce or inhibit glucuronidation, see Tables 1, 2, 5-6, and 13.
Target Plasma Levels for Patients with Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED or other concomitant medications (see Tables 1, 5, and 7). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: In women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be increased by as much as 2-fold over the recommended target maintenance dose to maintain a consistent lamotrigine plasma level.
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Tables 1 and 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (pill-free week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine consistently occur during the pill-free week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the pill-free week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: In women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. In women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients Taking Atazanavir/Ritonavir: While atazanavir/ritonavir does reduce the lamotrigine plasma concentration, no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of atazanavir/ritonavir. Dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on concomitant AED or other concomitant medications (see Tables 1, 2, and 5). In patients already taking maintenance doses of lamotrigine and not taking glucuronidation inducers, the dose of lamotrigine may need to be increased if atazanavir/ritonavir is added, or decreased if atazanavir/ritonavir is discontinued [see Clinical Pharmacology (12.3)].
Patients with Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 subjects with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients with Renal Impairment: Initial doses of lamotrigine should be based on patients' concomitant medications (see Tables 1-3 and 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.8)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In the clinical development program in adults with bipolar disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.8)].
2.2 Epilepsy—Adjunctive TherapyThis section provides specific dosing recommendations for patients older than 12 years and patients aged 2 to 12 years. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AEDs or other concomitant medications (see Table 1 for patients older than 12 years and Table 2 for patients aged 2 to 12 years). A weight-based dosing guide for patients aged 2 to 12 years on concomitant valproate is provided in Table 3.
Patients Older than 12 Years: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Older than 12 Years with Epilepsy In Patients TAKING Valproate* In Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,† or Valproate* In Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)]. Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day (in 2 divided doses) Week 5 onward to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks. Increase by 50 mg/day every 1 to 2 weeks. Increase by 100 mg/day every 1 to 2 weeks. Usual maintenance dose 100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses) 225 to 375 mg/day
(in 2 divided doses) 300 to 500 mg/day
(in 2 divided doses)Patients Aged 2 to 12 Years: Recommended dosing guidelines are summarized in Table 2.
Lower starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by lower starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients Aged 2 to 12 Years with Epilepsy In Patients TAKING Valproate* In Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,† or Valproate* In Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Note: Only whole tablets should be used for dosing. * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)]. Weeks 1 and 2 0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide) 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide) 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Week 5 onward to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose. The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose. The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose. Usual maintenance dose 1 to 5 mg/kg/day
(maximum 200 mg/day in 1 or 2 divided doses)
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day
(maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response. May need to be increased by as much as 50%, based on clinical response. May need to be increased by as much as 50%, based on clinical response. Table 3. The Initial Weight-Based Dosing Guide for Patients Aged 2 to 12 Years Taking Valproate (Weeks 1 to 4) with Epilepsy If the patient's weight is Give this daily dose, using the most appropriate combination of Lamotrigine 2- and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive trials in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1-4 has not been established in controlled trials.
2.3 Epilepsy—Conversion from Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to attempt to maintain seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations for lamotrigine should not be exceeded [see Boxed Warning].
Conversion from Adjunctive Therapy with Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy with Lamotrigine: After achieving a dose of 500 mg/day of lamotrigine using the guidelines in Table 1, the concomitant enzyme-inducing AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy with Valproate to Monotherapy with Lamotrigine: The conversion regimen involves the 4 steps outlined in Table 4.
Table 4. Conversion from Adjunctive Therapy with Valproate to Monotherapy with Lamotrigine in Patients Aged 16 Years and Older With Epilepsy Lamotrigine Valproate Step 1 Achieve a dose of 200 mg/day according to guidelines in Table 1. Maintain established stable dose. Step 2 Maintain at 200 mg/day. Decrease dose by decrements no greater than 500 mg/day/week to 500 mg/day and then maintain for 1 week. Step 3 Increase to 300 mg/day and maintain for 1 week. Simultaneously decrease to 250 mg/day and maintain for 1 week. Step 4 Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day. Discontinue.Conversion from Adjunctive Therapy with Antiepileptic Drugs other than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy with Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenytoin, phenobarbital, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy [see Indications and Usage (1)].
Patients taking lamotrigine for more than 16 weeks should be periodically reassessed to determine the need for maintenance treatment.
Adults
The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitor lopinavir/ritonavir that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. In patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). In patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine in Adults with Bipolar Disorder In Patients TAKING Valproate* In Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone,† or Valproate* In Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)]. Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to Lamotrigine in Adults with Bipolar Disorder Following Discontinuation of Psychotropic Medications Discontinuation of Psychotropic Drugs (excluding Valproate,* Carbamazepine, Phenytoin, Phenobarbital, or Primidone†) After Discontinuation of Valproate* After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone† Current Dose of Lamotrigine (mg/day) 100 Current Dose of Lamotrigine (mg/day) 400 * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)]. Week 1 Maintain current dose of Lamotrigine 150 400 Week 2 Maintain current dose of Lamotrigine 200 300 Week 3 onward Maintain current dose of Lamotrigine 200 200 -
Wilshire Pharmaceuticals, Inc.
![Lamotrigine Tablet, Film Coated, Extended Release [Wilshire Pharmaceuticals, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Teva Pharmaceuticals Usa Inc
![Lamotrigine Tablet, Film Coated, Extended Release [Wilshire Pharmaceuticals, Inc.] Lamotrigine Tablet, Film Coated, Extended Release [Wilshire Pharmaceuticals, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Donepezil hydrochloride tablets should be taken in the evening, just prior to retiring.
Donepezil hydrochloride tablets can be taken with or without food.
2.1 Mild to Moderate Alzheimer’s DiseaseThe dosages of donepezil hydrochloride tablets shown to be effective in controlled clinical trials are 5 mg and 10 mg administered once per day.
The higher dose of 10 mg did not provide a statistically significantly greater clinical benefit than 5 mg. There is a suggestion, however, based upon order of group mean scores and dose trend analyses of data from these clinical trials, that a daily dose of 10 mg of donepezil hydrochloride tablets might provide additional benefit for some patients. Accordingly, whether or not to employ a dose of 10 mg is a matter of prescriber and patient preference.
2.2 Severe Alzheimer’s DiseaseDonepezil hydrochloride tablets have been shown to be effective in controlled clinical trials at a dose of 10 mg administered once daily.
2.3 TitrationThe recommended starting dose of donepezil hydrochloride tablets is 5 mg once daily. Evidence from the controlled trials in mild to moderate Alzheimer’s disease indicates that the 10 mg dose, with a one week titration, is likely to be associated with a higher incidence of cholinergic adverse events compared to the 5 mg dose. In open-label trials using a 6 week titration, the type and frequency of these same adverse events were similar between the 5 mg and 10 mg dose groups. Therefore, because donepezil hydrochloride tablets steady state is achieved about 15 days after it is started and because the incidence of untoward effects may be influenced by the rate of dose escalation, a dose of 10 mg should not be administered until patients have been on a daily dose of 5 mg for 4 to 6 weeks.
-
Unit Dose Services
![Lamotrigine Tablet [Unit Dose Services]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Unit Dose Services
![Lamotrigine Tablet [Unit Dose Services] Lamotrigine Tablet [Unit Dose Services]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing Considerations: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of Lamotrigine with valproate, (2) exceeding the recommended initial dose of Lamotrigine, or (3) exceeding the recommended dose escalation for Lamotrigine. However, cases have occurred in the absence of these factors . Therefore, it is important that the dosing recommendations be followed closely. Rash[seeBoxed Warning]
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of Lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that Lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with Lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued Lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued Lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of Lamotrigine is affected by other concomitant medications . [see Clinical Pharmacology (12.3)]
: Drugs other than those listed in the Clinical Pharmacology section have not been systematically evaluated in combination with Lamotrigine. Because Lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of Lamotrigine and doses of Lamotrigine may require adjustment based on clinical response. Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation[see Clinical Pharmacology (12.3)]
A therapeutic plasma concentration range has not been established for Lamotrigine. Dosing of Lamotrigine should be based on therapeutic response . Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder:[see Clinical Pharmacology (12.3)]
: Although estrogen-containing oral contraceptives have been shown to increase the clearance of Lamotrigine , no adjustments to the recommended dose-escalation guidelines for Lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with Lamotrigine based on the concomitant AED or other concomitant medications (see or ). See below for adjustments to maintenance doses of Lamotrigine in women taking estrogen-containing oral contraceptives. Women Taking Estrogen-Containing Oral ContraceptivesStarting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives:[see Clinical Pharmacology (12.3)]Table 1Table 5
Adjustments to the Maintenance Dose of Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives:
For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation , the maintenance dose of Lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent Lamotrigine plasma level . (1) Taking Estrogen-Containing Oral Contraceptives:[see Drug Interactions ( ), 7Clinical Pharmacology ( )] 12.3[see Clinical Pharmacology (12.3)]
In women taking a stable dose of Lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent Lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see or ) unless Lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in Lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased Lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to Lamotrigine consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation , no adjustment to the dose of Lamotrigine should be necessary. (2) Starting Estrogen-Containing Oral Contraceptives:[see Drug Interactions ( ), Clinical Pharmacology ( )], 712.3Table 1Table 5[see Drug Interactions ( ), Clinical Pharmacology ( )] 712.3
For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation , the maintenance dose of Lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent Lamotrigine plasma level. The decrease in dose of Lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or Lamotrigine plasma levels indicate otherwise . For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation , no adjustment to the dose of Lamotrigine should be necessary. (3) Stopping Estrogen-Containing Oral Contraceptives:[see Drug Interactions ( ), Clinical Pharmacology ( )] 712.3[see Clinical Pharmacology ( )] 12.3[see Drug Interactions ( ), Clinical Pharmacology ( )] 712.3
: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of Lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of Lamotrigine up to 2-fold, and the progestin-only pills had no effect on Lamotrigine plasma levels. Therefore, adjustments to the dosage of Lamotrigine in the presence of progestogens alone will likely not be needed. Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy
: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment , the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response. Patients With Hepatic Impairment[see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)]
: Initial doses of Lamotrigine should be based on patients' concomitant medications (see or ); reduced maintenance doses may be effective for patients with significant renal impairment . Few patients with severe renal impairment have been evaluated during chronic treatment with Lamotrigine. Because there is inadequate experience in this population, Lamotrigine should be used with caution in these patients. Patients With Renal ImpairmentTables 1-3Table 5[see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]
: For patients receiving Lamotrigine in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed. Discontinuation StrategyEpilepsy:
If a decision is made to discontinue therapy with Lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation should prolong the half-life of Lamotrigine; discontinuing valproate should shorten the half-life of Lamotrigine.
In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of Lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of Lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of Lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal . Bipolar Disorder:[see Warnings and Precautions (5.9)]
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications ( for patients greater than 12 years of age and for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in . Table 1Table 2Table 3
Recommended dosing guidelines are summarized in . Patients Over 12 Years of Age:Table 1
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine [see Drug Interactions ( 7 ), Clinical Pharmacology ( 12.3 )]. † These drugs induce Lamotrigine glucuronidation and increase clearance Other drugs, that have similar effects include estrogen-containing oral contraceptives Dosing recommendations for oral contraceptives can be found in General Dosing Considerations Patients on rifampin, or other drugs that induce Lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. [see Drug Interactions ( 7 ) Clinical Pharmacology ( 12.3 )]. [see Drug Interactions ( 7 ), Clinical Pharmacology ( 12.3 )]. [see Dosage and Administration ( 2.1 )]. For Patients TAKING Valproate * For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone ,or Valproate †* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone and NOT TAKING Valproate †* Weeks 1 and 2 25 mg every day other 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day (in 2 divided doses) 100 mg/day Weeks 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day every 1 to 2 weeks
Increase by 100 mg/day every 1 to 2 weeks Usual Maintenance Dose (in 1 or 2 divided doses) 100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 2 divided doses) 225 to 375 mg/day
(in 2 divided doses) 300 to 500 mg/dayRecommended dosing guidelines are summarized in . Patients 2 to 12 Years of Age:Table 2
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine [see Drug Interactions ( ), Clinical Pharmacology ( )]. 712.3 † These drugs induce Lamotrigine glucuronidation and increase clearance . Other drugs, that have similar effects include estrogen-containing oral contraceptives . Dosing recommendations for oral contraceptives can be found in General Dosing Considerations Patients on rifampin, or other drugs that induce Lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. [see Drug Interactions ( ) Clinical Pharmacology ( )] 712.3 [see Drug Interactions ( ) Clinical Pharmacology ( )] 712.3
[see Dosage and Administration ( 2.1 )]. For Patients TAKING Valproate * For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone or Valproate
†
* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone and NOT TAKING Valproate †* Weeks 1 and 2 in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.3 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day
Weeks 3 and 4 in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.3 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day
Weeks 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual Maintenance Dose (maximum 200 mg/day in 1 or 2 divided doses). with valproate alone 1 to 5 mg/kg/day1 to 3 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 4.5 to 7.5 mg/kg/day
(maximum 400 mg/day in 2 divided doses) 5 to 15 mg/kg/day
Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response Note: Only whole tablets should be used for dosing. Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every day other 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayThe usual maintenance doses identified in Tables and are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of Lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone , maintenance doses of adjunctive Lamotrigine as high as 700 mg/day have been used. In patients receiving , maintenance doses of adjunctive Lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables has not been established in controlled trials. Usual Adjunctive Maintenance Dose for Epilepsy:12without valproatevalproate alone1 through 4
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with Lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of Lamotrigine.
The recommended maintenance dose of Lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded . [see ] Boxed Warning
After achieving a dose of 500 mg/day of Lamotrigine according to the guidelines in , the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial. Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine:Table 1
The conversion regimen involves 4 steps outlined in . Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine:Table 4
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age with EpilepsyLamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in (if not already on 200 mg/day). Table 1
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
No specific dosing guidelines can be provided for conversion to monotherapy with Lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate. Conversion from Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine:
2.4 Bipolar Disorder
The goal of maintenance treatment with Lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of Lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of Lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin, that increase the apparent clearance of Lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day . Accordingly, doses above 200 mg/day are not recommended. Treatment with Lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in . If other psychotropic medications are withdrawn following stabilization, the dose of Lamotrigine should be adjusted. For patients discontinuing valproate, the dose of Lamotrigine should be doubled over a 2-week period in equal weekly increments (see ). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation, the dose of Lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see ). The dose of Lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated. [see Clinical Studies ( )] 14.2Table 5Table 6Table 6
If other drugs are subsequently introduced, the dose of Lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of Lamotrigine [see Drug Interactions ( ), Clinical Pharmacology ( )] 712.3.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded . [see ] Boxed Warning
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine [see Drug Interactions ( ), Clinical Pharmacology ( )]. 712.3 † These drugs induce Lamotrigine glucuronidation and increase clearance Other drugs that have similar effects include estrogen- containing oral contraceptives . Dosing recommendations for oral contraceptives can be found in General Dosing Considerations . Patients on rifampin, or other drugs that induce Lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/ maintenance regimen as that used with anticonvulsants that have this effect. [see Drug Interactions ( ), Clinical Pharmacology ( )]. 712.3 [see Drug Interactions ( ), Clinical Pharmacology ( )] 712.3
[see Dosage and Administration ( )] 2.1 For Patients TAKING Valproate * For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone , or Valproate †* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone and NOT TAKING Valproate †* Weeks 1 and 2 25 mg every day other 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications * These drugs induce Lamotrigine glucuronidation and increase clearance Other drugs that have similar effects include estrogen-containing oral contraceptives . Dosing recommendations for oral contraceptives can be found in General Dosing Considerations . Patients on rifampin, or other drugs that induce Lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/ maintenance regimen as that used with anticonvulsants that have this effect. [see Drug Interactions ( ), Clinical Pharmacology ( )]. 712.3 [see Drug Interactions ( ), Clinical Pharmacology ( )] 712.3 [see Dosage and Administration ( )] 2.1 † Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine [see Drug Interactions ( ), Clinical Pharmacology ( )]. 712.3Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone , or Valproate ) *†
After Discontinuation of Valproate † After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone * Current dose of Lamotrigine (mg/day) 100Current dose of Lamotrigine (mg/day) 400
Week 1 Maintain current dose of Lamotrigine 150 400 Week 2 Maintain current dose of Lamotrigine 200 300 Week 3 onward Maintain current dose of Lamotrigine 200 200The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with Lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials . However, the optimal duration of treatment with Lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment. [see Clinical Studies ( )] 14.2
-
Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ] Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Dosing is based on concomitant medications, indication, and patient age. ( 2.2 , 2.4 ) To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations should not be exceeded. ( 2.1 ) Do not restart lamotrigine in patients who discontinued due to rash unless the potential benefits clearly outweigh the risks. ( 2.1 ) Adjustments to maintenance doses will in most cases be required in patients starting or stopping estrogen-containing oral contraceptives. ( 2.1 , 5.8 ) Lamotrigine tablets should be discontinued over a period of at least 2 weeks (approximately 50% reduction per week). ( 2.1 , 5.9 )Epilepsy
Adjunctive therapy—See Table 1 for patients >12 years of age and Tables 2 and 3 for patients 2 to 12 years. ( 2.2 ) Conversion to monotherapy—See Table 4. ( 2.3 )Bipolar Disorder: See Tables 5 and 6 ( 2.4 )
Rash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning ]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablet is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3) ].
Lamotrigine Tablets Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3) ] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3) ].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3) ], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3) ].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3) ]. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6) , Clinical Pharmacology (12.3) ], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7) , Clinical Pharmacology (12.3) ]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.
Discontinuation Strategy:
Epilepsy: For patients receiving lamotrigine tablets in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9) ].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9) ].
This section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine Tablets in Patients Over 12 Years of Age With Epilepsy
For
For Patients NOT TAKING
For Patients
Patients
Carbamazepine,
TAKING
TAKING
Phenytoin,
Carbamazepine,
Valproatea
Phenobarbital,
Phenytoin,
or Primidoneb,
Phenobarbital,
or Valproatea
or Primidoneb
and NOT TAKING
Valproatea
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Weeks 5 onwards to
maintenance
Increase by 25 to
50 mg/day every 1 to 2 weeks
Increase by 50
mg/day every 1
to 2 weeks
Increase by
100 mg/day every
1 to 2 weeks.
Usual maintenance
dose
100 to 200 mg/day
with valproate alone
225 to 375 mg/day
(in 2 divided doses).
300 to 500 mg/day
(in 2 divided doses).
100 to 400 mg/day
with valproate
and other drugs that induce glucuronidation
(in 1 or 2 divided doses)
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Patients 2 to 12 Years Of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine Tablets in Patients 2 to 12 Years of Age With Epilepsy
For Patients TAKING
Valproatea
For Patients NOT
TAKING Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea
For Patients TAKING
Carbamazepine, Phenytoin, Phenobarbital, or
Primidoneb and NOT
TAKING Valproatea
Weeks 1 and 2
0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the
nearest whole tablet (see Table 3 for weight
based dosing guide).
0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the
nearest whole tablet.
0.6 mg/kg/day
in 2 divided doses, rounded down to the
nearest whole tablet.
Weeks 3 and 4
0.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
(see Table 3 for weight
based dosing guide).
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet.
1.2 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet.
Weeks 5
onwards to
maintenance
The dose should be increased every
1 to 2 weeks as follows:
calculate 0.3 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose.
The dose should be increased every
1 to 2 weeks as follows:
calculate 0.6 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose
The dose should be increased every
1 to 2 weeks as follows:
calculate 1.2 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose
Usual
Maintenance
Dose
1 to 5 mg/kg/day
(maximum 200 mg/day
in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone
4.5 to 7.5 mg/kg/day
(maximum 300 mg/day
in 2 divided doses)
5 to 15 mg/kg/day
(maximum 400 mg/day
in 2 divided doses)
Maintenance dose in
patients
less than 30 kg
May need to be increased
by as much as 50%,
based on clinical response
May need to be increased
by as much as 50%,
based on clinical response
May need to be increased
by as much as 50%, based
on clinical response
Note: Only whole tablets should be used for dosing.
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is
Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
The goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in two divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets: After achieving a dose of 500 mg/day of lamotrigine tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets:
The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets in Patients ≥16 Years of Age with Epilepsy
Lamotrigine Tablets
Valproate
Step 1
Achieve a dose of 200 mg/day according to
guidelines in Table 1
(if not already on 200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than
500 mg/day/week and then maintain the dose of
500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to
250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every
week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
The goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2) ]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7) , Clinical Pharmacology (12.3) ].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning ].
Table 5. Escalation Regimen for Lamotrigine Tablets for Patients With Bipolar Disorder
For Patients TAKING
Valproatea
For Patients NOT TAKING
Carbamazepine, Phenytoin, Phenobarbital,
Primidoneb, or Valproatea
For Patients TAKING
Carbamazepine, Phenytoin,
Phenobarbital, or Primidoneb and NOT TAKING
Valproatea
Weeks 1 and 2
25 mg every
other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 6. Dosage Adjustments to Lamotrigine Tablets for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications
Discontinuation of Psychotropic Drugs
(excluding Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea)
After Discontinuation of
Valproatea
After Discontinuation of
Carbamazepine, Phenytoin,
Phenobarbital, or Primidoneb
Current dose of lamotrigine tablets
(mg/day)
100
Current dose of lamotrigine tablets
(mg/day)
400
Week 1
Maintain current dose of lamotrigine tablets
150
400
Week 2
Maintain current dose of lamotrigine tablets
200
300
Week 3 onward
Maintain current dose of lamotrigine tablets
200
200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine tablets was established in two randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2) ]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Mckesson Packaging Sevices A Business Unit Of Mckesson Corporation
![Lamotrigine Tablet [Mckesson Packaging Sevices A Business Unit Of Mckesson Corporation]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Mckesson Packaging Sevices A Business Unit Of Mckesson Corporation
![Lamotrigine Tablet [Mckesson Packaging Sevices A Business Unit Of Mckesson Corporation] Lamotrigine Tablet [Mckesson Packaging Sevices A Business Unit Of Mckesson Corporation]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash
There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see BOXED WARNING]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see CLINICAL PHARMACOLOGY (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation
Drugs other than those listed in the Clinical Pharmacology section [see CLINICAL PHARMACOLOGY (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients with Epilepsy or Bipolar Disorder
A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response [see CLINICAL PHARMACOLOGY (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives
Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives
Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see CLINICAL PHARMACOLOGY (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives
(1) Taking Estrogen-Containing Oral Contraceptives
For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see DRUG INTERACTIONS (7), CLINICAL PHARMACOLOGY (12.3)], the maintenance dose of lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see CLINICAL PHARMACOLOGY (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives
In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see DRUG INTERACTIONS (7), CLINICAL PHARMACOLOGY (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see DRUG INTERACTIONS (7), CLINICAL PHARMACOLOGY (12.3)], no adjustment to the dose of lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives
For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see DRUG INTERACTIONS (7), CLINICAL PHARMACOLOGY (12.3)], the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see CLINICAL PHARMACOLOGY (12.3)]. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see DRUG INTERACTIONS (7), CLINICAL PHARMACOLOGY (12.3)], no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy
The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients with Hepatic Impairment
Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see USE IN SPECIFIC POPULATIONS (8.6), CLINICAL PHARMACOLOGY (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients with Renal Impairment
Initial doses of lamotrigine should be based on patients' concomitant medications (see Tables 1 to 3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see USE IN SPECIFIC POPULATIONS (8.6), CLINICAL PHARMACOLOGY (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy
Epilepsy
For patients receiving lamotrigine in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see WARNINGS AND PRECAUTIONS (5.10)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder
In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see WARNINGS AND PRECAUTIONS (5.10)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age
Recommended dosing guidelines are summarized in Table 1.
Table 1 Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy For Patients Taking Valproate*
For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate*
For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate*
* Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see DRUG INTERACTIONS ( 7), CLINICAL PHARMACOLOGY ( 12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [see DRUG INTERACTIONS ( 7), CLINICAL PHARMACOLOGY ( 12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see DRUG INTERACTIONS ( 7), CLINICAL PHARMACOLOGY ( 12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see DOSAGE AND ADMINISTRATION ( 2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)Week 5 onwards to maintenance
Increase by 25 to 50 mg/day every 1 to 2 weeks
Increase by 50 mg/day every 1 to 2 weeks
Increase by 100 mg/day every 1 to 2 weeks.
Usual Maintenance Dose
100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses)225 to 375 mg/day
(in 2 divided doses)300 to 500 mg/day
(in 2 divided doses)Patients 2 to 12 Years of Age
Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2 Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy For Patients TAKING Valproatea
For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb, or Valproatea
For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea
Note: Only whole tablets should be used for dosing. *Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see DRUG INTERACTIONS (7), Pharmacokinetics (12.3)]. bThese drugs induce lamotrigine glucuronidation and increase clearance [see DRUG INTERACTIONS (7), CLINICAL PHARMACOLOGY (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see DRUG INTERACTIONS (7), CLINICAL PHARMACOLOGY (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see DOSAGE AND ADMINISTRATION (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.Weeks 1 and 2
0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest
whole tablet (see Table 3 for weight based dosing guide)0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tabletWeeks 3 and 4
0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest
whole tablet (see Table 3 for weight based dosing guide)0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tabletWeeks 5 onwards to maintenance
The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
Usual Maintenance Dose
1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses)
1 to 3 mg/kg/day with valproate alone4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses)5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses)
Maintenance dose in patients less than 30 kg
May need to be increased by as much as 50%,
based on clinical responseMay need to be increased by as much as 50%,
based on clinical responseMay need to be increased by as much as 50%,
Table 3 The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy
based on clinical responseIf the patient’s weight is
Give this daily dose, using the most appropriate combination of Lamotrigine 5 mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy
The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion from Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see BOXED WARNING].
Conversion from Adjunctive Therapy with Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy with Lamotrigine
After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy with Valproate to Monotherapy with Lamotrigine
The conversion regimen involves 4 steps outlined in Table 4.
Table 4 Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age With EpilepsyLamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to
guidelines in Table 1 (if not already on 200 mg/day).Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and
then maintain the dose of 500 mg/day for 1 week.Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy with AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy with Lamotrigine
No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see DRUG INTERACTIONS (7), CLINICAL PHARMACOLOGY (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see BOXED WARNING].
Table 5 Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see DRUG INTERACTIONS ( 7), CLINICAL PHARMACOLOGY ( 12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [see DRUG INTERACTIONS (7), CLINICAL PHARMACOLOGY ( 12.3)]. Other drugs which have similar effects include estrogen containing oral contraceptives [see DRUG INTERACTIONS (7), CLINICAL PHARMACOLOGY ( 12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see DOSAGE AND ADMINISTRATION ( 2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.For Patients TAKING Valproate*
For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate*
For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate*
Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
Table 6 Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications * These drugs induce lamotrigine glucuronidation and increase clearance [see DRUG INTERACTIONS ( 7), CLINICAL PHARMACOLOGY ( 12.3)]. Other drugs which have similar effects include estrogen containing oral contraceptives [see DRUG INTERACTIONS ( 7), CLINICAL PHARMACOLOGY ( 12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see DOSAGE AND ADMINISTRATION ( 2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. † Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see DRUG INTERACTIONS ( 7), CLINICAL PHARMACOLOGY ( 12.3)].Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone*, or Valproate†)
After Discontinuation of Valproate†
After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone*
Current dose of Lamotrigine (mg/day)
100Current dose of Lamotrigine (mg/day)
400Week 1
Maintain current dose of Lamotrigine
150
400
Week 2
Maintain current dose of Lamotrigine
200
300
Week 3 onward
Maintain current dose of Lamotrigine
200
200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
2.5 Administration of Lamotrigine Tablets (Chewable, Dispersible)Lamotrigine Tablets (Chewable, Dispersible) may be swallowed whole, chewed, or dispersed in water or diluted fruit juice. If the tablets are chewed, consume a small amount of water or diluted fruit juice to aid in swallowing.
To disperse Lamotrigine Tablets (Chewable, Dispersible), add the tablets to a small amount of liquid (1 teaspoon, or enough to cover the medication). Approximately 1 minute later, when the tablets are completely dispersed, swirl the solution and consume the entire quantity immediately. No attempt should be made to administer partial quantities of the dispersed tablets.
-
Jubilant Cadista Pharmaceuticals Inc.
![Lamotrigine (Lamotrigine) Tablet, Chewable [Jubilant Cadista Pharmaceuticals Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Jubilant Cadista Pharmaceuticals Inc.
![Lamotrigine (Lamotrigine) Tablet, Chewable [Jubilant Cadista Pharmaceuticals Inc.] Lamotrigine (Lamotrigine) Tablet, Chewable [Jubilant Cadista Pharmaceuticals Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy - Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy
For Patients TAKING Valproate *
For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone† , or Valproate*
For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate*
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Week 5 onwards to maintenance
Increase by 25 to 50 mg/day every 1 to 2 weeks
Increase by 50 mg/day every 1 to 2 weeks
Increase by 100 mg/day every 1 to 2 weeks.
Usual maintenance dose
100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses)
225 to 375 mg/day
(in 2 divided doses)
300 to 500 mg/day
(in 2 divided doses)
* Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
† These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
The smallest available strength of lamotrigine tablets (chewable, dispersible) is 2 mg, and only whole tablets should be administered. If the calculated dose cannot be achieved using whole tablets, the dose should be rounded down to the nearest whole tablet [see How Supplied/Storage and Handling (16) and Medication Guide].
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy
For Patients TAKING Valproate *
For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone† , or Valproate*
For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate*
Weeks 1 and 2
0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide)
0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet
0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet
Weeks 3 and 4
0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide)
0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet
1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet
Week 5 onwards to maintenance
The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
Usual maintenance dose
1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses)
1 to 3 mg/kg/day with valproate alone4.5 to 7.5 mg/kg/day (maximum 300 mg/day in 2 divided doses)
5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses)
Maintenance dose in patients less than 30 kg
May need to be increased by as much as 50%, based on clinical response
May need to be increased by as much as 50%, based on clinical response
May need to be increased by as much as 50%, based on clinical response
Note: Only whole tablets should be used for dosing.
* Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
† These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years of Age Taking Valproate (Weeks 1 to 4) With Epilepsy
If the patient’s weight is
Give this daily dose, using the most appropriate combination of lamotrigine 2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age With Epilepsy
Lamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion From Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder
For Patients TAKING Valproate‡
For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone† or Valproate‡
For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital or Primidone † and NOT TAKING Valproate‡
Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
‡ Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
† These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications
Discontinuation of Psychotropic Drugs (excluding Carbamazepine,
Phenytoin, Phenobarbital, Primidone, or Valproate‡)After Discontinuation of Valproate‡
After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital,or Primidone†
Current dose of Lamotrigine
(mg/day) 100Current dose of Lamotrigine
(mg/day) 400Week 1
Maintain current dose of Lamotrigine
150
400
Week 2
Maintain current dose of Lamotrigine
200
300
Week 3 onward
Maintain current dose of Lamotrigine
200
200
‡ Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
† These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2 )]. However, the optimal duration of treatment with lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
2.5 Administration of Lamotrigine Tablets (Chewable, Dispersible)Lamotrigine tablets (chewable, dispersible) may be swallowed whole, chewed, or dispersed in water or diluted fruit juice. If the tablets are chewed, consume a small amount of water or diluted fruit juice to aid in swallowing.
To disperse lamotrigine tablets (chewable, dispersible), add the tablets to a small amount of liquid (1 teaspoon, or enough to cover the medication). Approximately 1 minute later, when the tablets are completely dispersed, swirl the solution and consume the entire quantity immediately. No attempt should be made to administer partial quantities of the dispersed tablets.
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving lamotrigine in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy - Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy
For Patients TAKING Valproate *
For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone† , or Valproate*
For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate*
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Week 5 onwards to maintenance
Increase by 25 to 50 mg/day every 1 to 2 weeks
Increase by 50 mg/day every 1 to 2 weeks
Increase by 100 mg/day every 1 to 2 weeks.
Usual maintenance dose
100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses)
225 to 375 mg/day
(in 2 divided doses)
300 to 500 mg/day
(in 2 divided doses)
* Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
† These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
The smallest available strength of lamotrigine tablets (chewable, dispersible) is 2 mg, and only whole tablets should be administered. If the calculated dose cannot be achieved using whole tablets, the dose should be rounded down to the nearest whole tablet [see How Supplied/Storage and Handling (16) and Medication Guide].
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy
For Patients TAKING Valproate *
For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone† , or Valproate*
For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate*
Weeks 1 and 2
0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide)
0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet
0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet
Weeks 3 and 4
0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide)
0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet
1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet
Week 5 onwards to maintenance
The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
Usual maintenance dose
1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses)
1 to 3 mg/kg/day with valproate alone4.5 to 7.5 mg/kg/day (maximum 300 mg/day in 2 divided doses)
5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses)
Maintenance dose in patients less than 30 kg
May need to be increased by as much as 50%, based on clinical response
May need to be increased by as much as 50%, based on clinical response
May need to be increased by as much as 50%, based on clinical response
Note: Only whole tablets should be used for dosing.
* Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
† These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years of Age Taking Valproate (Weeks 1 to 4) With Epilepsy
If the patient’s weight is
Give this daily dose, using the most appropriate combination of lamotrigine 2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age With Epilepsy
Lamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion From Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. For patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder
For Patients TAKING Valproate‡
For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone† or Valproate‡
For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital or Primidone † and NOT TAKING Valproate‡
Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
‡ Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
† These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications
Discontinuation of Psychotropic Drugs (excluding Carbamazepine,
Phenytoin, Phenobarbital, Primidone, or Valproate‡)After Discontinuation of Valproate‡
After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital,or Primidone†
Current dose of Lamotrigine
(mg/day) 100Current dose of Lamotrigine
(mg/day) 400Week 1
Maintain current dose of Lamotrigine
150
400
Week 2
Maintain current dose of Lamotrigine
200
300
Week 3 onward
Maintain current dose of Lamotrigine
200
200
‡ Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
† These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2 )]. However, the optimal duration of treatment with lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
2.5 Administration of Lamotrigine Tablets (Chewable, Dispersible)Lamotrigine tablets (chewable, dispersible) may be swallowed whole, chewed, or dispersed in water or diluted fruit juice. If the tablets are chewed, consume a small amount of water or diluted fruit juice to aid in swallowing.
To disperse lamotrigine tablets (chewable, dispersible), add the tablets to a small amount of liquid (1 teaspoon, or enough to cover the medication). Approximately 1 minute later, when the tablets are completely dispersed, swirl the solution and consume the entire quantity immediately. No attempt should be made to administer partial quantities of the dispersed tablets.
-
Bryant Ranch Prepack
![Lamotrigine (Lamotrigine) Tablet [Bryant Ranch Prepack]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Bryant Ranch Prepack
![Lamotrigine (Lamotrigine) Tablet [Bryant Ranch Prepack] Lamotrigine (Lamotrigine) Tablet [Bryant Ranch Prepack]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of Lamotrigine with valproate, (2) exceeding the recommended initial dose of Lamotrigine, or (3) exceeding the recommended dose escalation for Lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of Lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that Lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with Lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued Lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued Lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of Lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with Lamotrigine. Because Lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of Lamotrigine and doses of Lamotrigine may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for Lamotrigine. Dosing of Lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of Lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for Lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with Lamotrigine based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of Lamotrigine in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of Lamotrigine will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent Lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of Lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent Lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless Lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in Lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased Lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to Lamotrigine consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of Lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of Lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent Lamotrigine plasma level. The decrease in dose of Lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or Lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of Lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of Lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of Lamotrigine up to 2-fold, and the progestin-only pills had no effect on Lamotrigine plasma levels. Therefore, adjustments to the dosage of Lamotrigine in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of Lamotrigine should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with Lamotrigine. Because there is inadequate experience in this population, Lamotrigine should be used with caution in these patients.
Discontinuation Strategy: Epilepsy: For patients receiving Lamotrigine in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse experiences is observed.
If a decision is made to discontinue therapy with Lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation should prolong the half-life of Lamotrigine; discontinuing valproate should shorten the half-life of Lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of Lamotrigine. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of Lamotrigine. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of Lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine [see Drug Interactions ( 7 ), Clinical Pharmacology ( 12.3 )]. † These drugs induce Lamotrigine glucuronidation and increase clearance [see Drug Interactions ( 7 ) Clinical Pharmacology ( 12.3 )]. Other drugs, which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions ( 7 ), Clinical Pharmacology ( 12.3 )]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration ( 2.1 )]. Patients on rifampin, or other drugs that induce Lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†,or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day (in 2 divided doses) Weeks 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day
every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks Usual Maintenance Dose 100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronication
(in 1 or 2 divided doses) 225 to 375 mg/day
(in 2 divided doses) 300 to 500 mg/day (in 2 divided doses)Patients 2 to 12 Years of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine [see Drug Interactions (7 ), Clinical Pharmacology (12.3)]. † These drugs induce Lamotrigine glucuronidation and increase clearance [see Drug Interactions (7 ) Clinical Pharmacology (12.3)]. Other drugs, which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7 ) Clinical Pharmacology (12.3)].
Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce Lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine,
Phenytoin,
Phenobarbital,
Primidone† or
Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Weeks 1 and 2 0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide) 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual Maintenance Dose 1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day
(maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response Note: Only whole tablets should be used for dosing. Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of Lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive Lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive Lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with Lamotrigine under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of Lamotrigine.
The recommended maintenance dose of Lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine: After achieving a dose of 500 mg/day of Lamotrigine according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine: The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥16 Years of Age with EpilepsyLamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
2.4 Bipolar Disorder
Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine: No specific dosing guidelines can be provided for conversion to monotherapy with Lamotrigine with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.The goal of maintenance treatment with Lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of Lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of Lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin, that increase the apparent clearance of Lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with Lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of Lamotrigine should be adjusted. For patients discontinuing valproate, the dose of Lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce Lamotrigine glucuronidation, the dose of Lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of Lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of Lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of Lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine [see Drug Interactions (7 ), Clinical Pharmacology (12.3)]. † These drugs induce Lamotrigine glucuronidation and increase clearance [see Drug Interactions (7 ), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen- containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)].
Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce Lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/ maintenance regimen as that used with anticonvulsants that have this effect. For Patients TAKING Valproate* For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications * These drugs induce Lamotrigine glucuronidation and increase clearance [see Drug Interactions (7 ), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce Lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/ maintenance regimen as that used with anticonvulsants that have this effect. † Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of Lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone*, or Valproate†)
After Discontinuation of Valproate† After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone* Current dose of Lamotrigine (mg/day) 100Current dose of Lamotrigine (mg/day) 400
Week 1 Maintain current dose of Lamotrigine 150 400 Week 2 Maintain current dose of Lamotrigine 200 300 Week 3 onward Maintain current dose of Lamotrigine 200 200The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with Lamotrigine was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with Lamotrigine has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Upsher-smith Laboratories, Inc.
-
Mylan Institutional Inc.
![Lamotrigine Tablet [Mylan Institutional Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Mylan Institutional Inc.
![Lamotrigine Tablet [Mylan Institutional Inc.] Lamotrigine Tablet [Mylan Institutional Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing Considerations RashThere are suggestions, yet to be proven, that the risk of severe, potentially life threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablets are exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Tablets Added to Drugs Known to Induce or Inhibit GlucuronidationDrugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets may require adjustment based on clinical response.
Target Plasma Levels for Patients with Epilepsy or Bipolar DisorderA therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women taking Estrogen-Containing Oral Contraceptives Starting Lamotrigine Tablets in Women taking Estrogen-Containing Oral ContraceptivesAlthough estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets in Women taking Estrogen-Containing Oral Contraceptives(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement TherapyThe effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.
Patients with Hepatic ImpairmentExperience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients with Renal ImpairmentInitial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1 to 3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.
Discontinuation Strategy EpilepsyFor patients receiving lamotrigine tablets in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.10)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar DisorderIn the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with bipolar disorder, two patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.10)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of AgeRecommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine Tablets in Patients Over 12 Years of Age with Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.For Patients TAKING
Valproate*For Patients NOT
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital,
Primidone† or
Valproate*For Patients
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital or
Primidone† and
NOT
TAKING
Valproate*Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)Week 5 onwards
to maintenanceIncrease by 25 to 50 mg/day every 1 to 2 weeks
Increase by 50 mg/day every 1 to 2 weeks
Increase by 100 mg/day every 1 to 2 weeks
Usual Maintenance
Dose100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses)225 to 375 mg/day
(in 2 divided doses)300 to 500 mg/day
Patients 2 to 12 Years of Age
(in 2 divided doses)Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine Tablets in Patients 2 to 12 Years of Age with Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.For Patients TAKING
Valproate*
For Patients NOT
TAKING
Carbamazepine,
Phenytoin, Phenobarbital, Primidone† or Valproate*For Patients TAKING
Carbamazepine,
Phenytoin,
Phenobarbital or
Primidone† and NOT
TAKING Valproate*Weeks
1 and 20.15 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet (see
Table 3 for weight based
dosing guide).0.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet.0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet.Weeks
3 and 40.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
(see Table 3 for weight
based dosing guide).0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet.1.2 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet.Week 5
onwards tomaintenance
The dose should be
increased every 1 to
2 weeks as follows:
calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet
and add this
amount to the previously
administered daily dose.The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day,
round this amount down to the nearest whole tablet and add this amount to the previously administered daily dose.
The dose should be
increased every 1 to 2 weeks as follows:
calculate
1.2 mg/kg/day, round this amount
down to the nearest
whole tablet and
add this amount to
the previously
administered daily
dose.Usual
Maintenance
Dose
1 to 5 mg/kg/day
(maximum 200 mg/day in
1 or 2 divided doses).
1 to 3 mg/kg/day with
valproate alone.4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses).5 to 15 mg/kg/day
(maximum 400 mg/day in 2 divided doses).Maintenance
dose in
patients less
than 30 kg
May need to be increased
by as much as 50%, based
on clinical response.May need to be increased by as much as 50%, based on clinical response.
May need to be
increased by as
much as 50%, based
on clinical response.Note: Only whole tablets should be used for dosing.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years of Age taking Valproate (Weeks 1 to 4) with EpilepsyIf the patient's weight is
Give this daily dose, using the most appropriate combination of lamotrigine 2 mg and 5 mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for EpilepsyThe usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion from Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in two divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion from Adjunctive Therapy with Carbamazepine, Phenytoin, Phenobarbital or Primidone to Monotherapy with Lamotrigine TabletsAfter achieving a dose of 500 mg/day of lamotrigine tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy with Valproate to Monotherapy with Lamotrigine TabletsThe conversion regimen involves four steps outlined in Table 4.
Table 4. Conversion from Adjunctive Therapy with Valproate to Monotherapy with Lamotrigine Tablets in Patients ≥ 16 Years of Age with EpilepsyLamotrigine Tablets
Valproate
Step 1
Achieve a dose of 200 mg/day according to
guidelines in Table 1 (if not already on200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by
decrements no greater than
500 mg/day/week and then
maintain the dose of
500 mg/day for one week.Step 3
Increase to 300 mg/day and maintain
for one week.Simultaneously decrease to
250 mg/day and maintain for
one week.Step 4
Increase by 100 mg/day every week to achieve
maintenance dose of 500 mg/day.Discontinue.
Conversion from Adjunctive Therapy with Antiepileptic Drugs Other than Carbamazepine, Phenytoin, Phenobarbital, Primidone or Valproate to Monotherapy with Lamotrigine TabletsNo specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine Tablets for Patients with Bipolar Disorder * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.For Patients
TAKING
Valproate*For Patients NOT
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital,
Primidone† or
Valproate*For Patients
TAKING
Carbamazepine,
Phenytoin, Phenobarbital or
Primidone† and
NOT TAKING
Valproate*Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
Table 6. Dosage Adjustments to Lamotrigine Tablets for Patients with Bipolar Disorder Following Discontinuation of Psychotropic Medications * These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. † Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].Discontinuation of
Psychotropic Drugs
(excluding Carbamazepine,
Phenytoin, Phenobarbital,
Primidone*
or Valproate†)After
Discontinuation
of Valproate†After Discontinuation
of Carbamazepine,
Phenytoin,
Phenobarbital or
Primidone*Current dose of lamotrigine tablets (mg/day)
100Current dose of lamotrigine tablets (mg/day)
400Week 1
Maintain current dose of lamotrigine tablets
150
400
Week 2
Maintain current dose of lamotrigine tablets
200
300
Week 3 onward
Maintain current dose of lamotrigine tablets
200
200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine tablets was established in two randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ] Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Dosing is based on concomitant medications, indication, and patient age. ( 2.2 , 2.4 ) To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations should not be exceeded. ( 2.1 ) Do not restart lamotrigine in patients who discontinued due to rash unless the potential benefits clearly outweigh the risks. ( 2.1 ) Adjustments to maintenance doses will in most cases be required in patients starting or stopping estrogen-containing oral contraceptives. ( 2.1 , 5.8 ) Lamotrigine tablets should be discontinued over a period of at least 2 weeks (approximately 50% reduction per week). ( 2.1 , 5.9 )Epilepsy
Adjunctive therapy—See Table 1 for patients >12 years of age and Tables 2 and 3 for patients 2 to 12 years. ( 2.2 ) Conversion to monotherapy—See Table 4. ( 2.3 )Bipolar Disorder: See Tables 5 and 6 ( 2.4 )
Rash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning ]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablet is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3) ].
Lamotrigine Tablets Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3) ] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3) ].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3) ], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3) ].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3) ]. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6) , Clinical Pharmacology (12.3) ], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7) , Clinical Pharmacology (12.3) ]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.
Discontinuation Strategy:
Epilepsy: For patients receiving lamotrigine tablets in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9) ].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9) ].
This section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine Tablets in Patients Over 12 Years of Age With Epilepsy
For
For Patients NOT TAKING
For Patients
Patients
Carbamazepine,
TAKING
TAKING
Phenytoin,
Carbamazepine,
Valproatea
Phenobarbital,
Phenytoin,
or Primidoneb,
Phenobarbital,
or Valproatea
or Primidoneb
and NOT TAKING
Valproatea
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Weeks 5 onwards to
maintenance
Increase by 25 to
50 mg/day every 1 to 2 weeks
Increase by 50
mg/day every 1
to 2 weeks
Increase by
100 mg/day every
1 to 2 weeks.
Usual maintenance
dose
100 to 200 mg/day
with valproate alone
225 to 375 mg/day
(in 2 divided doses).
300 to 500 mg/day
(in 2 divided doses).
100 to 400 mg/day
with valproate
and other drugs that induce glucuronidation
(in 1 or 2 divided doses)
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Patients 2 to 12 Years Of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine Tablets in Patients 2 to 12 Years of Age With Epilepsy
For Patients TAKING
Valproatea
For Patients NOT
TAKING Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea
For Patients TAKING
Carbamazepine, Phenytoin, Phenobarbital, or
Primidoneb and NOT
TAKING Valproatea
Weeks 1 and 2
0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the
nearest whole tablet (see Table 3 for weight
based dosing guide).
0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the
nearest whole tablet.
0.6 mg/kg/day
in 2 divided doses, rounded down to the
nearest whole tablet.
Weeks 3 and 4
0.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
(see Table 3 for weight
based dosing guide).
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet.
1.2 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet.
Weeks 5
onwards to
maintenance
The dose should be increased every
1 to 2 weeks as follows:
calculate 0.3 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose.
The dose should be increased every
1 to 2 weeks as follows:
calculate 0.6 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose
The dose should be increased every
1 to 2 weeks as follows:
calculate 1.2 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose
Usual
Maintenance
Dose
1 to 5 mg/kg/day
(maximum 200 mg/day
in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone
4.5 to 7.5 mg/kg/day
(maximum 300 mg/day
in 2 divided doses)
5 to 15 mg/kg/day
(maximum 400 mg/day
in 2 divided doses)
Maintenance dose in
patients
less than 30 kg
May need to be increased
by as much as 50%,
based on clinical response
May need to be increased
by as much as 50%,
based on clinical response
May need to be increased
by as much as 50%, based
on clinical response
Note: Only whole tablets should be used for dosing.
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is
Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
The goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in two divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets: After achieving a dose of 500 mg/day of lamotrigine tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets:
The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets in Patients ≥16 Years of Age with Epilepsy
Lamotrigine Tablets
Valproate
Step 1
Achieve a dose of 200 mg/day according to
guidelines in Table 1
(if not already on 200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than
500 mg/day/week and then maintain the dose of
500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to
250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every
week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
The goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2) ]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7) , Clinical Pharmacology (12.3) ].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning ].
Table 5. Escalation Regimen for Lamotrigine Tablets for Patients With Bipolar Disorder
For Patients TAKING
Valproatea
For Patients NOT TAKING
Carbamazepine, Phenytoin, Phenobarbital,
Primidoneb, or Valproatea
For Patients TAKING
Carbamazepine, Phenytoin,
Phenobarbital, or Primidoneb and NOT TAKING
Valproatea
Weeks 1 and 2
25 mg every
other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 6. Dosage Adjustments to Lamotrigine Tablets for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications
Discontinuation of Psychotropic Drugs
(excluding Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea)
After Discontinuation of
Valproatea
After Discontinuation of
Carbamazepine, Phenytoin,
Phenobarbital, or Primidoneb
Current dose of lamotrigine tablets
(mg/day)
100
Current dose of lamotrigine tablets
(mg/day)
400
Week 1
Maintain current dose of lamotrigine tablets
150
400
Week 2
Maintain current dose of lamotrigine tablets
200
300
Week 3 onward
Maintain current dose of lamotrigine tablets
200
200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine tablets was established in two randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2) ]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Zydus Pharmaceuticals (Usa) Inc.
![Lamotrigine Tablet Lamotrigine Tablet, Chewable [Zydus Pharmaceuticals (Usa) Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | X-gen Pharmaceuticals, Inc.
![Lamotrigine Tablet Lamotrigine Tablet, Chewable [Zydus Pharmaceuticals (Usa) Inc.] Lamotrigine Tablet Lamotrigine Tablet, Chewable [Zydus Pharmaceuticals (Usa) Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Dosage
2.1 DosagePANCRELIPASE is not interchangeable with other pancrelipase products other than ZENPEP ®.
PANCRELIPASE is orally administered. Therapy should be initiated at the lowest recommended dose and gradually increased. The dosage of PANCRELIPASE should be individualized based on clinical symptoms, the degree of steatorrhea present, and the fat content of the diet (see Limitations on Dosing below).
Dosage recommendations for pancreatic enzyme replacement therapy were published following the Cystic Fibrosis Foundation Consensus Conferences. 1, 2, 3 PANCRELIPASE should be administered in a manner consistent with the recommendations of the Conferences provided in the following paragraphs. Patients may be dosed on a fat ingestion based or actual body weight based dosing scheme.
Infants (up to 12 months) Infants may be given 3,000 lipase units (one capsule) per 120 mL of formula or per breast-feeding. Do not mix PANCRELIPASE capsule contents directly into formula or breast milk prior to administration [see Dosage and Administration (2.2)].
Children Older than 12 Months and Younger than 4 Years Enzyme dosing should begin with 1,000 lipase units/kg of body weight per meal for children less than age 4 years to a maximum of 2,500 lipase units/kg of body weight per meal (or less than or equal to 10,000 lipase units/kg of body weight per day), or less than 4,000 lipase units/g fat ingested per day.
Children 4 Years and Older and Adults Enzyme dosing should begin with 500 lipase units/kg of body weight per meal for those older than age 4 years to a maximum of 2,500 lipase units/kg of body weight per meal (or less than or equal to 10,000 lipase units/kg of body weight per day), or less than 4,000 lipase units/g fat ingested per day.
Usually, half of the prescribed PANCRELIPASE dose for an individualized full meal should be given with each snack. The total daily dose should reflect approximately three meals plus two or three snacks per day.
Enzyme doses expressed as lipase units/kg of body weight per meal should be decreased in older patients because they weigh more but tend to ingest less fat per kilogram of body weight.
Limitations on Dosing Dosing should not exceed the recommended maximum dosage set forth by the Cystic Fibrosis Foundation Consensus Conferences Guidelines. 1, 2, 3
If symptoms and signs of steatorrhea persist, the dosage may be increased by a healthcare professional. Patients should be instructed not to increase the dosage on their own. There is great inter individual variation in response to enzymes; thus, a range of doses is recommended. Changes in dosage may require an adjustment period of several days. If doses are to exceed 2,500 lipase units/kg of body weight per meal, further investigation is warranted.
Doses greater than 2,500 lipase units/kg of body weight per meal (or greater than 10,000 lipase units/kg of body weight per day) should be used with caution and only if they are documented to be effective by 3-day fecal fat measures that indicate a significantly improved coefficient of fat absorption. Doses greater than 6,000 lipase units/kg of body weight per meal have been associated with colonic strictures, indicative of fibrosing colonopathy, in children with cystic fibrosis less than 12 years of age [see Warnings and Precautions (5.1)]. Patients currently receiving higher doses than 6,000 lipase units/kg of body weight per meal should be examined and the dosage either immediately decreased or titrated downward to a lower range.
2.2 AdministrationPANCRELIPASE should always be taken as prescribed by a healthcare professional.
Infants (up to 12 Months) PANCRELIPASE should be administered to infants immediately prior to each feeding, using a dosage of 2,000 to 4,000 lipase units per 120 mL of formula or per breast-feeding. Contents of the capsule may be administered with a small amount of applesauce, or other acidic food with a pH of 4.5 or less (e.g., commercially available preparations of bananas, or pears). Contents of the capsule may also be administered directly to the mouth. Administration should be followed by breast milk or formula. Contents of the capsule should not be mixed directly into formula or breast milk as this may diminish efficacy. Care should be taken to ensure that PANCRELIPASE is not crushed or chewed or retained in the mouth, to avoid irritation of the oral mucosa.
Children and Adults PANCRELIPASE should be taken during meals or snacks, with sufficient fluid. PANCRELIPASE capsules and capsule contents should not be crushed or chewed. Capsules should be swallowed whole.
For patients who are unable to swallow intact capsules, the capsules may be carefully opened and the contents sprinkled on small amounts of acidic soft food of pH 4.5 or less (e.g., commercially available preparations of bananas, pears and applesauce).
The PANCRELIPASE-soft food mixture should be swallowed immediately without crushing or chewing, and followed with water or juice to ensure complete ingestion. Care should be taken to ensure that no drug is retained in the mouth.
-
Aurobindo Pharma Limited
![Lamotrigine Tablet [Aurobindo Pharma Limited]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Aurobindo Pharma Limited
![Lamotrigine Tablet [Aurobindo Pharma Limited] Lamotrigine Tablet [Aurobindo Pharma Limited]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash
There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation for lamotrigine tablets is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine tablets, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Tablets Added to Drugs Known to Induce or Inhibit Glucuronidation
Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine. Drugs that induce glucuronidation include carbamazepine, phenytoin, phenobarbital, primidone, rifampin, estrogen-containing oral contraceptives, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Valproate inhibits glucuronidation. For dosing considerations for lamotrigine tablets in patients on estrogen-containing contraceptives and atazanavir/ritonavir, see below and Table 13. For dosing considerations for lamotrigine tablets in patients on other drugs known to induce or inhibit glucuronidation, see Table 1, Table 2, Table 5, Table 6, and Table 13.Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder
A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3)].Women Taking Estrogen-Containing Oral Contraceptives
Starting Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.Adjustments to the Maintenance Dose of Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives
(1) Taking Estrogen-Containing Oral Contraceptives: In women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be increased by as much as 2-fold over the recommended target maintenance dose to maintain a consistent lamotrigine plasma level.
(2) Starting Estrogen-Containing Oral Contraceptives:In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (pill-free week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the pill-free week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the pill-free week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: In women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. In women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy
The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.Patients Taking Atazanavir/Ritonavir
While atazanavir/ritonavir does reduce the lamotrigine plasma concentration, no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of atazanavir/ritonavir. Dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on concomitant AED or other concomitant medications (see Tables 1, 2, and 5). In patients already taking maintenance doses of lamotrigine tablets and not taking glucuronidation inducers, the dose of lamotrigine tablets may need to be increased if atazanavir/ritonavir is added, or decreased if atazanavir/ritonavir is discontinued [see Clinical Pharmacology (12.3)].Patients With Hepatic Impairment
Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 subjects with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.Patients With Renal Impairment
Initial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1 to 3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.Discontinuation Strategy
Epilepsy: For patients receiving lamotrigine tablets in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with bipolar disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these patients with bipolar disorder. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy - Adjunctive TherapyThis section provides specific dosing recommendations for patients older than 12 years and patients aged 2 to 12 years. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AEDs or other concomitant medications (see Table 1 for patients older than 12 years and Table 2 for patients aged 2 to 12 years). A weight-based dosing guide for patients aged 2 to 12 years on concomitant valproate is provided in Table 3.
Patients Older Than 12 Years
Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine Tablets in Patients Older Than 12 Years With Epilepsy a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)].
In Patients TAKING Valproatea
In Patients NOT TAKING
Carbamazepine,
Phenytoin, Phenobarbital, Primidone,b or Valproatea
In Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Week 5 onward
to maintenance
Increase by 25 to
50 mg/day every 1 to
2 weeks.
Increase by 50 mg/day
every 1 to 2 weeks.
Increase by
100 mg/day every
1 to 2 weeks.
Usual maintenance
dose
100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses)
225 to 375 mg/day
(in 2 divided doses)
300 to 500 mg/day
(in 2 divided doses)
Patients Aged 2 to 12 Years
Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine Tablets in Patients Aged 2 to 12 Years With Epilepsy Note: Only whole tablets should be used for dosing.
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)].
In Patients TAKING Valproatea
In Patients NOT TAKING
Carbamazepine,
Phenytoin, Phenobarbital, Primidone,b or Valproatea
In Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea
Weeks 1 and 2
0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide)
0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet
0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet
Weeks 3 and 4
0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide)
0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet
1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet
Week 5 onward to maintenance
The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose.
The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose.
The dose should be increased every 1 to 2 weeks as follows: calculate
1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose.
Usual
maintenance
dose
1 to 5 mg/kg/day
(maximum 200 mg/day in
1 or 2 divided doses)
1 to 3 mg/kg/day with
valproate alone
4.5 to 7.5 mg/kg/day (maximum 300 mg/day in
2 divided doses)
5 to 15 mg/kg/day
(maximum
400 mg/day in 2
divided doses)
Maintenance
dose in
patients less
than 30 kg
May need to be increased
by as much as 50%, based
on clinical response
May need to be increased
by as much as 50%, based
on clinical response
May need to be
increased by as
much as 50%, based
on clinical response
Table 3. The Initial Weight-Based Dosing Guide for Patients Aged 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is
Give this daily dose, using the most appropriate combination of lamotrigine 2 mg and 5 mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy:
The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive trials in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 to 4 has not been established in controlled trials.
2.3 Epilepsy - Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to attempt to maintain seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations for lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets
After achieving a dose of 500 mg/day of lamotrigine tablets using the guidelines in Table 1, the concomitant enzyme-inducing AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets
The conversion regimen involves the 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets in Patients Aged 16 Years and Older With Epilepsy
Lamotrigine Tablets
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1.
Maintain established stable dose.
Step 2
Maintain at 200 mg/day.
Decrease dose by decrements no greater than 500 mg/day/week to 500 mg/day and then maintain for 1 week.
Step 3
Increase to 300 mg/day and maintain for
1 week.
Simultaneously decrease to
250 mg/day and maintain for
1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion From Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets
2.4 Bipolar Disorder
No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenytoin, phenobarbital, primidone, or valproate.The goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitor lopinavir/ritonavir that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine Tablets in Patients With Bipolar Disorder a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)].
In Patients TAKING Valproatea
In Patients NOT
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital,
Primidone,b or
Valproatea
In Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
Table 6. Dosage Adjustments to Lamotrigine Tablets in Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)].
Discontinuation of
Psychotropic Drugs
(excluding Valproate,a
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidoneb)
After Discontinuation of Valproatea
After Discontinuation of
Carbamazepine,
Phenytoin, Phenobarbital, or Primidoneb
Current dose of lamotrigine tablets (mg/day)
100
Current dose of lamotrigine tablets (mg/day)
400
Week 1
Maintain current dose of lamotrigine tablets
150
400
Week 2
Maintain current dose of lamotrigine tablets
200
300
Week 3 onward
Maintain current dose of lamotrigine tablets
200
200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine tablets was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2 )]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Dr.reddy’s Laboratories Limited
![Lamotrigine Tablet, Extended Release [Dr.reddy’s Laboratories Limited]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Dr.reddy's Laboratories Limited
![Lamotrigine Tablet, Extended Release [Dr.reddy’s Laboratories Limited] Lamotrigine Tablet, Extended Release [Dr.reddy’s Laboratories Limited]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine extended-release tablets are taken once daily, with or without food. Tablets must be swallowed whole and must not be chewed, crushed, or divided.
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine extended-release tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine extended-release tablets, or (3) exceeding the recommended dose escalation for lamotrigine extended-release tablets. However, cases have occurred in the absence of these factors [see BoxedWarning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation for lamotrigine extended-release tablets are exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine extended-release tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine extended-release tablets, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Extended-Release Tablets Added to Drugs Known to Induce or Inhibit Glucuronidation: Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine. Drugs that induce glucuronidation include carbamazepine, phenytoin, phenobarbital, primidone, rifampin, estrogen-containing oral contraceptives, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Valproate inhibits glucuronidation. For dosing considerations for lamotrigine extended-release tablets in patients on estrogen-containing contraceptives and atazanavir/ritonavir, see below and Table 5. For dosing considerations for lamotrigine extended-release tablets in patients on other drugs known to induce or inhibit glucuronidation, see Table 1 and Table 5.
Target Plasma Levels: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine extended-release tablets should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Extended-Release Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine extended-release tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine extended-release tablets based on the concomitant AED or other concomitant medications (see Table 1). See below for adjustments to maintenance doses of lamotrigine extended-release tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Extended-Release Tablets in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: In women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)] the maintenance dose of lamotrigine extended-release tablets will in most cases need to be increased by as much as 2-fold over the recommended target maintenance dose to maintain a consistent lamotrigine plasma level.
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine extended-release tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (pill-free week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine extended-release tablets consistently occur during the pill-free week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the pill-free week are not recommended. For women taking lamotrigine extended-release tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine extended-release tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: In women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine extended-release tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine extended-release tablets should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see ClinicalPharmacology (12.3)].In women taking lamotrigine extended-release tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine extended-release tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine extended-release tablets in the presence of progestogens alone will likely not be needed.
Patients Taking Atazanavir/Ritonavir: While atazanavir/ritonavir does reduce the lamotrigine plasma concentration, no adjustments to the recommended dose-escalation guidelines for lamotrigine extended-release tablets should be necessary solely based on the use of atazanavir/ritonavir. Dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine extended-release tablets based on concomitant AED or other concomitant medications (see Tables 1 and 5). In patients already taking maintenance doses of lamotrigine extended-release tablets and not taking glucuronidation inducers, the dose of lamotrigine extended-release tablets may need to be increased if atazanavir/ritonavir is added, or decreased if atazanavir/ritonavir is discontinued [see Clinical Pharmacology (12.3)].
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 subjects with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine extended-release tablets should be based on patients’ concomitant medications (see Table 1); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), ClinicalPharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with immediate-release lamotrigine. Because there is inadequate experience in this population, lamotrigine extended-release tablets should be used with caution in these patients.
Discontinuation Strategy: For patients receiving lamotrigine extended-release tablets in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine extended-release tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.8)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
2.2 Adjunctive Therapy for Primary Generalized Tonic-Clonic and Partial-Onset SeizuresThis section provides specific dosing recommendations for patients aged 13 years and older. Specific dosing recommendations are provided depending upon concomitant AEDs or other concomitant medications.
Table 1. Escalation Regimen for Lamotrigine Extended-Release Tablets in Patients Aged 13 Years and Older
For Patients TAKING Valproatea For PatientsNOT TAKING Carbamazepine, Phenytoin,Phenobarbital, Primidone,b or Valproatea For Patients TAKING Carbamazepine, Phenytoin,Phenobarbital, or Primidoneb and NOT TAKING Valproatea Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg every day Weeks 3 and 4 25 mg every day 50 mg every day 100 mg every day Week 5 50 mg every day 100 mg every day 200 mg every day Week 6 100 mg every day 150 mg every day 300 mg every day Week 7 150 mg every day 200 mg every day 400 mg every day Maintenance range (week 8 and onward) 200 to 250 mg everydayc 300 to 400 mg every dayc 400 to 600 mg every dayca Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)].
c Dose increases at week 8 or later should not exceed 100 mg daily at weekly intervals.
2.3 Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to attempt to maintain seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine extended-release tablets.
To avoid an increased risk of rash, the recommended maintenance dosage range of lamotrigine extended-release tablets as monotherapy is 250 to 300 mg given once daily.
The recommended initial dose and subsequent dose escalations for lamotrigine extended-release tablets should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Extended-Release Tablets:
After achieving a dose of 500 mg/day of lamotrigine extended-release tablets using the guidelines in Table 1, the concomitant enzyme-inducing AED should be withdrawn by 20% decrements each week over a 4-week period. Two weeks after completion of withdrawal of the enzyme-inducing AED, the dosage of lamotrigine extended-release tablets may be decreased no faster than 100 mg/day each week to achieve the monotherapy maintenance dosage range of 250 to 300 mg/day.
The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial using immediate-release lamotrigine.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Extended-Release Tablets:
The conversion regimen involves the 4 steps outlined in Table 2.
Table 2. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Extended-Release Tablets in Patients Aged 13 Years and Older With Epilepsy
Lamotrigine Extended-Release Tablets Valproate Step 1 Achieve a dose of 150 mg/day according to guidelines in Table 1. Maintain established stable dose. Step 2 Maintain at 150 mg/day. Decrease dose by decrements no greater than 500 mg/day/week to 500 mg/day and then maintain for 1 week. Step 3 Increase to 200 mg/day. Simultaneously decrease to 250 mg/day and maintain for 1 week. Step 4 Increase to 250 or 300 mg/day. Discontinue.Conversion From Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Extended-Release Tablets:
After achieving a dosage of 250 to 300 mg/day of lamotrigine extended-release tablets using the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. No adjustment to the monotherapy dose of lamotrigine extended-release tablets is needed.
2.4 Conversion From Immediate-Release Lamotrigine Tablets to Lamotrigine Extended-Release TabletsPatients may be converted directly from immediate-release lamotrigine to lamotrigine extended-release tablets. The initial dose of lamotrigine extended-release tablets should match the total daily dose of immediate-release lamotrigine. However, some subjects on concomitant enzyme inducing agents may have lower plasma levels of lamotrigine on conversion and should be monitored [see Clinical Pharmacology (12.3)].
Following conversion to lamotrigine extended-release tablets, all patients (but especially those on drugs that induce lamotrigine glucuronidation) should be closely monitored for seizure control [see Drug Interactions (7)]. Depending on the therapeutic response after conversion, the total daily dose may need to be adjusted within the recommended dosing instructions (Table 1).
-
Aurobindo Pharma Limited
![Lamotrigine Tablet, Chewable [Aurobindo Pharma Limited]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Aurobindo Pharma Limited
![Lamotrigine Tablet, Chewable [Aurobindo Pharma Limited] Lamotrigine Tablet, Chewable [Aurobindo Pharma Limited]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash
There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets (chewable, dispersible) with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets (chewable, dispersible), or (3) exceeding the recommended dose escalation for lamotrigine tablets (chewable, dispersible). However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation for lamotrigine tablets (chewable, dispersible) is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets (chewable, dispersible) not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine tablets (chewable, dispersible), the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Tablets (Chewable, Dispersible) Added to Drugs Known to Induce or Inhibit Glucuronidation
Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine. Drugs that induce glucuronidation include carbamazepine, phenytoin, phenobarbital, primidone, rifampin, estrogen-containing oral contraceptives, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Valproate inhibits glucuronidation. For dosing considerations for lamotrigine tablets (chewable, dispersible) in patients on estrogen-containing contraceptives and atazanavir/ritonavir, see below and Table 13. For dosing considerations for lamotrigine tablets (chewable, dispersible) in patients on other drugs known to induce or inhibit glucuronidation, see Tables 1, 2, 5 to 6, and 13.Target Plasma Levels for Patients with Epilepsy or Bipolar Disorder
A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets (chewable, dispersible) should be based on therapeutic response [see Clinical Pharmacology (12.3)].Women Taking Estrogen-Containing Oral Contraceptives
Starting Lamotrigine Tablets (Chewable, Dispersible) in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets (chewable, dispersible) should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets (chewable, dispersible) based on the concomitant AED or other concomitant medications (see Tables 1, 5, and 7). See below for adjustments to maintenance doses of lamotrigine tablets (chewable, dispersible) in women taking estrogen-containing oral contraceptives.Adjustments to the Maintenance Dose of Lamotrigine Tablets (Chewable, Dispersible) in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: In women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets (chewable, dispersible) will in most cases need to be increased by as much as 2-fold over the recommended target maintenance dose to maintain a consistent lamotrigine plasma level.
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets (chewable, dispersible) and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Tables 1 and 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (pill-free week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets (chewable, dispersible) consistently occur during the pill-free week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the pill-free week are not recommended. For women taking lamotrigine tablets (chewable, dispersible) in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets (chewable, dispersible) should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: In women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets (chewable, dispersible) will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets (chewable, dispersible) should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. In women taking lamotrigine tablets (chewable, dispersible) in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets (chewable, dispersible) should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy
The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets (chewable, dispersible) in the presence of progestogens alone will likely not be needed.Patients Taking Atazanavir/Ritonavir
While atazanavir/ritonavir does reduce the lamotrigine plasma concentration, no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets (chewable, dispersible) should be necessary solely based on the use of atazanavir/ritonavir. Dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets (chewable, dispersible) based on concomitant AED or other concomitant medications (see Tables 1, 2, and 5). In patients already taking maintenance doses of lamotrigine tablets (chewable, dispersible) and not taking glucuronidation inducers, the dose of lamotrigine tablets (chewable, dispersible) may need to be increased if atazanavir/ritonavir is added, or decreased if atazanavir/ritonavir is discontinued [see Clinical Pharmacology (12.3)].Patients with Hepatic Impairment
Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 subjects with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.Patients with Renal Impairment
Initial doses of lamotrigine tablets (chewable, dispersible) should be based on patients’ concomitant medications (see Tables 1 to 3, and 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets (chewable, dispersible). Because there is inadequate experience in this population, lamotrigine tablets (chewable, dispersible) should be used with caution in these patients.Discontinuation Strategy
Epilepsy: For patients receiving lamotrigine tablets (chewable, dispersible) in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.If a decision is made to discontinue therapy with lamotrigine tablets (chewable, dispersible), a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.8)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets (chewable, dispersible). In the clinical development program in adults with bipolar disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets (chewable, dispersible). Discontinuation of lamotrigine tablets (chewable, dispersible) should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.8)].
2.2 Epilepsy - Adjunctive TherapyThis section provides specific dosing recommendations for patients older than 12 years and patients aged 2 to 12 years. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AEDs or other concomitant medications (see Table 1 for patients older than 12 years and Table 2 for patients aged 2 to 12 years). A weight-based dosing guide for patients aged 2 to 12 years on concomitant valproate is provided in Table 3.
Table 1. Escalation Regimen for Lamotrigine Tablets (Chewable, Dispersible) in Patients Older than 12 Years with Epilepsy a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
Patients Older than 12 Years
Recommended dosing guidelines are summarized in Table 1.
b Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)].
In Patients TAKING
Valproatea
In Patients NOT TAKING
Carbamazepine, Phenytoin,
Phenobarbital, Primidone,b
or Valproatea
In Patients TAKING
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidoneb and NOT
TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Week 5 onward
to maintenance
Increase by 25 to
50 mg/day every 1 to
2 weeks.
Increase by 50 mg/day
every 1 to 2 weeks.
Increase by
100 mg/day every
1 to 2 weeks.
Usual maintenance
dose
100 to 200 mg/day with
valproate alone
100 to 400 mg/day with
valproate and other
drugs that induce
glucuronidation
(in 1 or 2 divided doses)
225 to 375 mg/day
(in 2 divided doses)
300 to 500 mg/day
(in 2 divided doses)
Patients Aged 2 to 12 Years
Table 2. Escalation Regimen for Lamotrigine Tablets (Chewable, Dispersible) in Patients Aged 2 to 12 Years with Epilepsy Note: Only whole tablets should be used for dosing.
Recommended dosing guidelines are summarized in Table 2.
Lower starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by lower starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
The smallest available strength of lamotrigine tablets (chewable, dispersible) is 2 mg, and only whole tablets should be administered. If the calculated dose cannot be achieved using whole tablets, the dose should be rounded down to the nearest whole tablet [see How Supplied/Storage and Handling (16) and Medication Guide].
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)].
In Patients TAKING
Valproatea
In Patients NOT TAKING
Carbamazepine,
Phenytoin, Phenobarbital,
Primidone,b or Valproatea
In Patients TAKING
Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidoneb and NOT
TAKING Valproatea
Weeks 1 and 2
0.15 mg/kg/day
in 1 or 2 divided doses,
rounded down to the nearest
whole tablet (see Table 3 for
weight-based dosing guide)
0.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the nearest
whole tablet
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet
Weeks 3 and 4
0.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the nearest
whole tablet (see Table 3 for
weight-based dosing guide)
0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet
1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet
Week 5 onward to maintenance
The dose should be increased
every 1 to 2 weeks as follows:
calculate 0.3 mg/kg/day,
round this amount down to
the nearest whole tablet, and
add this amount to the
previously administered daily
dose.
The dose should be
increased every 1 to 2 weeks
as follows: calculate 0.6
mg/kg/day, round this
amount down to the nearest
whole tablet, and add this
amount to the previously
administered daily dose.
The dose should be
increased every 1 to 2
weeks as follows: calculate
1.2 mg/kg/day, round this
amount down to the
nearest whole tablet, and
add this amount to the
previously administered
daily dose.
Usual
maintenance
dose
1 to 5 mg/kg/day
(maximum 200 mg/day in
1 or 2 divided doses)
1 to 3 mg/kg/day with
valproate alone
4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in
2 divided doses)
5 to 15 mg/kg/day
(maximum
400 mg/day in 2
divided doses)
Maintenance
dose in
patients less
than 30 kg
May need to be increased
by as much as 50%, based
on clinical response.
May need to be increased
by as much as 50%, based
on clinical response.
May need to be
increased by as
much as 50%, based
on clinical response.
Table 3. The Initial Weight-Based Dosing Guide for Patients Aged 2 to 12 Years Taking Valproate (Weeks 1 to 4) with Epilepsy If the patient’s weight is
Give this daily dose, using the most appropriate
combination of lamotrigine tablets (chewable, dispersible)
2 mg and 5 mg
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy
2.3 Epilepsy - Conversion from Adjunctive Therapy to Monotherapy
The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive trials in which the efficacy of lamotrigine tablets (chewable, dispersible) was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets (chewable, dispersible) as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets (chewable, dispersible) as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 to 4 has not been established in controlled trials.The goal of the transition regimen is to attempt to maintain seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets (chewable, dispersible).
The recommended maintenance dose of lamotrigine tablets (chewable, dispersible) as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations for lamotrigine tablets (chewable, dispersible) should not be exceeded [see Boxed Warning].
Table 4. Conversion from Adjunctive Therapy with Valproate to Monotherapy with Lamotrigine Tablets (Chewable, Dispersible) in Patients Aged 16 Years and Older with Epilepsy
Conversion from Adjunctive Therapy with Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy with Lamotrigine Tablets (Chewable, Dispersible)
After achieving a dose of 500 mg/day of lamotrigine tablets (chewable, dispersible) using the guidelines in Table 1, the concomitant enzyme-inducing AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy with Valproate to Monotherapy with Lamotrigine Tablets (Chewable, Dispersible)
The conversion regimen involves the 4 steps outlined in Table 4.
Lamotrigine Tablets
(Chewable, Dispersible)
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1.
Maintain established stable dose.
Step 2
Maintain at 200 mg/day.
Decrease dose by decrements no greater than 500 mg/day/week to 500 mg/day and then maintain for 1 week.
Step 3
Increase to 300 mg/day and maintain for
1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy with Antiepileptic Drugs other than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy with Lamotrigine Tablets (Chewable, Dispersible)
2.4 Bipolar Disorder
No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets (chewable, dispersible) with AEDs other than carbamazepine, phenytoin, phenobarbital, primidone, or valproate.The goal of maintenance treatment with lamotrigine tablets (chewable, dispersible) is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy [see Indications and Usage (1)].
Patients taking lamotrigine tablets (chewable, dispersible) for more than 16 weeks should be periodically reassessed to determine the need for maintenance treatment.
Adults
The target dose of lamotrigine tablets (chewable, dispersible) is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitor lopinavir/ritonavir that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended.
Treatment with lamotrigine tablets (chewable, dispersible) is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets (chewable, dispersible) should be adjusted. In patients discontinuing valproate, the dose of lamotrigine tablets (chewable, dispersible) should be doubled over a 2-week period in equal weekly increments (see Table 6). In patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation, the dose of lamotrigine tablets (chewable, dispersible) should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets (chewable, dispersible) may then be further adjusted to the target dose (200 mg) as clinically indicated.If other drugs are subsequently introduced, the dose of lamotrigine tablets (chewable, dispersible) may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets (chewable, dispersible) [see Drug Interactions (7), Clinical Pharmacology (12.3)].
Table 5. Escalation Regimen for Lamotrigine Tablets (Chewable, Dispersible) in Adults with Bipolar Disorder a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets (chewable, dispersible) should not be exceeded [see Boxed Warning].
b Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)].
In Patients TAKING Valproatea
In Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidoneb,or Valproatea
In Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
Table 6. Dosage Adjustments to Lamotrigine Tablets (Chewable, Dispersible) in Adults with Bipolar Disorder Following Discontinuation of Psychotropic Medications a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)].
Discontinuation of Psychotropic Drugs (excluding Valproate,a Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb)
After Discontinuation of Valproatea
After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or
Primidoneb
Current Dose of lamotrigine tablets (chewable, dispersible) (mg/day) 100
Current Dose of lamotrigine tablets (chewable, dispersible) (mg/day) 400
Week 1
Maintain current dose of lamotrigine tablets (chewable, dispersible)
150
400
Week 2
Maintain current dose of lamotrigine tablets (chewable, dispersible)
200
300
Week 3 onward
Maintain current dose of lamotrigine tablets (chewable, dispersible)
200
200
2.5 Administration of Lamotrigine Tablets (Chewable, Dispersible)Lamotrigine tablets (chewable, dispersible) may be swallowed whole, chewed, or dispersed in water or diluted fruit juice. If the tablets are chewed, consume a small amount of water or diluted fruit juice to aid in swallowing.
To disperse lamotrigine tablets (chewable, dispersible), add the tablets to a small amount of liquid (1 teaspoon, or enough to cover the medication). Approximately 1 minute later, when the tablets are completely dispersed, swirl the solution and consume the entire quantity immediately. No attempt should be made to administer partial quantities of the dispersed tablets. -
Apotex Corp
![Lamotrigine Tablet [Apotex Corp]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Mylan Pharmaceuticals Inc.
![Lamotrigine Tablet [Apotex Corp] Lamotrigine Tablet [Apotex Corp]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 HypertensionDosage must be individualized. The usual starting dose of telmisartan tablets is 40 mg once a day. Blood pressure response is dose-related over the range of 20 mg to 80 mg [see Clinical Studies (14.1)].
Most of the antihypertensive effect is apparent within 2 weeks and maximal reduction is generally attained after 4 weeks. When additional blood pressure reduction beyond that achieved with 80 mg telmisartan is required, a diuretic may be added.
No initial dosage adjustment is necessary for elderly patients or patients with renal impairment, including those on hemodialysis. Patients on dialysis may develop orthostatic hypotension; their blood pressure should be closely monitored.
Telmisartan tablets may be administered with other antihypertensive agents.
Telmisartan tablets may be administered with or without food.
-
Cardinal Health
![Lamotrigine Tablet [Cardinal Health]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Cardinal Health
![Lamotrigine Tablet [Cardinal Health] Lamotrigine Tablet [Cardinal Health]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing Considerations RashThere are suggestions, yet to be proven, that the risk of severe, potentially life threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablets are exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Tablets Added to Drugs Known to Induce or Inhibit GlucuronidationDrugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets may require adjustment based on clinical response.
Target Plasma Levels for Patients with Epilepsy or Bipolar DisorderA therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women taking Estrogen-Containing Oral Contraceptives Starting Lamotrigine Tablets in Women taking Estrogen-Containing Oral ContraceptivesAlthough estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets in Women taking Estrogen-Containing Oral Contraceptives(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement TherapyThe effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.
Patients with Hepatic ImpairmentExperience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients with Renal ImpairmentInitial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1 to 3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.
Discontinuation Strategy EpilepsyFor patients receiving lamotrigine tablets in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.10)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar DisorderIn the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with bipolar disorder, two patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.10)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of AgeRecommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine Tablets in Patients Over 12 Years of Age with Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.For Patients TAKING
Valproate*For Patients NOT
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital,
Primidone† or
Valproate*For Patients
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital or
Primidone† and
NOT
TAKING
Valproate*Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)Week 5 onwards
to maintenanceIncrease by 25 to 50 mg/day every 1 to 2 weeks
Increase by 50 mg/day every 1 to 2 weeks
Increase by 100 mg/day every 1 to 2 weeks
Usual Maintenance
Dose100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses)225 to 375 mg/day
(in 2 divided doses)300 to 500 mg/day
Patients 2 to 12 Years of Age
(in 2 divided doses)Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine Tablets in Patients 2 to 12 Years of Age with Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.For Patients TAKING
Valproate*
For Patients NOT
TAKING
Carbamazepine,
Phenytoin, Phenobarbital, Primidone† or Valproate*For Patients TAKING
Carbamazepine,
Phenytoin,
Phenobarbital or
Primidone† and NOT
TAKING Valproate*Weeks
1 and 20.15 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet (see
Table 3 for weight based
dosing guide).0.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet.0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet.Weeks
3 and 40.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
(see Table 3 for weight
based dosing guide).0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet.1.2 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet.Week 5
onwards tomaintenance
The dose should be
increased every 1 to
2 weeks as follows:
calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet
and add this
amount to the previously
administered daily dose.The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day,
round this amount down to the nearest whole tablet and add this amount to the previously administered daily dose.
The dose should be
increased every 1 to 2 weeks as follows:
calculate
1.2 mg/kg/day, round this amount
down to the nearest
whole tablet and
add this amount to
the previously
administered daily
dose.Usual
Maintenance
Dose
1 to 5 mg/kg/day
(maximum 200 mg/day in
1 or 2 divided doses).
1 to 3 mg/kg/day with
valproate alone.4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses).5 to 15 mg/kg/day
(maximum 400 mg/day in 2 divided doses).Maintenance
dose in
patients less
than 30 kg
May need to be increased
by as much as 50%, based
on clinical response.May need to be increased by as much as 50%, based on clinical response.
May need to be
increased by as
much as 50%, based
on clinical response.Note: Only whole tablets should be used for dosing.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years of Age taking Valproate (Weeks 1 to 4) with EpilepsyIf the patient's weight is
Give this daily dose, using the most appropriate combination of lamotrigine 2 mg and 5 mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for EpilepsyThe usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion from Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in two divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion from Adjunctive Therapy with Carbamazepine, Phenytoin, Phenobarbital or Primidone to Monotherapy with Lamotrigine TabletsAfter achieving a dose of 500 mg/day of lamotrigine tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy with Valproate to Monotherapy with Lamotrigine TabletsThe conversion regimen involves four steps outlined in Table 4.
Table 4. Conversion from Adjunctive Therapy with Valproate to Monotherapy with Lamotrigine Tablets in Patients ≥ 16 Years of Age with EpilepsyLamotrigine Tablets
Valproate
Step 1
Achieve a dose of 200 mg/day according to
guidelines in Table 1 (if not already on200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by
decrements no greater than
500 mg/day/week and then
maintain the dose of
500 mg/day for one week.Step 3
Increase to 300 mg/day and maintain
for one week.Simultaneously decrease to
250 mg/day and maintain for
one week.Step 4
Increase by 100 mg/day every week to achieve
maintenance dose of 500 mg/day.Discontinue.
Conversion from Adjunctive Therapy with Antiepileptic Drugs Other than Carbamazepine, Phenytoin, Phenobarbital, Primidone or Valproate to Monotherapy with Lamotrigine TabletsNo specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine Tablets for Patients with Bipolar Disorder * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.For Patients
TAKING
Valproate*For Patients NOT
TAKING
Carbamazepine,
Phenytoin,
Phenobarbital,
Primidone† or
Valproate*For Patients
TAKING
Carbamazepine,
Phenytoin, Phenobarbital or
Primidone† and
NOT TAKING
Valproate*Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
Table 6. Dosage Adjustments to Lamotrigine Tablets for Patients with Bipolar Disorder Following Discontinuation of Psychotropic Medications * These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. † Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].Discontinuation of
Psychotropic Drugs
(excluding Carbamazepine,
Phenytoin, Phenobarbital,
Primidone*
or Valproate†)After
Discontinuation
of Valproate†After Discontinuation
of Carbamazepine,
Phenytoin,
Phenobarbital or
Primidone*Current dose of lamotrigine tablets (mg/day)
100Current dose of lamotrigine tablets (mg/day)
400Week 1
Maintain current dose of lamotrigine tablets
150
400
Week 2
Maintain current dose of lamotrigine tablets
200
300
Week 3 onward
Maintain current dose of lamotrigine tablets
200
200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine tablets was established in two randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Carilion Materials Management
![Lamotrigine Tablet, Chewable [Carilion Materials Management]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Carilion Materials Management
![Lamotrigine Tablet, Chewable [Carilion Materials Management] Lamotrigine Tablet, Chewable [Carilion Materials Management]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing Considerations: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets (chewable, dispersible) with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets (chewable, dispersible), or (3) exceeding the recommended dose escalation for lamotrigine tablets (chewable, dispersible). However, cases have occurred in the absence of these factors [see ]. Therefore, it is important that the dosing recommendations be followed closely. RashBoxed Warning
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablets (chewable, dispersible) is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets (chewable, dispersible) not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [ ]. see Clinical Pharmacology ( ) 12.3
: Drugs other than those listed in the Clinical Pharmacology section [ ] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets (chewable, dispersible) may require adjustment based on clinical response. Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidationsee Clinical Pharmacology ( ) 12.3
: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets (chewable, dispersible) should be based on therapeutic response [ ]. Target Plasma Levels for Patients With Epilepsy or Bipolar Disordersee Clinical Pharmacology ( ) 12.3
: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [ ], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets (chewable, dispersible) should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets (chewable, dispersible) based on the concomitant AED or other concomitant medications (see or ). See below for adjustments to maintenance doses of lamotrigine tablets (chewable, dispersible) in women taking estrogen-containing oral contraceptives. Women Taking Estrogen-Containing Oral ContraceptivesStarting Lamotrigine Tablets (Chewable, Dispersible) in Women Taking Estrogen-Containing Oral Contraceptives:see Clinical Pharmacology ( ) 12.3Table 1Table 5
Adjustments to the Maintenance Dose of Lamotrigine Tablets (Chewable, Dispersible) in Women Taking Estrogen-Containing Oral Contraceptives:
For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [ ], the maintenance dose of lamotrigine tablets (chewable, dispersible) will in most cases need to be increased, by as much as 2 fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [ ]. (1) Taking Estrogen-Containing Oral Contraceptives:see Drug Interactions ( ), Clinical Pharmacology ( ) 712.3see Clinical Pharmacology ( ) 12.3
In women taking a stable dose of lamotrigine tablets (chewable, dispersible) and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [ ], the maintenance dose will in most cases need to be increased by as much as 2 fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see or ) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (“pill-free” week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets (chewable, dispersible) consistently occur during the “pill-free” week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the “pill-free” week are not recommended. For women taking lamotrigine tablets (chewable, dispersible) in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [ ], no adjustment to the dose of lamotrigine tablets (chewable, dispersible) should be necessary. (2) Starting Estrogen-Containing Oral Contraceptives:see Drug Interactions ( ), Clinical Pharmacology ( ) 712.3Table 1Table 5see Drug Interactions ( ), Clinical Pharmacology ( ) 712.3
For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [ ], the maintenance dose of lamotrigine tablets (chewable, dispersible) will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets (chewable, dispersible) should not exceed 25% of the total daily dose per week over a 2 week period, unless clinical response or lamotrigine plasma levels indicate otherwise [ ]. For women taking lamotrigine tablets (chewable, dispersible) in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [ ], no adjustment to the dose of lamotrigine tablets (chewable, dispersible) should be necessary. (3) Stopping Estrogen-Containing Oral Contraceptives:see Drug Interactions ( ), Clinical Pharmacology ( ) 712.3see Clinical Pharmacology ( ) 12.3see Drug Interactions ( ), Clinical Pharmacology ( ) 712.3
: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2 fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets (chewable, dispersible) in the presence of progestogens alone will likely not be needed. Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy
: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [ ], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response. Patients With Hepatic Impairmentsee Use in Specific Populations ( ), Clinical Pharmacology ( ) 8.612.3
: Initial doses of lamotrigine tablets (chewable, dispersible) should be based on patients' concomitant medications (see to or ); reduced maintenance doses may be effective for patients with significant renal impairment [ ]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets (chewable, dispersible). Because there is inadequate experience in this population, lamotrigine tablets (chewable, dispersible) should be used with caution in these patients. Patients With Renal ImpairmentTables 13Table 5see Use in Specific Populations ( ), Clinical Pharmacology ( ) 8.712.3
: For patients receiving lamotrigine tablets (chewable, dispersible) in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed. Discontinuation StrategyEpilepsy:
If a decision is made to discontinue therapy with lamotrigine tablets (chewable, dispersible), a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [ ]. see Warnings and Precautions ( ) 5.9
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets (chewable, dispersible). In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets (chewable, dispersible). However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets (chewable, dispersible) should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [ ]. Bipolar Disorder:see Warnings and Precautions ( ) 5.9
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications ( for patients greater than 12 years of age and for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in . Table 1Table 2Table 3
Recommended dosing guidelines are summarized in . Patients Over 12 Years of Age:Table 1
Table 1. Escalation Regimen for Lamotrigine in Patients Over 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ ]. see Drug Interactions ( ), Clinical Pharmacology ( ) 712.3 † These drugs induce lamotrigine glucuronidation and increase clearance [ ]. Other drugs that have similar effects include estrogen-containing oral contraceptives [ ]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [ ]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. see Drug Interactions ( ), Clinical Pharmacology ( ) 712.3 see Drug Interactions ( ), Clinical Pharmacology ( ) 712.3 see Dosage and Administration ( ) 2.1For Patients TAKING Valproate *
For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate †* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone and NOT TAKING Valproate †* Weeks 1 and 2 25 mg every day other 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day (in 2 divided doses) 100 mg/day Week 5 onwards to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks Increase by 50 mg/day every 1 to 2 weeks Increase by 100 mg/day every 1 to 2 weeks Usual Maintenance Dose100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induceglucuronidation
(in 1 or 2 divided doses)
225 to 375 mg/day
(in 2 divided doses)
300 to 500 mg/day
(in 2 divided doses)
Recommended dosing guidelines are summarized in . Patients 2 to 12 Years of Age:Table 2
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
[ ]. The smallest available strength of lamotrigine tablets (chewable, dispersible) is 2 mg, and only whole tablets should be administered. If the calculated dose cannot be achieved using whole tablets, the dose should be rounded down to the nearest whole tabletsee How Supplied/Storage and Handling ( ) and 16Medication Guide
Table 2. Escalation Regimen for Lamotrigine in Patients 2 to 12 Years of Age With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ ]. see Drug Interactions ( ), Clinical Pharmacology ( ) 712.3 † These drugs induce lamotrigine glucuronidation and increase clearance [ ]. Other drugs that have similar effects include estrogen-containing oral contraceptives [ ]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [ ]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. see Drug Interactions ( ), Clinical Pharmacology ( ) 712.3 see Drug Interactions ( ), Clinical Pharmacology ( ) 712.3 see Dosage and Administration ( ) 2.1 For Patients TAKING Valproate * For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate †* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone and NOT TAKING Valproate †* Weeks 1 and 2 in 1 or 2 divided doses, rounded down to the nearest whole tablet (see for weight based dosing guide) 0.15 mg/kg/dayTable 3 in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.3 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day Weeks 3 and 4 in 1 or 2 divided doses, rounded down to the nearest whole tablet (see for weight based dosing guide) 0.3 mg/kg/dayTable 3 in 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day Week 5 onwards to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose Usual Maintenance Dose (maximum 200 mg/day in 1 or 2 divided doses) with valproate alone 1 to 5 mg/kg/day1 to 3 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 4.5 to 7.5 mg/kg/day (maximum 400 mg/day in 2 divided doses) 5 to 15 mg/kg/day Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical response May need to be increased by as much as 50%, based on clinical responseNote: Only whole tablets should be used for dosing.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years of Age Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of lamotrigine tablets, 2 mg and 5 mg Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every day other 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayThe usual maintenance doses identified in and are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets (chewable, dispersible) was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone , maintenance doses of adjunctive lamotrigine tablets (chewable, dispersible) as high as 700 mg/day have been used. In patients receiving , maintenance doses of adjunctive lamotrigine tablets (chewable, dispersible) as high as 200 mg/day have been used. The advantage of using doses above those recommended in through has not been established in controlled trials. Usual Adjunctive Maintenance Dose for Epilepsy:Tables 12without valproatevalproate aloneTables 14
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets (chewable, dispersible) under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets (chewable, dispersible).
The recommended maintenance dose of lamotrigine tablets (chewable, dispersible) as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets (chewable, dispersible) should not be exceeded [see ]. Boxed Warning
After achieving a dose of 500 mg/day of lamotrigine tablets (chewable, dispersible) according to the guidelines in , the concomitant AED should be withdrawn by 20% decrements each week over a 4 week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial. Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets (Chewable, Dispersible):Table 1
The conversion regimen involves 4 steps outlined in . Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets (Chewable, Dispersible):Table 4
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients ≥ 16 Years of Age With Epilepsy Lamotrigine Valproate Step 1 Achieve a dose of 200 mg/day according to guidelines in (if not already on 200 mg/day). Table 1 Maintain previous stable dose. Step 2 Maintain at 200 mg/day. Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week. Step 3 Increase to 300 mg/day and maintain for 1 week. Simultaneously decrease to 250 mg/day and maintain for 1 week. Step 4 Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day. Discontinue.No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets (chewable, dispersible) with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate. Conversion From Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets (Chewable, Dispersible):
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine tablets (chewable, dispersible) is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets (chewable, dispersible) is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [ ]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets (chewable, dispersible) is introduced, based on concurrent medications, according to the regimen outlined in . If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets (chewable, dispersible) should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets (chewable, dispersible) should be doubled over a 2 week period in equal weekly increments (see ). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine tablets (chewable, dispersible) should remain constant for the first week and then should be decreased by half over a 2 week period in equal weekly decrements (see ). The dose of lamotrigine tablets (chewable, dispersible) may then be further adjusted to the target dose (200 mg) as clinically indicated. see Clinical Studies ( ) 14.2Table 5Table 6Table 6
If other drugs are subsequently introduced, the dose of lamotrigine tablets (chewable, dispersible) may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets (chewable, dispersible) [ ]. see Drug Interactions ( ), Clinical Pharmacology ( ) 712.3
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets (chewable, dispersible) should not be exceeded [see ]. Boxed Warning
Table 5. Escalation Regimen for Lamotrigine for Patients With Bipolar Disorder * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ ]. see Drug Interactions ( ), Clinical Pharmacology ( ) 712.3 † These drugs induce lamotrigine glucuronidation and increase clearance [ ]. Other drugs that have similar effects include estrogen-containing oral contraceptives [ ]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [ ]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. see Drug Interactions ( ), Clinical Pharmacology ( ) 712.3 see Drug Interactions ( ), Clinical Pharmacology ( ) 712.3 see Dosage and Administration ( ) 2.1 For Patients TAKING Valproate * For Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate †* For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone and NOT TAKING Valproate †* Weeks 1 and 2 25 mg every day other 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to Lamotrigine for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications * These drugs induce lamotrigine glucuronidation and increase clearance [ ]. Other drugs that have similar effects include estrogen-containing oral contraceptives [ ]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [ ]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. see Drug Interactions ( ), Clinical Pharmacology ( ) 712.3 see Drug Interactions ( ), Clinical Pharmacology ( ) 712.3 see Dosage and Administration ( ) 2.1 † Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ ]. see Drug Interactions ( ), Clinical Pharmacology ( ) 712.3Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate ) *†
After Discontinuation of Valproate † After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone * Current dose of Lamotrigine (mg/day) 100Current dose of Lamotrigine (mg/day)
400
Week 1 Maintain current dose of lamotrigine 150 400 Week 2 Maintain current dose of lamotrigine 200 300 Week 3 onward Maintain current dose of lamotrigine 200 200The benefit of continuing treatment in patients who had been stabilized in an 8 to 16 week open-label phase with lamotrigine tablets (chewable, dispersible) was established in 2 randomized, placebo-controlled clinical maintenance trials [ ]. However, the optimal duration of treatment with lamotrigine tablets (chewable, dispersible) has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment. see Clinical Studies ( ) 14.2
2.5 Administration of Lamotrigine Tablets (Chewable, Dispersible)Lamotrigine tablets (chewable, dispersible) may be swallowed whole, chewed, or dispersed in water or diluted fruit juice. If the tablets are chewed, consume a small amount of water or diluted fruit juice to aid in swallowing.
To disperse lamotrigine tablets (chewable, dispersible), add the tablets to a small amount of liquid (1 teaspoon, or enough to cover the medication). Approximately 1 minute later, when the tablets are completely dispersed, swirl the solution and consume the entire quantity immediately. No attempt should be made to administer partial quantities of the dispersed tablets.
-
Teva Pharmaceuticals Usa Inc
![Lamotrigine Tablet, Chewable [Teva Pharmaceuticals Usa Inc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Legacy Pharmaceutical Packaging
![Lamotrigine Tablet, Chewable [Teva Pharmaceuticals Usa Inc] Lamotrigine Tablet, Chewable [Teva Pharmaceuticals Usa Inc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Carvedilol should be taken with food to slow the rate of absorption and reduce the incidence of orthostatic effects.
2.1 Left Ventricular Dysfunction Following Myocardial Infarction:DOSAGE MUST BE INDIVIDUALIZED AND MONITORED DURING UP-TITRATION. Treatment with carvedilol tablets may be started as an inpatient or outpatient and should be started after the patient is hemodynamically stable and fluid retention has been minimized. It is recommended that carvedilol tablets be started at 6.25 mg twice daily and increased after 3 to 10 days, based on tolerability, to 12.5 mg twice daily, then again to the target dose of 25 mg twice daily. A lower starting dose may be used (3.125 mg twice daily) and/or the rate of up-titration may be slowed if clinically indicated (e.g., due to low blood pressure or heart rate, or fluid retention). Patients should be maintained on lower doses if higher doses are not tolerated. The recommended dosing regimen need not be altered in patients who received treatment with an IV or oral β-blocker during the acute phase of the myocardial infarction.
2.2 HypertensionDOSAGE MUST BE INDIVIDUALIZED. The recommended starting dose of carvedilol tablets is 6.25 mg twice daily. If this dose is tolerated, using standing systolic pressure measured about 1 hour after dosing as a guide, the dose should be maintained for 7 to 14 days, and then increased to 12.5 mg twice daily if needed, based on trough blood pressure, again using standing systolic pressure one hour after dosing as a guide for tolerance. This dose should also be maintained for 7 to 14 days and can then be adjusted upward to 25 mg twice daily if tolerated and needed. The full antihypertensive effect of carvedilol tablet is seen within 7 to 14 days. Total daily dose should not exceed 50 mg.
Concomitant administration with a diuretic can be expected to produce additive effects and exaggerate the orthostatic component of carvedilol action.
2.3 Hepatic ImpairmentCarvedilol tablets should not be given to patients with severe hepatic impairment [see CONTRAINDICATIONS (4)].
-
Teva Pharmaceuticals Usa Inc
![Lamotrigine Tablet [Teva Pharmaceuticals Usa Inc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Teva Pharmaceuticals Usa Inc
![Lamotrigine Tablet [Teva Pharmaceuticals Usa Inc] Lamotrigine Tablet [Teva Pharmaceuticals Usa Inc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash
There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation for lamotrigine tablets is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation
Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine. Drugs that induce glucuronidation include carbamazepine, phenytoin, phenobarbital, primidone, rifampin, estrogen-containing oral contraceptives, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Valproate inhibits glucuronidation. For dosing considerations for lamotrigine tablets in patients on estrogen-containing contraceptives and atazanavir/ritonavir, see below and Table 13. For dosing considerations for lamotrigine tablets in patients on other drugs known to induce or inhibit glucuronidation, see Table 1, Table 2, Table 5, Table 6, and Table 13.Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder
A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3)].Women Taking Estrogen-Containing Oral Contraceptives
Starting Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.Adjustments to the Maintenance Dose of Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: In women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be increased by as much as 2 fold over the recommended target maintenance dose to maintain a consistent lamotrigine plasma level.
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2 fold to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (pill-free week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the pill-free week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the pill-free week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: In women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2 week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. In women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy
The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2 fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.Patients Taking Atazanavir/Ritonavir
While atazanavir/ritonavir does reduce the lamotrigine plasma concentration, no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of atazanavir/ritonavir. Dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on concomitant AED or other concomitant medications (see Tables 1, 2 and 5). In patients already taking maintenance doses of lamotrigine tablets and not taking glucuronidation inducers, the dose of lamotrigine tablets may need to be increased if atazanavir/ritonavir is added, or decreased if atazanavir/ritonavir is discontinued [see Clinical Pharmacology (12.3)].Patients With Hepatic Impairment
Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 subjects with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.Patients With Renal Impairment
Initial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1 to 3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.Discontinuation Strategy
Epilepsy: For patients receiving lamotrigine tablets in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with bipolar disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these patients with bipolar disorder. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients older than 12 years and patients aged 2 to 12 years. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AEDs or other concomitant medications (see Table 1 for patients older than 12 years and Table 2for patients aged 2 to 12 years). A weight-based dosing guide for patients aged 2 to 12 years on concomitant valproate is provided in Table 3.
Patients Older Than 12 Years
Table 1. Escalation Regimen for Lamotrigine in Patients Older Than 12 Years With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration ( 2.1) ]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration ( 2.1), Drug Interactions (7), and Clinical Pharmacology (12.3) ].
Recommended dosing guidelines are summarized in Table 1.In Patients TAKING Valproate*
In Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate*
In Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate*
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day (in 2 divided doses)
Week 5 onward to maintenance
Increase by 25 to 50 mg/day every 1 to 2 weeks
Increase by 50 mg/day every 1 to 2 weeks
Increase by 100 mg/day every 1 to 2 weeks
Usual maintenance dose
100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses)
225 to 375 mg/day (in 2 divided doses)
300 to 500 mg/day
(in 2 divided doses)
Patients Aged 2 to 12 Years
Recommended dosing guidelines are summarized in Table 2.Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients Aged 2 to 12 Years With Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].In Patients TAKING Valproate*
In Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate*
In Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone†and NOT TAKING Valproate*
Weeks 1 and 2
0.15 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide)
0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet
0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet
Weeks 3 and 4
0.3 mg/kg/day in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide)
0.6 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet
1.2 mg/kg/day in 2 divided doses, rounded down to the nearest whole tablet
Week 5 onward to maintenance
The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose.
The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose.
The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose.
Usual maintenance dose
1 to 5 mg/kg/day (maximum 200 mg/day in 1 or 2 divided doses)
1 to 3 mg/kg/day with valproate alone4.5 to 7.5 mg/kg/day (maximum 300 mg/day in 2 divided doses)
5 to 15 mg/kg/day (maximum 400 mg/day in 2 divided doses)
Maintenance dose in patients less than 30 kg
May need to be increased by as much as 50%, based on clinical response.
May need to be increased by as much as 50%, based on clinical response.
May need to be increased by as much as 50%, based on clinical response.
Note: Only whole tablets should be used for dosing.
Table 3. The Initial Weight-Based Dosing Guide for Patients Aged 2 to 12 Years Taking Valproate (Weeks 1 to 4) With EpilepsyIf the patient’s weight is
Give this daily dose, using the most appropriate combination of lamotrigine, 2 and 5 mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
2.3 Epilepsy – Conversion From Adjunctive Therapy to Monotherapy
Usual Adjunctive Maintenance Dose for Epilepsy
The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive trials in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.The goal of the transition regimen is to attempt to maintain seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations for lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets
After achieving a dose of 500 mg/day of lamotrigine tablets using the guidelines in Table 1, the concomitant enzyme-inducing AED should be withdrawn by 20% decrements each week over a 4 week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine in Patients Aged 16 Years and Older With Epilepsy
The conversion regimen involves the 4 steps outlined in Table 4.Lamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1.
Maintain established stable dose.
Step 2
Maintain at 200 mg/day.
Decrease dose by decrements no greater than 500 mg/day/week to 500 mg/day and then maintain for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
2.4 Bipolar Disorder
Conversion From Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets
No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenytoin, phenobarbital, primidone, or valproate.The goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitor lopinavir/ritonavir that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2 week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2 week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine in Patients With Bipolar Disorder * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ see Drug Interactions (7), Clinical Pharmacology (12.3)] . † Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [ see Drug Interactions (7), Clinical Pharmacology (12.3)].In Patients TAKING Valproate*
In Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate†
In Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone†and NOT TAKING Valproate*
Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
Table 6. Dosage Adjustments to Lamotrigine in Patients With Bipolar Disorder Following Discontinuation of Psychotropic MedicationsDiscontinuation of Psychotropic Drugs (excluding Valproate*, Carbamazepine, Phenytoin, Phenobarbital, or Primidone†)
After Discontinuation of Valproate*
After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone†
Current dose of Lamotrigine (mg/day) 100
Current dose of Lamotrigine (mg/day)
400
Week 1
Maintain current dose of lamotrigine
150
400
Week 2
Maintain current dose of lamotrigine
200
300
Week 3 onward
Maintain current dose of lamotrigine
200
200
The benefit of continuing treatment in patients who had been stabilized in an 8 to 16 week open-label phase with lamotrigine tablets was established in 2 randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Remedyrepack Inc.
![Lamotrigine Tablet [Remedyrepack Inc. ] Lamotrigine Tablet [Remedyrepack Inc. ]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Dosing is based on concomitant medications, indication, and patient age. ( 2.2 , 2.4 ) To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations should not be exceeded. ( 2.1 ) Do not restart lamotrigine in patients who discontinued due to rash unless the potential benefits clearly outweigh the risks. ( 2.1 ) Adjustments to maintenance doses will in most cases be required in patients starting or stopping estrogen-containing oral contraceptives. ( 2.1 , 5.8 ) Lamotrigine tablets should be discontinued over a period of at least 2 weeks (approximately 50% reduction per week). ( 2.1 , 5.9 )Epilepsy
Adjunctive therapy—See Table 1 for patients >12 years of age and Tables 2 and 3 for patients 2 to 12 years. ( 2.2 ) Conversion to monotherapy—See Table 4. ( 2.3 )Bipolar Disorder: See Tables 5 and 6 ( 2.4 )
Rash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning ]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablet is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3) ].
Lamotrigine Tablets Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3) ] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets may require adjustment based on clinical response.
Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3) ].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3) ], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets In Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3) ].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3) ]. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6) , Clinical Pharmacology (12.3) ], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7) , Clinical Pharmacology (12.3) ]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.
Discontinuation Strategy:
Epilepsy: For patients receiving lamotrigine tablets in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9) ].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9) ].
This section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Patients Over 12 Years of Age: Recommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine Tablets in Patients Over 12 Years of Age With Epilepsy
For
For Patients NOT TAKING
For Patients
Patients
Carbamazepine,
TAKING
TAKING
Phenytoin,
Carbamazepine,
Valproatea
Phenobarbital,
Phenytoin,
or Primidoneb,
Phenobarbital,
or Valproatea
or Primidoneb
and NOT TAKING
Valproatea
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Weeks 5 onwards to
maintenance
Increase by 25 to
50 mg/day every 1 to 2 weeks
Increase by 50
mg/day every 1
to 2 weeks
Increase by
100 mg/day every
1 to 2 weeks.
Usual maintenance
dose
100 to 200 mg/day
with valproate alone
225 to 375 mg/day
(in 2 divided doses).
300 to 500 mg/day
(in 2 divided doses).
100 to 400 mg/day
with valproate
and other drugs that induce glucuronidation
(in 1 or 2 divided doses)
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Patients 2 to 12 Years Of Age: Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine Tablets in Patients 2 to 12 Years of Age With Epilepsy
For Patients TAKING
Valproatea
For Patients NOT
TAKING Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea
For Patients TAKING
Carbamazepine, Phenytoin, Phenobarbital, or
Primidoneb and NOT
TAKING Valproatea
Weeks 1 and 2
0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the
nearest whole tablet (see Table 3 for weight
based dosing guide).
0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the
nearest whole tablet.
0.6 mg/kg/day
in 2 divided doses, rounded down to the
nearest whole tablet.
Weeks 3 and 4
0.3 mg/kg/day
in 1 or 2 divided doses,
rounded down to the
nearest whole tablet
(see Table 3 for weight
based dosing guide).
0.6 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet.
1.2 mg/kg/day
in 2 divided doses,
rounded down to the
nearest whole tablet.
Weeks 5
onwards to
maintenance
The dose should be increased every
1 to 2 weeks as follows:
calculate 0.3 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose.
The dose should be increased every
1 to 2 weeks as follows:
calculate 0.6 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose
The dose should be increased every
1 to 2 weeks as follows:
calculate 1.2 mg/kg/day, round this amount
down to the nearest whole tablet, and
add this amount to the
previously administered daily dose
Usual
Maintenance
Dose
1 to 5 mg/kg/day
(maximum 200 mg/day
in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone
4.5 to 7.5 mg/kg/day
(maximum 300 mg/day
in 2 divided doses)
5 to 15 mg/kg/day
(maximum 400 mg/day
in 2 divided doses)
Maintenance dose in
patients
less than 30 kg
May need to be increased
by as much as 50%,
based on clinical response
May need to be increased
by as much as 50%,
based on clinical response
May need to be increased
by as much as 50%, based
on clinical response
Note: Only whole tablets should be used for dosing.
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is
Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy: The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
The goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in two divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets: After achieving a dose of 500 mg/day of lamotrigine tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets:
The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets in Patients ≥16 Years of Age with Epilepsy
Lamotrigine Tablets
Valproate
Step 1
Achieve a dose of 200 mg/day according to
guidelines in Table 1
(if not already on 200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than
500 mg/day/week and then maintain the dose of
500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to
250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every
week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets: No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate.
The goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2) ]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7) , Clinical Pharmacology (12.3) ].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning ].
Table 5. Escalation Regimen for Lamotrigine Tablets for Patients With Bipolar Disorder
For Patients TAKING
Valproatea
For Patients NOT TAKING
Carbamazepine, Phenytoin, Phenobarbital,
Primidoneb, or Valproatea
For Patients TAKING
Carbamazepine, Phenytoin,
Phenobarbital, or Primidoneb and NOT TAKING
Valproatea
Weeks 1 and 2
25 mg every
other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b These drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
Table 6. Dosage Adjustments to Lamotrigine Tablets for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications
Discontinuation of Psychotropic Drugs
(excluding Carbamazepine, Phenytoin,
Phenobarbital, Primidoneb, or
Valproatea)
After Discontinuation of
Valproatea
After Discontinuation of
Carbamazepine, Phenytoin,
Phenobarbital, or Primidoneb
Current dose of lamotrigine tablets
(mg/day)
100
Current dose of lamotrigine tablets
(mg/day)
400
Week 1
Maintain current dose of lamotrigine tablets
150
400
Week 2
Maintain current dose of lamotrigine tablets
200
300
Week 3 onward
Maintain current dose of lamotrigine tablets
200
200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine tablets was established in two randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2) ]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Jubilant Cadista Pharmaceuticals, Inc.
![Lamotrigine (Lamotrigine) Tablet [Jubilant Cadista Pharmaceuticals, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Jubilant Cadista Pharmaceuticals, Inc.
![Lamotrigine (Lamotrigine) Tablet [Jubilant Cadista Pharmaceuticals, Inc.] Lamotrigine (Lamotrigine) Tablet [Jubilant Cadista Pharmaceuticals, Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsRash
There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine with valproate, (2) exceeding the recommended initial dose of lamotrigine, or (3) exceeding the recommended dose escalation for Lamotrigine. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation for lamotrigine is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued Lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Added to Drugs Known to Induce or Inhibit Glucuronidation
Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine. Drugs that induce glucuronidation include carbamazepine, phenytoin, phenobarbital, primidone, rifampin, estrogen-containing oral contraceptives, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Valproate inhibits glucuronidation. For dosing considerations for Lamotrigine in patients on estrogen-containing contraceptives and atazanavir/ritonavir, see below and Table 13. For dosing considerations for Lamotrigine in patients on other drugs known to induce or inhibit glucuronidation, see Tables 1, 2, 5-6, and 13.Target Plasma Levels for Patients with Epilepsy or Bipolar Disorder
A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of Lamotrigine should be based on therapeutic response [see Clinical Pharmacology (12.3)].Women Taking Estrogen-Containing Oral Contraceptives
Starting Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for Lamotrigine should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with Lamotrigine based on the concomitant AED or other concomitant medications (see Tables 1, 5, and 7). See below for adjustments to maintenance doses of Lamotrigine in women taking estrogen-containing oral contraceptives.Adjustments to the Maintenance Dose of Lamotrigine in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: In women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be increased by as much as 2-fold over the recommended target maintenance dose to maintain a consistent lamotrigine plasma level.
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of Lamotrigine and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Tables 1 and 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (pill-free week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to Lamotrigine consistently occur during the pill-free week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the pill-free week are not recommended. For women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of Lamotrigine should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: In women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of Lamotrigine should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. In women taking Lamotrigine in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of Lamotrigine should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy
The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of Lamotrigine in the presence of progestogens alone will likely not be needed.Patients Taking Atazanavir/Ritonavir
While atazanavir/ritonavir does reduce the lamotrigine plasma concentration, no adjustments to the recommended dose-escalation guidelines for Lamotrigine should be necessary solely based on the use of atazanavir/ritonavir. Dose escalation should follow the recommended guidelines for initiating adjunctive therapy with Lamotrigine based on concomitant AED or other concomitant medications (see Tables 1, 2, and 5). In patients already taking maintenance doses of Lamotrigine and not taking glucuronidation inducers, the dose of Lamotrigine may need to be increased if atazanavir/ritonavir is added, or decreased if atazanavir/ritonavir is discontinued [see Clinical Pharmacology (12.3)].Patients with Hepatic Impairment
Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 subjects with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.Patients with Renal Impairment
Initial doses of Lamotrigine should be based on patients' concomitant medications (see Tables 1-3 and 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine. Because there is inadequate experience in this population, lamotrigine should be used with caution in these patients.Discontinuation Strategy
Epilepsy: For patients receiving lamotrigine in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.If a decision is made to discontinue therapy with lamotrigine, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.8)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine. In the clinical development program in adults with bipolar disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine. Discontinuation of lamotrigine should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.8)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients older than 12 years and patients aged 2 to 12 years. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AEDs or other concomitant medications (see Table 1 for patients older than 12 years and Table 2 for patients aged 2 to 12 years). A weight-based dosing guide for patients aged 2 to 12 years on concomitant valproate is provided in Table 3.
Patients Older than 12 Years
Table 1 Escalation Regimen for Lamotrigine in Patients Older than 12 Years with Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions ( 7 ), Clinical Pharmacology ( 12.3 )]. † Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)]. In Patients TAKING Valproate* In Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†,or Valproate* In Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Weeks 1 and 2 25 mg every other day 25 mg every day 50 mg/day Weeks 3 and 4 25 mg every day 50 mg/day 100 mg/day
Recommended dosing guidelines are summarized in Table 1.
(in 2 divided doses) Week 5 onward to maintenance Increase by 25 to 50 mg/day every 1 to 2 weeks. Increase by 50 mg/day
every 1 to 2 weeks. Increase by 100 mg/day every 1 to 2 weeks. Usual maintenance dose 100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation
(in 1 or 2 divided doses) 225 to 375 mg/day
(in 2 divided doses) 300 to 500 mg/day
(in 2 divided doses)Patients Aged 2 to 12 Years
Recommended dosing guidelines are summarized in Table 2.Lower starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by lower starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine in Patients Aged 2 to 12 Years with Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)]. In Patients TAKING Valproate* In Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone† or
Valproate* In Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Weeks 1 and 2 0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide) 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Weeks 3 and 4 0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide) 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet 1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet Week 5 onward to maintenance The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose. The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose. The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose. Usual maintenance dose 1 to 5 mg/kg/day
(maximum 200 mg/day in 1 or 2 divided doses)
1 to 3 mg/kg/day with valproate alone 4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 5 to 15 mg/kg/day
(maximum 400 mg/day in 2 divided doses) Maintenance dose in patients less than 30 kg May need to be increased by as much as 50%, based on clinical response. May need to be increased by as much as 50%, based on clinical response. May need to be increased by as much as 50%, based on clinical response. Note: Only whole tablets should be used for dosing. Table 3. The Initial Weight-Based Dosing Guide for Patients Aged 2 to 12 Years Taking Valproate (Weeks 1 to 4) with Epilepsy If the patient’s weight is Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets Greater than And less than Weeks 1 and 2 Weeks 3 and 4 6.7 kg 14 kg 2 mg every other day 2 mg every day 14.1 kg 27 kg 2 mg every day 4 mg every day 27.1 kg 34 kg 4 mg every day 8 mg every day 34.1 kg 40 kg 5 mg every day 10 mg every dayUsual Adjunctive Maintenance Dose for Epilepsy
2.3 Epilepsy – Conversion from Adjunctive Therapy to Monotherapy
The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive trials in which the efficacy of lamotrigine was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1- 4 has not been established in controlled trials.The goal of the transition regimen is to attempt to maintain seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine.
The recommended maintenance dose of lamotrigine as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations for lamotrigine should not be exceeded [see Boxed Warning].
Conversion from Adjunctive Therapy with Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy with Lamotrigine
After achieving a dose of 500 mg/day of lamotrigine using the guidelines in Table 1, the concomitant enzyme-inducing AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.Conversion from Adjunctive Therapy with Valproate to Monotherapy with Lamotrigine
Table 4. Conversion from Adjunctive Therapy with Valproate to Monotherapy with Lamotrigine in Patients Aged 16 Years and Older with Epilepsy
The conversion regimen involves the 4 steps outlined in Table 4.Lamotrigine
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1.
Maintain established stable dose.
Step 2
Maintain at 200 mg/day.
Decrease dose by decrements no greater than 500 mg/day/week to 500 mg/day and then maintain for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy with Antiepileptic Drugs other than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy with Lamotrigine
2.4 Bipolar Disorder
No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine with AEDs other than carbamazepine, phenytoin, phenobarbital, primidone, or valproate.The goal of maintenance treatment with lamotrigine is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy [see Indications and Usage (1)].
Patients taking Lamotrigine for more than 16 weeks should be periodically reassessed to determine the need for maintenance treatment.
Adults
The target dose of lamotrigine is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitor lopinavir/ritonavir that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended.
Treatment with lamotrigine is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine should be adjusted. In patients discontinuing valproate, the dose of lamotrigine should be doubled over a 2-week period in equal weekly increments (see Table 6). In patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation, the dose of lamotrigine should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of Lamotrigine should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine in Adults with Bipolar Disorder * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)]. In Patients TAKING Valproate* In Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate* In Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate* Weeks 1 and 2 25 mg every other day 25 mg daily 50 mg daily Weeks 3 and 4 25 mg daily 50 mg daily 100 mg daily, in divided doses Week 5 50 mg daily 100 mg daily 200 mg daily, in divided doses Week 6 100 mg daily 200 mg daily 300 mg daily, in divided doses Week 7 100 mg daily 200 mg daily up to 400 mg daily, in divided doses Table 6. Dosage Adjustments to Lamotrigine in Adults with Bipolar Disorder Following Discontinuation of Psychotropic Medications * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)]. Discontinuation of Psychotropic Drugs (excluding Valproate *Carbamazepine, Phenytoin, Phenobarbital, Primidone†) After Discontinuation of Valproate* After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone† Current dose of lamotrigine (mg/day) 100Current dose of lamotrigine (mg/day) 400
Week 1 Maintain current dose of Lamotrigine 150 400 Week 2 Maintain current dose of Lamotrigine 200 300 Week 3 onward Maintain current dose of Lamotrigine 200 200 -
Mylan Pharmaceuticals Inc.
![Lamotrigine Tablet [Mylan Pharmaceuticals Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Mylan Pharmaceuticals Inc.
![Lamotrigine Tablet [Mylan Pharmaceuticals Inc.] Lamotrigine Tablet [Mylan Pharmaceuticals Inc.]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing Considerations RashThere are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation for lamotrigine tablets is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine tablets, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine tablets for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Tablets Added to Drugs Known to Induce or Inhibit GlucuronidationBecause lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine. Drugs that induce glucuronidation include carbamazepine, phenytoin, phenobarbital, primidone, rifampin, estrogen-containing oral contraceptives, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Valproate inhibits glucuronidation. For dosing considerations for lamotrigine tablets in patients on estrogen-containing contraceptives and atazanavir/ritonavir, see below and Table 13. For dosing considerations for lamotrigine tablets in patients on other drugs known to induce or inhibit glucuronidation, see Table 1, Table 2, Table 5, Table 6, and Table 13.
Target Plasma Levels for Patients with Epilepsy or Bipolar DisorderA therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women taking Estrogen-Containing Oral Contraceptives Starting Lamotrigine Tablets in Women taking Estrogen-Containing Oral ContraceptivesAlthough estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Tablets in Women taking Estrogen-Containing Oral Contraceptives (1) Taking Estrogen-Containing Oral ContraceptivesIn women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be increased by as much as 2-fold over the recommended target maintenance dose to maintain a consistent lamotrigine plasma level.
(2) Starting Estrogen-Containing Oral ContraceptivesIn women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (pill-free week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the pill-free week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the pill-free week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
(3) Stopping Estrogen-Containing Oral ContraceptivesIn women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. In women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation[see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement TherapyThe effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.
Patients Taking Atazanavir/RitonavirWhile atazanavir/ritonavir does reduce the lamotrigine plasma concentration, no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of atazanavir/ritonavir. Dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on concomitant AED or other concomitant medications (see Tables 1, 2, and 5). In patients already taking maintenance doses of lamotrigine tablets and not taking glucuronidation inducers, the dose of lamotrigine tablets may need to be increased if atazanavir/ritonavir is added, or decreased if atazanavir/ritonavir is discontinued [see Clinical Pharmacology (12.3)].
Patients with Hepatic ImpairmentExperience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 subjects with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients with Renal ImpairmentInitial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1 to 3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.
Discontinuation Strategy EpilepsyFor patients receiving lamotrigine tablets in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar DisorderIn the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with bipolar disorder, two patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these patients with bipolar disorder. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.9)].
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients older than 12 years and patients aged 2 to 12 years. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AEDs or other concomitant medications (see Table 1 for patients older than 12 years and Table 2 for patients aged 2 to 12 years). A weight-based dosing guide for patients aged 2 to 12 years on concomitant valproate is provided in Table 3.
Patients Older than 12 YearsRecommended dosing guidelines are summarized in Table 1.
Table 1. Escalation Regimen for Lamotrigine Tablets in Patients Older than 12 Years with Epilepsy * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)].In Patients TAKING Valproate*
In Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate*
In Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate*
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)Week 5 onward
to maintenance
Increase by 25 to
50 mg/day every
1 to 2 weeks.Increase by
50 mg/day every
1 to 2 weeks.Increase by
100 mg/day every
1 to 2 weeks.Usual maintenance
dose100 to 200 mg/day with valproate alone
100 to 400 mg/day with valproate and other drugs that induce glucuronidation(in 1 or 2 divided doses)
225 to 375 mg/day
(in 2 divided doses)300 to 500 mg/day
Patients Aged 2 to 12 Years
(in 2 divided doses)Recommended dosing guidelines are summarized in Table 2.
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine Tablets in Patients Aged 2 to 12 Years with Epilepsy Note: Only whole tablets should be used for dosing. * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)].In Patients TAKING
Valproate*
In Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate*
In Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate*
Weeks 1 and 2
0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide)0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tabletWeeks 3 and 4
0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide)
0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tabletWeek 5
onward to
maintenance
The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose.
The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose.
The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose.
Usual
maintenance
dose
1 to 5 mg/kg/day
(maximum 200 mg/day in 1 or 2 divided doses)
1 to 3 mg/kg/day with valproate alone4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses)5 to 15 mg/kg/day
(maximum 400 mg/day in 2 divided doses)Maintenance
dose in
patients less
than 30 kg
May need to be increased by as much as 50%, based
on clinical response.May need to be increased by as much as 50%, based on clinical response.
May need to be increased by as much as 50%, based on clinical response.
Table 3. The Initial Weight-Based Dosing Guide for Patients Aged 2 to 12 Years Taking Valproate (Weeks 1 to 4) with EpilepsyIf the patient’s weight is
Give this daily dose, using the most appropriate combination of lamotrigine 2 mg and 5 mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for EpilepsyThe usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive trials in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate, maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone, maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials.
2.3 Epilepsy – Conversion from Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to attempt to maintain seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in two divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations for lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion from Adjunctive Therapy with Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy with Lamotrigine TabletsAfter achieving a dose of 500 mg/day of lamotrigine tablets using the guidelines in Table 1, the concomitant enzyme-inducing AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy with Valproate to Monotherapy with Lamotrigine TabletsThe conversion regimen involves the four steps outlined in Table 4.
Table 4. Conversion from Adjunctive Therapy with Valproate to Monotherapy with Lamotrigine Tablets in Patients Aged 16 Years and Older with EpilepsyLamotrigine Tablets
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1.
Maintain established stable dose.
Step 2
Maintain at 200 mg/day.
Decrease dose by decrements no greater than 500 mg/day/week to 500 mg/day and then maintain for one week.
Step 3
Increase to 300 mg/day and maintain for one week.
Simultaneously decrease to 250 mg/day and maintain for one week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy with Antiepileptic Drugs Other than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy with Lamotrigine TabletsNo specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenytoin, phenobarbital, primidone, or valproate.
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitor lopinavir/ritonavir that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Table 5. Escalation Regimen for Lamotrigine Tablets in Patients with Bipolar Disorder * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)].In Patients TAKING Valproate*
In Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidone†, or Valproate*
In Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidone† and NOT TAKING Valproate*
Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 *mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
Table 6. Dosage Adjustments to Lamotrigine Tablets in Patients with Bipolar Disorder Following Discontinuation of Psychotropic Medications * Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)]. † Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)].Discontinuation of Psychotropic Drugs (excluding Valproate*, Carbamazepine, Phenytoin, Phenobarbital, or Primidone†)
After Discontinuation of Valproate*
After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidone†
Current dose of lamotrigine tablets (mg/day) 100
Current dose of lamotrigine tablets (mg/day)
400
Week 1
Maintain current dose of lamotrigine tablets
150
400
Week 2
Maintain current dose of lamotrigine tablets
200
300
Week 3 onward
Maintain current dose of lamotrigine tablets
200
200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine tablets was established in two randomized, placebo-controlled clinical maintenance trials [see Clinical Studies (14.2)]. However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment.
-
Torrent Pharmaceuticals Limited
![Lamotrigine Tablet, Extended Release [Torrent Pharmaceuticals Limited]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Torrent Pharmaceuticals Limited
![Lamotrigine Tablet, Extended Release [Torrent Pharmaceuticals Limited] Lamotrigine Tablet, Extended Release [Torrent Pharmaceuticals Limited]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine extended-release tablets are taken once daily, with or without food. Tablets must be swallowed whole and must not be chewed, crushed, or divided.
2.1 General Dosing ConsiderationsRash: There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine extended-release tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine extended-release tablets, or (3) exceeding the recommended dose escalation for lamotrigine extended-release tablets. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation for lamotrigine extended-release tablets is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine extended-release tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine extended-release tablets, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Extended-Release Tablets Added to Drugs Known to Induce or Inhibit Glucuronidation: Drugs other than those listed in the Clinical Pharmacology section [see Clinical Pharmacology (12.3)] have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine extended-release tablets may require adjustment based on clinical response.
Target Plasma Levels: A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine extended-release tablets should be based on therapeutic response [see Clinical Pharmacology (12.3)].
Women Taking Estrogen-Containing Oral Contraceptives: Starting Lamotrigine Extended-Release Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine extended-release tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine extended-release tablets based on the concomitant AED or other concomitant medications (see Table 1). See below for adjustments to maintenance doses of lamotrigine extended-release tablets in women taking estrogen-containing oral contraceptives.
Adjustments to the Maintenance Dose of Lamotrigine Extended-Release Tablets in Women Taking Estrogen-Containing Oral Contraceptives:
(1) Taking Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine extended-release tablets will in most cases need to be increased by as much as 2-fold over the recommended target maintenance dose in order to maintain a consistent lamotrigine plasma level [see Clinical Pharmacology (12.3)].
(2) Starting Estrogen-Containing Oral Contraceptives: In women taking a stable dose of lamotrigine extended-release tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (pill-free week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine extended-release tablets consistently occur during the pill-free week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the pill-free week are not recommended. For women taking lamotrigine extended-release tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine extended-release tablets should be necessary.
(3) Stopping Estrogen-Containing Oral Contraceptives: For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine extended-release tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine extended-release tablets should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. For women taking lamotrigine extended-release tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine extended-release tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy: The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine extended-release tablets in the presence of progestogens alone will likely not be needed.
Patients With Hepatic Impairment: Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)], the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients With Renal Impairment: Initial doses of lamotrigine extended-release tablets should be based on patients' concomitant medications (see Table 1); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with immediate-release lamotrigine. Because there is inadequate experience in this population, lamotrigine extended-release tablets should be used with caution in these patients.
Discontinuation Strategy: For patients receiving lamotrigine extended-release tablets in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.
If a decision is made to discontinue therapy with lamotrigine extended-release tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.8)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
2.2 Adjunctive Therapy for Primary Generalized Tonic-Clonic and Partial Onset SeizuresThis section provides specific dosing recommendations for patients ≥13 years of age. Specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications.
Table 1. Escalation Regimen for Lamotrigine Extended-Release Tablets in Patients ≥13 Years of AgeaValproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
bThese drugs induce lamotrigine glucuronidation and increase clearance [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see Drug Interactions (7), Clinical Pharmacology (12.3)]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect.
cDose increases at week 8 or later should not exceed 100 mg daily at weekly intervals.
For Patients
TAKING Valproatea
For Patients NOT TAKING Carbamazepine,
Phenytoin,
Phenobarbital,
Primidone,b or
Valproatea
For Patients TAKING Carbamazepine,
Phenytoin,
Phenobarbital, or
Primidoneb and
NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg every day
Weeks 3 and 4
25 mg every day
50 mg every day
100 mg every day
Week 5
50 mg every day
100 mg every day
200 mg every day
Week 6
100 mg every day
150 mg every day
300 mg every day
Week 7
150 mg every day
200 mg every day
400 mg every day
Maintenance range
(week 8 and onward)
200 to 250 mg every dayc
300 to 400 mg every dayc
400 to 600 mg every dayc
2.3 Conversion From Adjuctive Therapy to MonotherapyThe goal of the transition regimen is to attempt to maintain seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine extended-release tablets.
The recommended maintenance dosage range of lamotrigine extended-release tablets as monotherapy is 250 to 300 mg given once daily.
The recommended initial dose and subsequent dose escalations for lamotrigine extended-release tablets should not be exceeded [see Boxed Warning].
Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Extended-Release Tablets: After achieving a dosage of 500 mg/day of lamotrigine extended-release tablets using the guidelines in Table 1, the concomitant enzyme-inducing AED should be withdrawn by 20% decrements each week over a 4-week period. Two weeks after completion of withdrawal of the enzyme-inducing AED, the dosage of lamotrigine extended-release tablets may be decreased no faster than 100 mg/day each week to achieve the monotherapy maintenance dosage range of 250 to 300 mg/day.
The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial using immediate-release lamotrigine.
Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Extended-Release Tablets: The conversion regimen involves the 4 steps outlined in Table 2.
Table 2. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Extended-Release Tablets in Patients ≥13 Years of Age With Epilepsy
Lamotrigine extended-release tablets
Valproate
Step 1
Achieve a dosage of 150 mg/day according to guidelines in Table 1.
Maintain established stable dose.
Step 2
Maintain at 150 mg/day1
Decrease dosage by decrements no greater than 500 mg/day/week to 500 mg/day and then maintain for 1 week.
Step 3
Increase to 200 mg/day.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase to 250 or 300 mg/day.
Discontinue.
Conversion From Adjunctive Therapy With Antiepileptic Drugs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Extended-Release Tablets: After achieving a dosage of 250 to 300 mg/day of lamotrigine extended-release tablets using the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. No adjustment to the monotherapy dose of lamotrigine extended-release tablets is needed.
2.4 Conversion From Immediate-Release Lamotrigine Tablets to Lamotrigine Extended-Release TabletsPatients may be converted directly from immediate-release lamotrigine to lamotrigine extended-release tablets. The initial dose of lamotrigine extended-release tablets should match the total daily dose of immediate-release lamotrigine. However, some subjects on concomitant enzyme-inducing agents may have lower plasma levels of lamotrigine on conversion and should be monitored [see Clinical Pharmacology (12.3)].
Following conversion to lamotrigine extended-release tablets, all patients (but especially those on drugs that induce lamotrigine glucuronidation) should be closely monitored for seizure control [see Drug Interactions (7)]. Depending on the therapeutic response after conversion, the total daily dose may need to be adjusted within the recommended dosing instructions (Table 1).
-
Cipla Limited
![Lamotrigine Tablet [Cipla Limited]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Perrigo New York Inc
![Lamotrigine Tablet [Cipla Limited] Lamotrigine Tablet [Cipla Limited]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
• do not take more than directed (see overdose warning)adults and children 12 years and over
• take 2 caplets every 6 hours while symptoms last • do not take more than 6 caplets in 24 hours, unless directed by a doctor • do not use for more than 10 days unless directed by a doctorchildren under 12 years
ask a doctor
-
Tya Pharmaceuticals
![Lamotrigine Tablet [Tya Pharmaceuticals]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Tya Pharmaceuticals
![Lamotrigine Tablet [Tya Pharmaceuticals] Lamotrigine Tablet [Tya Pharmaceuticals]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1 General Dosing ConsiderationsThere are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors Therefore, it is important that the dosing recommendations be followed closely. Rash:[see ]. Boxed Warning
The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation of lamotrigine tablet is exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see ]. Clinical Pharmacology (12.3)
Drugs other than those listed in the Clinical Pharmacology section have not been systematically evaluated in combination with lamotrigine. Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine and doses of lamotrigine tablets may require adjustment based on clinical response. Lamotrigine Tablets Added to Drugs Known to Induce or Inhibit Glucuronidation:[see ] Clinical Pharmacology (12.3)
A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response Target Plasma Levels for Patients With Epilepsy or Bipolar Disorder:[see ]. Clinical Pharmacology (12.3)
Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1 or Table 5). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives. Women Taking Estrogen-Containing Oral Contraceptives:Starting Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives:[see ], Clinical Pharmacology (12.3)
Adjustments to the Maintenance Dose of Lamotrigine Tablets In Women Taking Estrogen-Containing Oral Contraceptives:
For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation the maintenance dose of lamotrigine tablets will in most cases need to be increased, by as much as 2-fold over the recommended target maintenance dose, in order to maintain a consistent lamotrigine plasma level (1) Taking Estrogen-Containing Oral Contraceptives:[see , ], Drug Interactions (7)Clinical Pharmacology (12.3)[see ]. Clinical Pharmacology (12.3)
In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation the maintenance dose will in most cases need to be increased by as much as 2-fold in order to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Table 1 or Table 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation ("pill-free" week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the "pill-free" week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the "pill-free" week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation no adjustment to the dose of lamotrigine tablets should be necessary. (2) Starting Estrogen-Containing Oral Contraceptives:[see , ], Drug Interactions (7)Clinical Pharmacology (12.3)[see , ], Drug Interactions (7)Clinical Pharmacology (12.3)
For women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50% in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation no adjustment to the dose of lamotrigine tablets should be necessary. (3) Stopping Estrogen-Containing Oral Contraceptives:[see , ], Drug Interactions (7)Clinical Pharmacology (12.3)[see ]. Clinical Pharmacology (12.3)[see , ], Drug Interactions (7)Clinical Pharmacology (12.3)
The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed. Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy:
Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 patients with mild, moderate, and severe liver impairment the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response. Patients With Hepatic Impairment:[see , ], Use in Specific Populations (8.6)Clinical Pharmacology (12.3)
Initial doses of lamotrigine tablets should be based on patients' concomitant medications (see Tables 1-3 or Table 5); reduced maintenance doses may be effective for patients with significant renal impairment Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients. Patients With Renal Impairment:[see , ]. Use in Specific Populations (8.7)Clinical Pharmacology (12.3)
Discontinuation Strategy:
For patients receiving lamotrigine tablets in combination with other AEDs, a reevaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed. Epilepsy:
If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see ]. Warnings and Precautions (5.9)
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone or other drugs such as rifampin that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In clinical trials in patients with Bipolar Disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. However, there were confounding factors that may have contributed to the occurrence of seizures in these bipolar patients. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal Bipolar Disorder:[see ]. Warnings and Precautions (5.9)
2.2 Epilepsy – Adjunctive TherapyThis section provides specific dosing recommendations for patients greater than 12 years of age and patients 2 to 12 years of age. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AED or other concomitant medications (Table 1 for patients greater than 12 years of age and Table 2 for patients 2 to 12 years of age). A weight-based dosing guide for patients 2 to 12 years of age on concomitant valproate is provided in Table 3.
Recommended dosing guidelines are summarized in Table 1. Patients Over 12 Years of Age:
Table 1. Escalation Regimen for Lamotrigine Tablets in Patients Over 12 Years of Age With Epilepsya Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see , ]. Drug Interactions (7)Clinical Pharmacology (12.3)
b These drugs induce lamotrigine glucuronidation and increase clearance [see , ]. Other drugs that have similar effects include estrogen-containing oral contraceptives [see , ]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see ]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. Drug Interactions (7)Clinical Pharmacology (12.3)Drug Interactions (7)Clinical Pharmacology (12.3)Dosage and Administration (2.1)
For
For Patients NOT TAKING
For Patients
Patients
Carbamazepine,
TAKING
TAKING
Phenytoin,
Carbamazepine,
Valproate a
Phenobarbital,
Phenytoin,
or Primidone b,
Phenobarbital,
or Valproate a
or Primidone b
and NOT TAKING
Valproate a
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
(in 2 divided doses) 100 mg/day
Weeks 5 onwards to maintenance
Increase by 25 to 50 mg/day every 1 to 2 weeks
Increase by 50 mg/day every 1 to 2 weeks
Increase by 100 mg/day every 1 to 2 weeks.
Usual maintenance dose
100 to 200 mg/day
with valproate alone
(in 2 divided doses). 225 to 375 mg/day
(in 2 divided doses). 300 to 500 mg/day
100 to 400 mg/day
with valproate
and other drugs that induce glucuronidation
(in 1 or 2 divided doses)
Recommended dosing guidelines are summarized in Table 2. Patients 2 to 12 Years Of Age:
Smaller starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by smaller starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2. Escalation Regimen for Lamotrigine Tablets in Patients 2 to 12 Years of Age With EpilepsyNote:Onlywholetabletsshouldbeusedfordosing.
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see , ]. Drug Interactions (7)Clinical Pharmacology (12.3)
b These drugs induce lamotrigine glucuronidation and increase clearance [see , ]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see , ]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see ]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. Drug Interactions (7)Clinical Pharmacology (12.3)Drug Interactions (7)Clinical Pharmacology (12.3)Dosage and Administration (2.1)
For Patients TAKING
Valproate a
For Patients NOT
TAKING Carbamazepine, Phenytoin,
Phenobarbital, Primidone b, or
Valproate a
For Patients TAKING
Carbamazepine, Phenytoin, Phenobarbital, or
Primidone band NOT
TAKING Valproate a
Weeks 1 and 2
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide). 0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet. 0.3 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet. 0.6 mg/kg/day
Weeks 3 and 4
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight based dosing guide). 0.3 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet. 0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet. 1.2 mg/kg/day
Weeks 5 onwards to maintenance
The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose.
The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
Usual Maintenance Dose
(maximum 200 mg/day in 1 or 2 divided doses). with valproate alone 1 to 5 mg/kg/day
1 to 3 mg/kg/day
(maximum 300 mg/day in 2 divided doses) 4.5 to 7.5 mg/kg/day
(maximum 400 mg/day in 2 divided doses) 5 to 15 mg/kg/day
Maintenance dose in patients less than 30 kg
May need to be increased by as much as 50%, based on clinical response
May need to be increased by as much as 50%, based on clinical response
May need to be increased by as much as 50%, based on clinical response
Table 3. The Initial Weight-Based Dosing Guide for Patients 2 to 12 Years Taking Valproate (Weeks 1 to 4) With Epilepsy If the patient’s weight is
Give this daily dose, using the most appropriate combination of Lamotrigine 2-mg and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every day other
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive studies in which the efficacy of lamotrigine tablets was established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone , maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving , maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 through 4 has not been established in controlled trials. Usual Adjunctive Maintenance Dose for Epilepsy:without valproatevalproate alone
2.3 Epilepsy – Conversion From Adjunctive Therapy to MonotherapyThe goal of the transition regimen is to effect the conversion to monotherapy with lamotrigine tablets under conditions that ensure adequate seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in two divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see ]. Boxed Warning
After achieving a dose of 500 mg/day of lamotrigine tablets according to the guidelines in Table 1, the concomitant AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial. Conversion From Adjunctive Therapy With Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy With Lamotrigine Tablets:
Conversion from Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets:
The conversion regimen involves 4 steps outlined in Table 4.
Table 4. Conversion From Adjunctive Therapy With Valproate to Monotherapy With Lamotrigine Tablets in Patients ≥16 Years of Age with Epilepsy
Lamotrigine Tablets
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1 (if not already on 200 mg/day).
Maintain previous stable dose.
Step 2
Maintain at 200 mg/day.
Decrease to 500 mg/day by decrements no greater than 500 mg/day/week and then maintain the dose of 500 mg/day for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenobarbital, phenytoin, primidone, or valproate. Conversion from Adjunctive Therapy With AEDs Other Than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy With Lamotrigine Tablets:
2.4 Bipolar DisorderThe goal of maintenance treatment with lamotrigine tablets is to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy. The target dose of lamotrigine tablets is 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day Accordingly, doses above 200 mg/day are not recommended. Treatment with lamotrigine tablets is introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. For patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2-week period in equal weekly increments (see Table 6). For patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin that induce lamotrigine glucuronidation, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated. [see ]. Clinical Studies (14.2)
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see , ]. Drug Interactions (7)Clinical Pharmacology (12.3)
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see ]. Boxed Warning
Table 5. Escalation Regimen for Lamotrigine Tablets for Patients With Bipolar Disordera Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see , ]. Drug Interactions (7)Clinical Pharmacology (12.3)
b These drugs induce lamotrigine glucuronidation and increase clearance [see , ]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see , ]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see ]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. Drug Interactions (7)Clinical Pharmacology (12.3)Drug Interactions (7)Clinical Pharmacology (12.3)Dosage and Administration (2.1)
For Patients TAKING
Valproate a
For Patients NOT TAKING
Carbamazepine, Phenytoin, Phenobarbital,
Primidone b, or Valproate a
For Patients TAKING
Carbamazepine, Phenytoin,
Phenobarbital, or Primidone b and NOT TAKING
Valproate a
Weeks 1 and 2
25 mg every day
other
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
Table 6. Dosage Adjustments to Lamotrigine Tablets for Patients With Bipolar Disorder Following Discontinuation of Psychotropic Medications
Discontinuation of Psychotropic Drugs
(excluding Carbamazepine, Phenytoin,
Phenobarbital, Primidone b, or
Valproate a)
After Discontinuation of
Valproate a
After Discontinuation of
Carbamazepine, Phenytoin,
Phenobarbital, or Primidone b
Current dose of lamotrigine tablets
(mg/day)
100
Current dose of lamotrigine tablets
(mg/day)
400
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see , ]. Drug Interactions (7)Clinical Pharmacology (12.3)
b These drugs induce lamotrigine glucuronidation and increase clearance [see , ]. Other drugs which have similar effects include estrogen-containing oral contraceptives [see , ]. Dosing recommendations for oral contraceptives can be found in General Dosing Considerations [see ]. Patients on rifampin, or other drugs that induce lamotrigine glucuronidation and increase clearance, should follow the same dosing titration/maintenance regimen as that used with anticonvulsants that have this effect. Drug Interactions (7)Clinical Pharmacology (12.3)Drug Interactions (7)Clinical Pharmacology (12.3)Dosage and Administration (2.1)
Week 1
Maintain current dose of lamotrigine tablets
150
400
Week 2
Maintain current dose of lamotrigine tablets
200
300
Week 3 onward
Maintain current dose of lamotrigine tablets
200
200
The benefit of continuing treatment in patients who had been stabilized in an 8- to 16-week open-label phase with lamotrigine tablets was established in two randomized, placebo-controlled clinical maintenance trials However, the optimal duration of treatment with lamotrigine tablets has not been established. Thus, patients should be periodically reassessed to determine the need for maintenance treatment. [see ]. Clinical Studies (14.2)
-
American Health Packaging
![Lamotrigine Tablet [American Health Packaging]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Ge Healthcare Inc.
![Lamotrigine Tablet [American Health Packaging] Lamotrigine Tablet [American Health Packaging]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
The volume and concentration of OMNIPAQUE 300 to be administered will depend on the degree and extent of contrast required in the area(s) under examination and on the equipment and technique employed.
OMNIPAQUE 300 at a concentration of 300 mgI/mL is recommended for the examination of the lumbar, thoracic, and cervical regions in adults by lumbar or direct cervical injection and is slightly hypertonic to CSF.
A total dose of 3060 mg iodine or a concentration of 300 mgI/mL should not be exceeded in adults in a single myelographic examination. This is based on clinical trial evaluation to date. As in all diagnostic procedures, the minimum volume and dose to produce adequate visualization should be used. Most procedures do not require either maximum dose or concentration.
Anesthesia is not necessary. Premedication sedatives or tranquilizers are usually not needed (see PRECAUTIONS). Patients should be well hydrated prior to and following contrast administration.
Seizure-prone patients should be maintained on anticonvulsant medication.
Many radiopaque contrast agents are incompatible in vitro with some antihistamines and many other drugs; therefore, concurrent drugs should not be physically admixed with contrast agents.
Rate of InjectionTo avoid excessive mixing with CSF and consequent dilution of contrast, injection should be made slowly over 1 to 2 minutes.
Depending on the estimated volume of contrast medium which may be required for the procedure a small amount of CSF may be removed to minimize distention of the subarachnoid spaces.
The lumbar or cervical puncture needle may be removed immediately following injection since it is not necessary to remove OMNIPAQUE after injection into the subarachnoid space.
AdultsThe usual recommended total doses for use in lumbar, thoracic, cervical, and total columnar myelography in adults are 1.2 gI to 3.0 gI as follows:
Procedure Formulations Concentration
(mgI/mL) Volume
(mL) Dose
(gI) Thoracic Myelography (via lumbar injection) OMNIPAQUE 300 300 6-10 1.8-3.0 Cervical Myelography (via lumbar injection) OMNIPAQUE 300 300 6-10 1.8-3.0 Cervical Myelography (via C1-2 injection OMNIPAQUE 300 300 4-10 1.2-3.0 Total Columnar Myelography (via lumbar injection OMNIPAQUE 300 300 6-10 1.8-3.0Refer to DIRECTIONS FOR PROPER USE OF OMNIPAQUE PHARMACY BULK PACKAGE section for instructions.
Parenteral products should be inspected visually for particulate matter or discoloration prior to administration. If particulate matter or discoloration is present, do not use.
Repeat ProceduresIf in the clinical judgment of the physician sequential or repeat examinations are required, a suitable interval of time between administrations should be observed to allow for normal clearance of the drug from the body. An interval of at least 48 hours should be allowed before repeat examination; however, whenever possible, 5 to 7 days is recommended.
As with all radiopaque contrast agents, the lowest dose of OMNIPAQUE necessary to obtain adequate visualization should be used. A lower dose may reduce the possibility of an adverse reaction. Most procedures do not require use of either the maximum volume or the highest concentration of OMNIPAQUE. The combination of volume and concentration of OMNIPAQUE to be used should be carefully individualized accounting for factors such as age, body weight, size of the vessel and the rate of blood flow within the vessel. Other factors such as anticipated pathology, degree and extent of opacification required, structure(s) or area to be examined, disease processes affecting the patient, and equipment and technique to be employed should be considered.
Sterile technique must be used in all vascular injections involving contrast media.
Refer to DIRECTIONS FOR PROPER USE OF OMNIPAQUE PHARMACY BULK PACKAGE section for instructions.
If nondisposable equipment is used, scrupulous care should be taken to prevent residual contamination with traces of cleansing agents.
It may be desirable that solutions of radiopaque diagnostic agents be used at body temperature when injected.
Parenteral products should be inspected visually for particulate matter and discoloration prior to administration whenever solution and container permit. Solutions of OMNIPAQUE should be used only if clear and within the normal colorless to pale yellow range. If particulate matter or discoloration is present, do not use.
Dosage and AdministrationThe individual dose or volume is determined by the size of the structure to be visualized, the anticipated degree of hemodilution, and valvular competence. Weight is a minor consideration in adults, but must be considered in infants and young children. The volume of each individual injection is a more important consideration than the total dosage used. When large individual volumes are administered, as in ventriculography and aortography, it has been suggested that several minutes be permitted to elapse between each injection to allow for subsidence of possible hemodynamic disturbances.
The recommended single injection volume of OMNIPAQUE 350 for angiocardiographic procedures in adults and the recommended single injection volumes of OMNIPAQUE 350 and OMNIPAQUE 300 for angiographic procedures in children are as follows:
Ventriculography AdultsThe usual adult volume for a single injection is 40 mL with a range of 30 mL to 60 mL. This may be repeated as necessary. When combined with selective coronary arteriography, the total administered volume should not exceed 250 mL (87.5 gI).
PediatricsThe usual single injection dose of OMNIPAQUE 350 is 1.25 mL/kg of body weight with a range of 1.0 mL/kg to 1.5 mL/kg. For OMNIPAQUE 300 the usual single injection dose is 1.75 mL/kg with a range of 1.5 mL/kg to 2.0 mL/kg. When multiple injections are given, the total administered dose should not exceed 5 mL/kg up to a total volume of 250 mL of OMNIPAQUE 350 or up to a total volume of 291 mL of OMNIPAQUE 300.
Selective Coronary ArteriographyThe usual adult volume for right or left coronary arteriography is 5 mL (range 3 mL to 14 mL) per injection.
Aortic Root and Arch Study When Used AloneThe usual adult single injection volume is 50 mL, with a range of 20 mL to 75 mL.
Pulmonary Angiography PediatricsThe usual single injection dose is 1.0 mL/kg of OMNIPAQUE 350.
Combined Angiocardiographic Procedures Multiple Procedures AdultsThe visualization of multiple vascular systems and target organs is possible during a single radiographic examination of the patient.
Large doses of OMNIPAQUE 350 were well tolerated in angiographic procedures requiring multiple injections.
The maximum total volume for multiple procedures should not exceed 250 mL of 350 mgI/mL (87.5 gI).
PediatricsVisualization of multiple vascular systems and target organs is possible during a single radiographic examination of the patient.
The maximum total dose for multiple injection procedures should not exceed 5.0 mL/kg up to a total volume of 250 mL of OMNIPAQUE 350 or 6.0 mL/kg up to a total volume of 291 mL of OMNIPAQUE 300.
Dosage and Administration AdultsThe usual adult volume as a single injection is 50 mL to 80 mL for the aorta, 30 mL to 60 mL for major branches including celiac and mesenteric arteries, and 5 mL to 15 mL for renal arteries. Repeated injections may be performed if indicated, but the total volume should not exceed 291 mL of OMNIPAQUE 300 or 250 mL of OMNIPAQUE 350 (87.5 gI).
PediatricsThe usual single injection dose is 1.0 mL/kg of OMNIPAQUE 350 and should not exceed 5.0 mL/kg up to a total volume of 250 mL of OMNIPAQUE 350.
Dosage and AdministrationOMNIPAQUE 300 is recommended for cerebral arteriography at the following volumes: common carotid artery (6 mL to 12 mL), internal carotid artery (8 mL to 10 mL), external carotid artery (6 mL to 9 mL), and vertebral artery (6 mL to 10 mL).
Dosage and AdministrationThe concentration and volume required will depend on the equipment and imaging technique used.
Dosage and AdministrationThe usual injection volume of OMNIPAQUE 350 for the intravenous digital technique is 30 mL to 50 mL of a 350 mgI/mL solution. This is administered as a bolus at 7.5 to 30 mL/second using a pressure injector. The volume and rate of injection will depend primarily on the type of equipment and technique used.
Frequently three or more injections may be required, up to a total volume not to exceed 250 mL (87.5 gI).
Dosage and AdministrationThe volume required will depend on the size, flow rate, and disease state of the injected vessel and on the size and condition of the patient, as well as the imaging technique used.
The dosage recommended for use in peripheral angiography is as follows:
Aortofemoral runoffs: 20 mL to 70 mL of OMNIPAQUE 350 (350 mgI/mL)
30 mL to 90 mL of OMNIPAQUE 300 (300 mgI/mL) Selective arteriograms: (femoral/iliac) 10 mL to 30 mL of OMNIPAQUE 350 (350 mgI/mL)
10 mL to 60 mL of OMNIPAQUE 300 (300 mgI/mL) Venography (per leg): 40 mL to 100 mL of OMNIPAQUE 300 (300 mgI/mL) Dosage and Administration AdultsOMNIPAQUE 300 and OMNIPAQUE 350 at dosages from 200 mgI/kg body weight to 350 mgI/kg body weight have produced diagnostic opacification of the excretory system in patients with normal renal function.
See SECTION II, DOSAGE AND ADMINISTRATION—General.
Dosage and Administration AdultsThe recommended dosage of undiluted OMNIPAQUE 350 at a concentration of 350 mgI/mL for oral pass-thru examination of the gastrointestinal tract in adults is 50 mL to 100 mL depending on the nature of the examination and the size of the patient.
The recommended oral dosage of OMNIPAQUE diluted to concentrations of 6 mgI/mL to 9 mgI/mL for contrast enhanced computed tomography of the abdomen in adults is 500 mL to 1000 mL. Smaller administered volumes are needed as the concentration of the final solution is increased (see Table below). In conjunction with dilute oral administration, the recommended dosage of OMNIPAQUE 300 administered intravenously is 100 mL to 150 mL. The oral dose is administered about 20 to 40 minutes prior to the intravenous dose and image acquisition.
ChildrenThe dosage of undiluted OMNIPAQUE 300 at a concentration of 300 mgI/mL, is dependent on the nature of the examination and the size of the patient. Based on clinical experience, it is recommended that OMNIPAQUE 180 (available in single use vials), be used in children less than 3 months of age. OMNIPAQUE 300 may be used in children 3 months of age and older. The following dosage guidelines are recommended:
Age Volume of OMNIPAQUE Less than 3 months 5 — 30 mL Three months to 3 years Up to 60 mL Four years to 10 years Up to 80 mL Greater than 10 years Up to 100 mLWhen given rectally, larger volumes may be used.
The recommended oral dosage of OMNIPAQUE diluted to concentrations of 9 mgI/mL to 21 mgI/mL for contrast enhanced computed tomography of the abdomen in children is 180 mL to 750 mL. Smaller administered volumes are needed as the concentration of the final solution is increased (see Table below). The total oral dose in grams of iodine should generally not exceed 5 gI for children under 3 years of age and 10 gI for children from 3 to 18 years of age. The oral dosage may be given all at once or over a period of 30 to 45 minutes if there is difficulty in consuming the required volume.
In conjunction with dilute oral administration the recommended dosage of OMNIPAQUE 300 is 2.0 mL/kg when administered intravenously with a range of 1.0 mL/kg to 2.0 mL/kg. Dosage for infants and children should be administered in proportion to age and body weight. The total intravenously administered dose should not exceed 3 mL/kg. The oral dose is administered about 30 to 60 minutes prior to the intravenous dose and image acquisition.
OMNIPAQUE may be diluted with water or beverage as follows:
To Achieve Add To One Liter of Contrast Medium at A Final Concentration
(mgI/mL) of Stock Concentration of OMNIPAQUE
(mgI/mL) Volume
(mL) Water, Carbonated Beverage, Milk, or Juice
(mL) 6 300 20 980 350 17 983 9 300 30 970 350 26 974 12 300 40 960 350 35 965 15 300 50 950 350 43 957 18 300 60 940 350 52 948 21 300 70 930 350 60 940Dilutions of OMNIPAQUE should be prepared just prior to use and any unused portion discarded after the procedure.
Dosage and AdministrationOMNIPAQUE may be diluted, utilizing aseptic technique, with Sterile Water for Injection to a concentration of 50 mgI/mL to 100 mgI/mL for voiding cystourethrography. The concentration may vary depending upon the patient's size and age and also with the technique and equipment used. Sufficient volume of contrast medium should be administered to adequately fill the bladder. The usual volume ranges from 50 mL to 300 mL of OMNIPAQUE at a concentration of 100 mgI/mL and 50 mL to 600 mL of OMNIPAQUE at a concentration of 50 mgI/mL.
OMNIPAQUE may be diluted with Sterile Water for Injection as indicated in the table below:
To Achieve Add To A Final Concentration Each 100 mL of OMNIPAQUE Sterile Water for Injection, USP (mL) (mgI/mL) OMNIPAQUE 300 OMNIPAQUE 350 100 200 250 90 233 289 80 275 338 70 330 400 60 400 483 50 500 600Dilutions of OMNIPAQUE should be prepared just prior to use and any unused portion discarded after the procedure.
Dosage and AdministrationArthrography is usually performed under local anesthesia. The amount of OMNIPAQUE injected is dependent on the size of the joint to be examined and the technique employed. Lower volumes of contrast medium are usually injected for knee and shoulder arthrography when double-contrast examinations using 15 mL to 100 mL of air are performed.
The following concentrations and volumes are recommended for normal adult knee, shoulder, and temporomandibular joints but should serve as guidelines since joints may require more or less contrast medium for optimal visualization.
KNEE Lower volumes recommended for double-contrast examinations; higher volumes recommended for single-contrast examinations. OMNIPAQUE 300 5 mL to 15 mL OMNIPAQUE 350 5 mL to 10 mL SHOULDER OMNIPAQUE 300 10 mL TEMPOROMANDIBULAR OMNIPAQUE 300 0.5 mL to 1.0 mLPassive or active manipulation is used to disperse the medium throughout the joint space.
Dosage and AdministrationThe recommended dosage of OMNIPAQUE 300 is 15 mL to 20 mL but will vary depending on individual anatomy and/or disease state.
-
Northstar Rxllc
![Lamotrigine Tablet [Northstar Rxllc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Northstar Rxllc
![Lamotrigine Tablet [Northstar Rxllc] Lamotrigine Tablet [Northstar Rxllc]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
2.1. General Dosing ConsiderationsRash
There are suggestions, yet to be proven, that the risk of severe, potentially life-threatening rash may be increased by (1) coadministration of lamotrigine tablets with valproate, (2) exceeding the recommended initial dose of lamotrigine tablets, or (3) exceeding the recommended dose escalation for lamotrigine tablets. However, cases have occurred in the absence of these factors [see Boxed Warning]. Therefore, it is important that the dosing recommendations be followed closely.The risk of nonserious rash may be increased when the recommended initial dose and/or the rate of dose escalation for lamotrigine tablets are exceeded and in patients with a history of allergy or rash to other AEDs.
It is recommended that lamotrigine tablets not be restarted in patients who discontinued due to rash associated with prior treatment with lamotrigine, unless the potential benefits clearly outweigh the risks. If the decision is made to restart a patient who has discontinued lamotrigine, the need to restart with the initial dosing recommendations should be assessed. The greater the interval of time since the previous dose, the greater consideration should be given to restarting with the initial dosing recommendations. If a patient has discontinued lamotrigine for a period of more than 5 half-lives, it is recommended that initial dosing recommendations and guidelines be followed. The half-life of lamotrigine is affected by other concomitant medications [see Clinical Pharmacology (12.3)].
Lamotrigine Tablets Added to Drugs Known to Induce or Inhibit Glucuronidation
Because lamotrigine is metabolized predominantly by glucuronic acid conjugation, drugs that are known to induce or inhibit glucuronidation may affect the apparent clearance of lamotrigine. Drugs that induce glucuronidation include carbamazepine, phenytoin, phenobarbital, primidone, rifampin, estrogen-containing oral contraceptives, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Valproate inhibits glucuronidation. For dosing considerations for lamotrigine tablets in patients on estrogen-containing contraceptives and atazanavir/ritonavir, see below and Table 13. For dosing considerations for lamotrigine tablets in patients on other drugs known to induce or inhibit glucuronidation, see Tables 1, 2, 5 to 6, and 13.Target Plasma Levels for Patients with Epilepsy or Bipolar Disorder
A therapeutic plasma concentration range has not been established for lamotrigine. Dosing of lamotrigine tablets should be based on therapeutic response [see Clinical Pharmacology (12.3)].Women Taking Estrogen-Containing Oral Contraceptives
Starting Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives: Although estrogen-containing oral contraceptives have been shown to increase the clearance of lamotrigine [see Clinical Pharmacology (12.3)], no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of estrogen-containing oral contraceptives. Therefore, dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on the concomitant AED or other concomitant medications (see Table 1, 5 and 7). See below for adjustments to maintenance doses of lamotrigine tablets in women taking estrogen-containing oral contraceptives.Adjustments to the Maintenance Dose of Lamotrigine Tablets in Women Taking Estrogen-Containing Oral Contraceptives
1) Taking Estrogen-Containing Oral Contraceptives:In women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be increased by as much as 2-fold over the recommended target maintenance dose to maintain a consistent lamotrigine plasma level
2) Starting Estrogen-Containing Oral Contraceptives:In women taking a stable dose of lamotrigine tablets and not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose will in most cases need to be increased by as much as 2-fold to maintain a consistent lamotrigine plasma level. The dose increases should begin at the same time that the oral contraceptive is introduced and continue, based on clinical response, no more rapidly than 50 to 100 mg/day every week. Dose increases should not exceed the recommended rate (see Tables 1 and 5) unless lamotrigine plasma levels or clinical response support larger increases. Gradual transient increases in lamotrigine plasma levels may occur during the week of inactive hormonal preparation (pill-free week), and these increases will be greater if dose increases are made in the days before or during the week of inactive hormonal preparation. Increased lamotrigine plasma levels could result in additional adverse reactions, such as dizziness, ataxia, and diplopia. If adverse reactions attributable to lamotrigine tablets consistently occur during the pill-free week, dose adjustments to the overall maintenance dose may be necessary. Dose adjustments limited to the pill-free week are not recommended. For women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine should be necessary.
3) Stopping Estrogen-Containing Oral Contraceptives:In women not taking carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], the maintenance dose of lamotrigine tablets will in most cases need to be decreased by as much as 50%, in order to maintain a consistent lamotrigine plasma level. The decrease in dose of lamotrigine tablets should not exceed 25% of the total daily dose per week over a 2-week period, unless clinical response or lamotrigine plasma levels indicate otherwise [see Clinical Pharmacology (12.3)]. In women taking lamotrigine tablets in addition to carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation [see Drug Interactions (7), Clinical Pharmacology (12.3)], no adjustment to the dose of lamotrigine tablets should be necessary.
Women and Other Hormonal Contraceptive Preparations or Hormone Replacement Therapy
The effect of other hormonal contraceptive preparations or hormone replacement therapy on the pharmacokinetics of lamotrigine has not been systematically evaluated. It has been reported that ethinylestradiol, not progestogens, increased the clearance of lamotrigine up to 2-fold, and the progestin-only pills had no effect on lamotrigine plasma levels. Therefore, adjustments to the dosage of lamotrigine tablets in the presence of progestogens alone will likely not be needed.Patients Taking Atazanavir/Ritonavir
While atazanavir/ritonavir does reduce the lamotrigine plasma concentration, no adjustments to the recommended dose-escalation guidelines for lamotrigine tablets should be necessary solely based on the use of atazanavir/ritonavir. Dose escalation should follow the recommended guidelines for initiating adjunctive therapy with lamotrigine tablets based on concomitant AED or other concomitant medications (see Tables 1, 2, and 5). In patients already taking maintenance doses of lamotrigine tablets and not taking glucuronidation inducers, the dose of lamotrigine tablets may need to be increased if atazanavir/ritonavir is added, or decreased if atazanavir/ritonavir is discontinued [see Clinical Pharmacology (12.3)].Patients with Hepatic Impairment
Experience in patients with hepatic impairment is limited. Based on a clinical pharmacology study in 24 subjects with mild, moderate, and severe liver impairment [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)],the following general recommendations can be made. No dosage adjustment is needed in patients with mild liver impairment. Initial, escalation, and maintenance doses should generally be reduced by approximately 25% in patients with moderate and severe liver impairment without ascites and 50% in patients with severe liver impairment with ascites. Escalation and maintenance doses may be adjusted according to clinical response.
Patients with Renal Impairment
Initial doses of lamotrigine tablets should be based on patients’ concomitant medications (see Tables 1 to 3, and 5); reduced maintenance doses may be effective for patients with significant renal impairment [see Use in Specific Populations (8.7), Clinical Pharmacology (12.3)]. Few patients with severe renal impairment have been evaluated during chronic treatment with lamotrigine tablets. Because there is inadequate experience in this population, lamotrigine tablets should be used with caution in these patients.Discontinuation Strategy
Epilepsy: For patients receiving lamotrigine tablets in combination with other AEDs, a re-evaluation of all AEDs in the regimen should be considered if a change in seizure control or an appearance or worsening of adverse reactions is observed.If a decision is made to discontinue therapy with lamotrigine tablets, a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) is recommended unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.8)].
Discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproate should shorten the half-life of lamotrigine.
Bipolar Disorder: In the controlled clinical trials, there was no increase in the incidence, type, or severity of adverse reactions following abrupt termination of lamotrigine tablets. In the clinical development program in adults with bipolar disorder, 2 patients experienced seizures shortly after abrupt withdrawal of lamotrigine tablets. Discontinuation of lamotrigine tablets should involve a step-wise reduction of dose over at least 2 weeks (approximately 50% per week) unless safety concerns require a more rapid withdrawal [see Warnings and Precautions (5.8)].
2.2. Epilepsy - Adjunctive TherapyThis section provides specific dosing recommendations for patients older than 12 years and patients aged 2 to 12 years. Within each of these age-groups, specific dosing recommendations are provided depending upon concomitant AEDs or other concomitant medications (see Table 1 for patients older than 12 years and Table 2 for patients aged 2 to 12 years). A weight-based dosing guide for patients aged 2 to 12 years on concomitant valproate is provided in Table 3.
Patients Older than 12 Years
Recommended dosing guidelines are summarized in Table 1.Table 1
Escalation Regimen for Lamotrigine Tablets in Patients Older than 12 Years with Epilepsy
In Patients TAKING Valproatea
In Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidoneb, or Valproatea
In Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneband NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg every day
50 mg/day
Weeks 3 and 4
25 mg every day
50 mg/day
100 mg/day
(in 2 divided doses)
Week 5 onwards to maintenance
Increase by 25 to 50 mg/day every 1 to 2 weeks
Increase by 50 mg/day every 1 to 2 weeks
Increase by 100 mg/day every 1 to 2 weeks.
Usual Maintenance Dose
100 to 200 mg/day with valproate alone
100 to 400 mg/day
with valproate and other drugs that induce glucuronidation
( in 1 or 2 divided doses)
225 to 375 mg/day
(in 2 divided doses)
300 to 500 mg/day
(in 2 divided doses)
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)].
Patients Aged 2 to 12 Years
Recommended dosing guidelines are summarized in Table 2.Lower starting doses and slower dose escalations than those used in clinical trials are recommended because of the suggestion that the risk of rash may be decreased by lower starting doses and slower dose escalations. Therefore, maintenance doses will take longer to reach in clinical practice than in clinical trials. It may take several weeks to months to achieve an individualized maintenance dose. Maintenance doses in patients weighing less than 30 kg, regardless of age or concomitant AED, may need to be increased as much as 50%, based on clinical response.
Table 2
Escalation Regimen for Lamotrigine Tablets in Patients Aged 2 to 12 Years with Epilepsy
In Patients TAKING Valproatea
In Patients
NOT TAKING Carbamazepine,
Phenytoin,
Phenobarbital,
Primidoneb, or Valproatea
For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneband NOT TAKING Valproatea
Weeks 1 and 2
0.15 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide).
0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet.
0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet.
Weeks 3 and 4
0.3 mg/kg/day
in 1 or 2 divided doses, rounded down to the nearest whole tablet (see Table 3 for weight-based dosing guide).
0.6 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet.
1.2 mg/kg/day
in 2 divided doses, rounded down to the nearest whole tablet.
Week 5 onwards to maintenance
The dose should be increased every 1 to 2 weeks as follows: calculate 0.3 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose.
The dose should be increased every 1 to 2 weeks as follows: calculate 0.6 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
The dose should be increased every 1 to 2 weeks as follows: calculate 1.2 mg/kg/day, round this amount down to the nearest whole tablet, and add this amount to the previously administered daily dose
Usual maintenance dose
1 to 5 mg/kg/day(maximum 200 mg/day in 1 or 2 divided doses).
1 to 3 mg/kg/day with valproate alone
4.5 to 7.5 mg/kg/day
(maximum 300 mg/day in 2 divided doses)
5 to 15 mg/kg/day(maximum 400 mg/day in 2 divided doses)
Maintenance dose in patients less than 30 kg
May need to be increased by as much as 50%, based on clinical response
May need to be increased by as much as 50%, based on clinical response
May need to be increased by as much as 50%, based on clinical response
Note: Only whole tablets should be used for dosing
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].b Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)].
Table 3
The Initial Weight-Based Dosing Guide for Patients Aged 2 to 12 Years Taking Valproate (Weeks 1 to 4) with Epilepsy
If the patient’s weight is
Give this daily dose, using the most appropriate combination of lamotrigine tablets 2- and 5-mg tablets
Greater than
And less than
Weeks 1 and 2
Weeks 3 and 4
6.7 kg
14 kg
2 mg every other day
2 mg every day
14.1 kg
27 kg
2 mg every day
4 mg every day
27.1 kg
34 kg
4 mg every day
8 mg every day
34.1 kg
40 kg
5 mg every day
10 mg every day
Usual Adjunctive Maintenance Dose for Epilepsy
2.3. Epilepsy - Conversion from Adjunctive Therapy to Monotherapy
The usual maintenance doses identified in Tables 1 and 2 are derived from dosing regimens employed in the placebo-controlled adjunctive trials in which the efficacy of lamotrigine tablets were established. In patients receiving multidrug regimens employing carbamazepine, phenytoin, phenobarbital, or primidone without valproate , maintenance doses of adjunctive lamotrigine tablets as high as 700 mg/day have been used. In patients receiving valproate alone , maintenance doses of adjunctive lamotrigine tablets as high as 200 mg/day have been used. The advantage of using doses above those recommended in Tables 1 to 4 has not been established in controlled trials.The goal of the transition regimen is to attempt to maintain seizure control while mitigating the risk of serious rash associated with the rapid titration of lamotrigine tablets.
The recommended maintenance dose of lamotrigine tablets as monotherapy is 500 mg/day given in 2 divided doses.
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations for lamotrigine tablets should not be exceeded [see Boxed Warning].
Conversion from Adjunctive Therapy with Carbamazepine, Phenytoin, Phenobarbital, or Primidone to Monotherapy with Lamotrigine Tablets
After achieving a dose of 500 mg/day of lamotrigine tablets using the guidelines in Table 1, the concomitant enzyme-inducing AED should be withdrawn by 20% decrements each week over a 4-week period. The regimen for the withdrawal of the concomitant AED is based on experience gained in the controlled monotherapy clinical trial.
Conversion from Adjunctive Therapy with Valproate to Monotherapy with Lamotrigine Tablets
The conversion regimen involves the 4 steps outlined in Table 4.
Table 4Conversion from Adjunctive Therapy with Valproate to Monotherapy with Lamotrigine Tablets in Patients Aged 16 Years and Older with Epilepsy
Lamotrigine Tablets
Valproate
Step 1
Achieve a dose of 200 mg/day according to guidelines in Table 1
Maintain established stable dose.
Step 2
Maintain at 200 mg/day.
Decrease dose by decrements no greater than 500 mg/day/ week to 500 mg/day and then maintain for 1 week.
Step 3
Increase to 300 mg/day and maintain for 1 week.
Simultaneously decrease to 250 mg/day and maintain for 1 week.
Step 4
Increase by 100 mg/day every week to achieve maintenance dose of 500 mg/day.
Discontinue.
Conversion from Adjunctive Therapy with Antiepileptic Drugs other than Carbamazepine, Phenytoin, Phenobarbital, Primidone, or Valproate to Monotherapy with Lamotrigine Tablets
2.4. Bipolar Disorder
No specific dosing guidelines can be provided for conversion to monotherapy with lamotrigine tablets with AEDs other than carbamazepine, phenytoin, phenobarbital, primidone, or valproate.The goal of maintenance treatment with lamotrigine tablets are to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes) in patients treated for acute mood episodes with standard therapy therapy [see Indications and Usage (1)].
Patients taking lamotrigine tablets for more than 16 weeks should be periodically reassessed to determine the need for maintenance treatment.
Adults
The target dose of lamotrigine tablets are 200 mg/day (100 mg/day in patients taking valproate, which decreases the apparent clearance of lamotrigine, and 400 mg/day in patients not taking valproate and taking either carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir that increase the apparent clearance of lamotrigine). In the clinical trials, doses up to 400 mg/day as monotherapy were evaluated; however, no additional benefit was seen at 400 mg/day compared with 200 mg/day [see Clinical Studies (14.2)]. Accordingly, doses above 200 mg/day are not recommended.
Treatment with lamotrigine tablets are introduced, based on concurrent medications, according to the regimen outlined in Table 5. If other psychotropic medications are withdrawn following stabilization, the dose of lamotrigine tablets should be adjusted. In patients discontinuing valproate, the dose of lamotrigine tablets should be doubled over a 2-week period in equal weekly increments (see Table 6). In patients discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs such as rifampin and the protease inhibitors lopinavir/ritonavir that induce lamotrigine glucuronidation, the dose of lamotrigine tablets should remain constant for the first week and then should be decreased by half over a 2-week period in equal weekly decrements (see Table 6). The dose of lamotrigine tablets may then be further adjusted to the target dose (200 mg) as clinically indicated.
If other drugs are subsequently introduced, the dose of lamotrigine tablets may need to be adjusted. In particular, the introduction of valproate requires reduction in the dose of lamotrigine tablets [see Drug Interactions (7), Clinical Pharmacology (12.3)].
To avoid an increased risk of rash, the recommended initial dose and subsequent dose escalations of lamotrigine tablets should not be exceeded [see Boxed Warning].
Table 5
Escalation Regimen for Lamotrigine Tablets in Adults with Bipolar Disorder
In Patients TAKING Valproatea
In Patients NOT TAKING Carbamazepine, Phenytoin, Phenobarbital, Primidoneb, or Valproatea
For Patients TAKING Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb and NOT TAKING Valproatea
Weeks 1 and 2
25 mg every other day
25 mg daily
50 mg daily
Weeks 3 and 4
25 mg daily
50 mg daily
100 mg daily, in divided doses
Week 5
50 mg daily
100 mg daily
200 mg daily, in divided doses
Week 6
100 mg daily
200 mg daily
300 mg daily, in divided doses
Week 7
100 mg daily
200 mg daily
up to 400 mg daily, in divided doses
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology(12.3)].
Table 6Dosage Adjustments to Lamotrigine Tablets in Adults with Bipolar Disorder Following
Discontinuation of Psychotropic Medications
Discontinuation of Psychotropic Drugs (excluding Carbamazepine, Phenytoin, Phenobarbital Primidoneb)
After Discontinuation of Valproatea
After Discontinuation of Carbamazepine, Phenytoin, Phenobarbital, or Primidoneb
Current Dose of Lamotrigine Tablets (mg/day) 100
Current Dose of Lamotrigine Tablets (mg/day) 400
Week 1
Maintain current dose of Lamotrigine Tablets
150
400
Week 2
Maintain current dose of Lamotrigine Tablets
200
300
Week 3 onward
Maintain current dose of Lamotrigine Tablets
200
200
a Valproate has been shown to inhibit glucuronidation and decrease the apparent clearance of lamotrigine [see Drug Interactions (7), Clinical Pharmacology (12.3)].
b Drugs that induce lamotrigine glucuronidation and increase clearance, other than the specified antiepileptic drugs, include estrogen-containing oral contraceptives, rifampin, and the protease inhibitors lopinavir/ritonavir and atazanavir/ritonavir. Dosing recommendations for oral contraceptives and the protease inhibitor atazanavir/ritonavir can be found in General Dosing Considerations [see Dosage and Administration (2.1)]. Patients on rifampin and the protease inhibitor lopinavir/ritonavir should follow the same dosing titration/maintenance regimen used with antiepileptic drugs that induce glucuronidation and increase clearance [see Dosage and Administration (2.1), Drug Interactions (7), and Clinical Pharmacology (12.3)].
-
Cardinal Health
![Lamotrigine Tablet [Cardinal Health]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Lamotrigine | Teva Pharmaceuticals Usa Inc
![Lamotrigine Tablet [Cardinal Health] Lamotrigine Tablet [Cardinal Health]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
HypertensionThe recommended initial dosage of trandolapril tablets for patients not receiving a diuretic is 1 mg once daily in non-black patients and 2 mg in black patients. Dosage should be adjusted according to the blood pressure response. Generally, dosage adjustments should be made at intervals of at least 1 week. Most patients have required dosages of 2 to 4 mg once daily. There is little clinical experience with doses above 8 mg.
Patients inadequately treated with once-daily dosing at 4 mg may be treated with twice-daily dosing. If blood pressure is not adequately controlled with trandolapril tablets monotherapy, a diuretic may be added.
In patients who are currently being treated with a diuretic, symptomatic hypotension occasionally can occur following the initial dose of trandolapril tablets. To reduce the likelihood of hypotension, the diuretic should, if possible, be discontinued two to three days prior to beginning therapy with trandolapril tablets. (See WARNINGS.) Then, if blood pressure is not controlled with trandolapril tablets alone, diuretic therapy should be resumed. If the diuretic cannot be discontinued, an initial dose of 0.5 mg trandolapril tablets should be used with careful medical supervision for several hours until blood pressure has stabilized. The dosage should subsequently be titrated (as described above) to the optimal response. (See WARNINGS and PRECAUTIONS, Drug Interactions.)
Concomitant administration of trandolapril tablets with potassium supplements, potassium salt substitutes, or potassium sparing diuretics can lead to increases of serum potassium. (See PRECAUTIONS.)
Heart Failure Post Myocardial Infarction or Left-Ventricular Dysfunction Post Myocardial InfarctionThe recommended starting dose is 1 mg, once daily. Following the initial dose, all patients should be titrated (as tolerated) toward a target dose of 4 mg, once daily. If a 4 mg dose is not tolerated, patients can continue therapy with the greatest tolerated dose.
Dosage Adjustment in Renal Impairment or Hepatic CirrhosisFor patients with a creatinine clearance < 30 mL/min. or with hepatic cirrhosis, the recommended starting dose, based on clinical and pharmacokinetic data, is 0.5 mg daily. Patients should subsequently have their dosage titrated (as described above) to the optimal response.
Login To Your Free Account

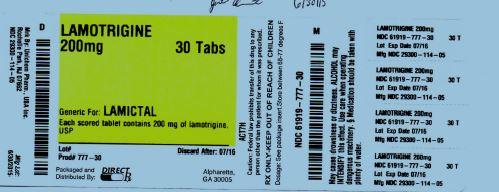

![Lamotrigine (Lamotrigine) Tablet [Avpak]](http://www.recallguide.org/wp-content/themes/recallguide/assets/img/drug-image-placeholder.jpg)
![Lamotrigine Tablet [Proficient Rx Lp]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=b94ae2e4-e276-40c1-bc25-da980194fc99&name=lamotriginetablet-figure-04.jpg)
![Lamotrigine Tablet [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=2b670a0c-9d63-4da1-ad23-8a7ff9a49571&name=MM4.jpg)
![Lamotrigine Tablet, Orally Disintegrating [Global Pharmaceuticals, Division Of Impax Laboratories Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=380bddae-5b31-4965-96de-97711d859d11&name=lamotrigine-03.jpg)
![Lamotrigine Tablet [Direct Rx]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=b71ea970-4d53-44c2-aaed-19f2b5d22ce3&name=label1.jpg)
![Lamotrigine Tablet [State Of Florida Doh Central Pharmacy]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=d07bcc09-7679-4bc1-84be-83d86c26147f&name=Lamotigine25mg.jpg)
![Lamotrigine (Lamotrigine ) Tablet [State Of Florida Doh Central Pharmacy]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=3ace34cc-eac4-45a4-9c8e-b18e8157d98d&name=Lamotrigine25mg.jpg)
![Lamotrigine Tablet [State Of Florida Doh Central Pharmacy]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=2ea96dec-633c-4afb-9cd1-30861712be9f&name=Lamotrigine25mg.jpg)
![Lamotrigine Tablet Lamotrigine Kit [Sandoz Inc]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=19c64c47-0410-4c7d-bad8-dbcd8fb94d1a&name=b0406e06-b384-4f8a-9c2c-e8dba2389c42-02.jpg)
![Lamotrigine Tablet [Mckesson Packaging Services Business Unit Of Mckesson Corporation]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=d44bd66b-90e6-4447-803c-7c3bc02bf877&name=d44bd66b-90e6-4447-803c-7c3bc02bf877-02.jpg)
![Lamotrigine Tablet [Mckesson Packaging Services A Buisness Unit Of Mckesson Corporation]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=5fb7c70d-410f-46a6-9906-edd5106c34d0&name=5fb7c70d-410f-46a6-9906-edd5106c34d0-02.jpg)
![Lamotrigine Tablet [Stat Rx Usa Llc]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=11800356-759d-4a8d-8811-e7942a3db6f5&name=LAMOTRIGINE100mg_802.jpg)
![Lamotrigine (Lamotrigine ) Tablet [Pd-rx Pharmaceuticals, Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=f31e1854-6068-4e45-b1e5-6def862fc466&name=43063203.jpg)
![Lamotrigine (Lamotrigine ) Tablet [Pd-rx Pharmaceuticals, Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=e879e3e4-0cbc-4e69-9466-63d445d4f0cc&name=43063259.jpg)
![Lamotrigine (Lamotrigine ) Tablet [Pd-rx Pharmaceuticals, Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=c638ab70-05dd-4f8b-9a11-b33a75f8c504&name=43063238.jpg)
![Lamotrigine (Lamotrigine ) Tablet [Pd-rx Pharmaceuticals, Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=4f7c068e-f499-436b-a533-15e5bf6cfbd2&name=43063202.jpg)
![Lamotrigine Tablet [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=cf3d4110-3ae5-46fd-84f4-127fd2998dbb&name=MM2.jpg)
![Lamotrigine Tablet [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=c3bd674c-cf21-4957-bbaf-ddd4b0770ff4&name=MM2.jpg)
![Lamotrigine Tablet [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=502fac46-67a6-4c4d-a666-65305d50d7a1&name=MM2.jpg)
![Lamotrigine Tablet [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=23452a86-8ae2-4165-aca6-056b3d2c6462&name=MM2.jpg)
![Lamotrigine Tablet, Chewable [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=8e9e8cb6-d28a-475a-9584-a1dee4899c4f&name=MM2.jpg)
![Lamotrigine Tablet [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=e2d3f96d-7e36-4b80-8fa5-7a4e606148c3&name=MM2.jpg)
![Lamotrigine Tablet [West-ward Pharmaceutical Corp]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=71a48f30-97f8-44d9-aaff-71447c553688&name=lamotrigine-tablets-3.jpg)
![Lamotrigine Tablet [Hikma Pharmaceutical]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=0a268a3a-4179-4f87-8125-53172992b0a8&name=lamotrigine-tablets-3.jpg)
![Lamotrigine Tablet [Ncs Healthcare Of Ky, Inc Dba Vangard Labs]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=8e2fc056-755f-447a-98d6-351879729e13&name=lamotrigine-2.jpg)
![Lamotrigine Tablet [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=6056b480-a27f-403f-b92b-b0bc6e5e7b0e&name=MM2.jpg)
![Lamotrigine Tablet [Rebel Distributors Corp]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=7332e0ea-fbd0-43fb-8d1e-f7068504c61d&name=7332e0ea-fbd0-43fb-8d1e-f7068504c61d-06.jpg)
![Lamotrigine Tablet [Lake Erie Medical & Surgical Supply Dba Quality Care Products Llc]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=d8de0c54-16a3-4c06-b1e7-58f966093d2b&name=Lamotrigine100mgTaro.jpg)
![Lamotrigine Tablet, Chewable [Mylan Pharmaceuticals Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=9780fed5-d051-46c5-851b-9b8800eb43bf&name=ab4fe0f9-4d21-4a99-8136-133cf4ac66d7-02.jpg)
![Lamotrigine Tablet Lamotrigine Tablet, Chewable [Cadila Healthcare Limited]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=0f2f7421-56d4-45d0-9d2d-dc1edaede039&name=lamotriginetabmanu-figure-04.jpg)
![Lamotrigine Tablet [Unichem Pharmaceuticals (Usa), Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=4b72ea7a-a0b0-4980-84ad-84f64e2e6368&name=lamotriginetablet-figure-04.jpg)
![Lamotrigine Tablet [Cardinal Health]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=91198340-cf13-4c76-93fd-0c3ef7c300b3&name=361e8060-b977-4a40-a32b-7db04f256378-02.jpg)
![Lamotrigine Tablet [Unit Dose Services]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=aea4c8d6-12c7-4729-a199-94e378d42303&name=rspl50436-3995.jpg)
![Lamotrigine Tablet, Chewable [Dr. Reddy’s Laboratories Limited]](http://recallguide.cwdevelopsp.com/wp-content/themes/recallguide/assets/img/drug-image-placeholder.jpg)
![Lamotrigine Tablet [Bryant Ranch Prepack]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=2bff8e82-83e6-0430-abde-0a27ad460852&name=label1datamaxfda366.jpg)
![Lamotrigine Tablet [Bryant Ranch Prepack]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=63726971-3809-0dc3-8502-d89095dc8401&name=label1datamaxfda360.jpg)
![Lamotrigine Tablet, Extended Release [Wockhardt Usa Llc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=0e9b23d9-0813-4fb5-848d-776453f361f7&name=lamotrigineertablets-figure-04.jpg)
![Lamotrigine Tablet, Extended Release [Wockhardt Limited]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=d3a8267b-979f-431d-baba-4ad3c5aa05e4&name=lamotrigineertabs-m-figure-04.jpg)
![Lamotrigine Tablet Lamotrigine Kit [Upsher-smith Laboratories, Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=b5e88a0b-5504-4a69-8c72-02311c70e9c9&name=lamotrigine-06.jpg)
![Lamotrigine (Lamotrigine) Tablet [Bryant Ranch Prepack]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=d33c4293-347c-49a1-9d98-f291c3dab6da&name=46971.jpg)
![Lamotrigine Tablet [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=fcaab1cd-c3a8-4c70-ad0f-7edf6cda119d&name=MM2.jpg)
![Lamotrigine Tablet [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=c3c8d9d3-b448-4cb3-a7cc-b8e6381fd460&name=MM6.jpg)
![Lamotrigine Tablet [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=e777329d-ac92-43b0-8f27-604d40057b40&name=MM2.jpg)
![Lamotrigine Tablet [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=b11a78ec-26e5-4153-8f13-ddacf91e0514&name=MM2.jpg)
![Lamotrigine Tablet [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=c879a87d-758e-45eb-9359-66a056f8342a&name=MM2.jpg)
![Lamotrigine Tablet [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=3e5149aa-c566-4d75-916d-08eeb809262d&name=MM2.jpg)
![Lamotrigine (Lamotrigine) Tablet [Avkare, Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=23a0ec98-f528-4b1a-bf1c-006f7fd100b7&name=SprayLabel.jpg)
![Lamotrigine (Lamotrigine ) Tablet [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=387c4270-2fd7-466b-8b7b-3ed35f5daa31&name=MM8.jpg)
![Lamotrigine Tablet [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=7c14101a-5553-4acf-a853-d11652a66d9a&name=MM2.jpg)
![Lamotrigine (Lamotrigine ) Tablet [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=22167b92-da4a-4b6d-aceb-04dacd0afcd3&name=MM10.jpg)
![Lamotrigine (Lamotrigine ) Tablet [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=fc093dc4-015b-40a6-9aa8-e75dd1fd6122&name=MM8.jpg)
![Lamotrigine (Lamotrigine ) Tablet [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=94848587-ab3e-42b1-959b-4f78da4caad0&name=MM8.jpg)
![Lamotrigine Tablet [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=5ab17771-0bf3-455e-9b08-4b7e205fe5fd&name=MM2.jpg)
![Lamotrigine Tablet [Mckesson Contract Packaging]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=5ac43f18-ae9f-40b8-b1e3-4d6e5b867150&name=2c979c14-8820-4101-8ecd-f6efb2dddcc7-02.jpg)
![Lamotrigine Tablet [Clinical Solutions Wholesale]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=3bf01120-bf91-4d77-9500-9870bf331c47&name=Lamo150Lab00.jpg)
![Lamotrigine Tablet [Ascend Laboratories, Llc]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=70cd448a-2921-4c69-bdf2-5a6ce883bd07&name=lamo-100mg.jpg)
![Lamotrigine Tablet, Chewable [Cobalt Laboratories]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=25bbfc59-b566-1f01-8b30-b03fa3906069&name=lamotrigine-chewable-tablets-7.jpg)
![Lamotrigine Tablet, Chewable [American Health Packaging]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=780fc63a-6aaf-4b27-a053-c593f3838dd4&name=fc158f5c-4e60-44b8-adba-fbcbc6e734ec-06.jpg)
![Lamotrigine Tablet [Physicians Total Care, Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=6c925a5d-e154-475c-8478-ab7a271d68b9&name=5921.jpg)
![Lamotrigine Tablet [Aidarex Pharmaceuticals Llc]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=6d3f37b6-ad2e-470e-be6a-3de98479a941&name=lamotrigine-100mg-tab-for-unichem-4.jpg)
![Lamotrigine Tablet [Aidarex Pharmaceuticals Llc]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=235c107d-24f7-4bf3-ac3a-3918ac1da88f&name=lamotrigine-25mg-200mg-tab-for-jubilant-cadista-2.jpg)
![Lamotrigine Tablet [Preferred Pharmaceuticals, Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=7f62f47d-4347-4a2b-a5c8-5495b57a7d97&name=0501592b-f7bf-4b0e-bae1-89ddc3ad8fc1-02.jpg)
![Lamotrigine Tablet, Chewable [Taro Pharmaceuticals U.s.a., Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=0aad8c43-6a19-4420-8987-97a3d95c52cf&name=43063423.jpg)
![Lamotrigine (Lamotrigine ) Tablet Lamotrigine (Lamotrigine) Kit [Torrent Pharmaceuticals Limited]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=3448839b-4933-4ef9-a80a-9e504d2c5696&name=lamotrigine-tab-08.jpg)
![Lamotrigine Tablet, Chewable [Glenmark Generics Inc., Usa]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=50fcf452-2d21-493e-a1dd-0c6ea9ac6184&name=25mg-bottle.jpg)
![Lamotrigine Tablet [Taro Pharmaceuticals U.s.a., Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=b829f9b2-f0ac-408a-a6f4-18b72150227d&name=lamotrigine-08.jpg)
![Lamotrigine Tablet, Film Coated, Extended Release [Wilshire Pharmaceuticals, Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=92955094-5466-4f1c-b00d-71b27353f088&name=image-12.jpg)
![Lamotrigine Tablet [Unit Dose Services]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=d3fe5f79-89c6-4947-b0d9-9c2afef1b8f7&name=50436-3996.jpg)
![Lamotrigine Tablet [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=0dcb5bfd-f21b-4efd-bfc6-174681fe9a06&name=MM4.jpg)
![Lamotrigine Tablet [Mckesson Packaging Sevices A Business Unit Of Mckesson Corporation]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=f9ff0b60-e406-4998-8c0e-42f18f7af411&name=5bb31c31-86f9-4ef6-8b94-d6d778079561-04.jpg)
![Lamotrigine (Lamotrigine) Tablet [Bryant Ranch Prepack]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=a8a5b330-0158-00b7-195e-6234292653cf&name=41831.jpg)
![Lamotrigine (Lamotrigine) Tablet [Upsher-smith Laboratories, Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=88f7a5b7-f6d5-4512-898a-4eff302a712e&name=old-spice-01.jpg)
![Lamotrigine Tablet [Mylan Institutional Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=3960b810-f239-4ee0-a82f-fc79d6856199&name=image-01.jpg)
![Lamotrigine Tablet [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=2a7ffb2a-2db7-4a19-b58c-8bae33dd349b&name=MM4.jpg)
![Lamotrigine Tablet Lamotrigine Tablet, Chewable [Zydus Pharmaceuticals (Usa) Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=81589b41-e480-4575-a84b-2b012a6ad1c3&name=pancrelipase-1.jpg)
![Lamotrigine Tablet [Aurobindo Pharma Limited]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=a9a4309e-fe43-4a26-a30f-c6577d650336&name=lamotrigine-fig2.jpg)
![Lamotrigine Tablet, Chewable [Aurobindo Pharma Limited]](https://www.recallguide.org/wp-content/themes/bootstrap/assets/img/drug-image-placeholder.jpg)
![Lamotrigine Tablet [Apotex Corp]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=c3658bc8-1524-43db-930e-66f9ac01b808&name=c3658bc8-1524-43db-930e-66f9ac01b808-02.jpg)
![Lamotrigine Tablet [Cardinal Health]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=c961f0f2-9217-404c-b94a-1ee9ce1dbb49&name=image-01.jpg)
![Lamotrigine Tablet, Chewable [Carilion Materials Management]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=a7455849-968d-4d85-8733-1e01701d7942&name=68151-4249.jpg)
![Lamotrigine Tablet, Chewable [Teva Pharmaceuticals Usa Inc]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=0db9d532-d62c-46c5-b4b9-855d78d01314&name=carvedilol-tablets---zydus-4.jpg)
![Lamotrigine Tablet [Teva Pharmaceuticals Usa Inc]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=14799df4-c425-4946-9168-9028c1f2e571&name=image-02.jpg)
![Lamotrigine Tablet [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=62918b2d-d51c-41fd-9b86-e622ba29fde1&name=MM4.jpg)
![Lamotrigine (Lamotrigine) Tablet [Jubilant Cadista Pharmaceuticals, Inc.]](http://www.recallguide.org/wp-content/themes/bootstrap/assets/img/drug-image-placeholder.jpg)
![Lamotrigine Tablet [Mylan Pharmaceuticals Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=173bb299-f774-e888-0ecf-7520ac220d78&name=image-06.jpg)
![Lamotrigine Tablet, Extended Release [Torrent Pharmaceuticals Limited]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=52df02a7-83da-4b20-9951-69790237dc24&name=lamoxrtablets-figure-07.jpg)
![Lamotrigine Tablet [Cipla Limited]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=efe2f519-4ac3-489c-ba5e-edb475cf5f2a&name=34ea3cb5-fac4-4d2b-ac5f-4455141fea3c-01.jpg)
![Lamotrigine Tablet [Tya Pharmaceuticals]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=05405214-6215-432a-aa53-f7e03f35c7b1&name=64725-0111.jpg)
![Lamotrigine Tablet [American Health Packaging]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=442aed6e-6242-4a96-90aa-d988b62d55e8&name=omnipaque-03.jpg)
![Lamotrigine Tablet [Northstar Rxllc]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=dbe07049-223d-4e54-b1ab-5b57bb9ad8ae&name=lamotrigine-100mg.jpg)
![Lamotrigine Tablet [Cardinal Health]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=26404e50-011e-4068-9745-647d2de681a3&name=image-02.jpg)