FDA records indicate that there are no current recalls for this drug.
Are you a medical professional?
Trending Topics
Sandimmune Recall
Get an alert when a recall is issued.
Questions & Answers
Side Effects & Adverse Reactions
Kidney, Liver, and Heart Transplant
(See BOXED WARNING): Sandimmune (cyclosporine), when used in high doses, can cause hepatotoxicity and nephrotoxicity.
Nephrotoxicity
It is not unusual for serum creatinine and BUN levels to be elevated during Sandimmune (cyclosporine) therapy. These elevations in renal transplant patients do not necessarily indicate rejection, and each patient must be fully evaluated before dosage adjustment is initiated.
Nephrotoxicity has been noted in 25% of cases of renal transplantation, 38% of cases of cardiac transplantation, and 37% of cases of liver transplantation. Mild nephrotoxicity was generally noted 2 to 3 months after transplant and consisted of an arrest in the fall of the preoperative elevations of BUN and creatinine at a range of 35 to 45 mg/dl and 2.0 to 2.5 mg/dl, respectively. These elevations were often responsive to dosage reduction.
More overt nephrotoxicity was seen early after transplantation and was characterized by a rapidly rising BUN and creatinine. Since these events are similar to rejection episodes, care must be taken to differentiate between them. This form of nephrotoxicity is usually responsive to Sandimmune (cyclosporine) dosage reduction.
Although specific diagnostic criteria which reliably differentiate renal graft rejection from drug toxicity have not been found, a number of parameters have been significantly associated to one or the other. It should be noted however, that up to 20% of patients may have simultaneous nephrotoxicity and rejection.
| Nephrotoxicity vs. Rejection | ||
| Parameter | Nephrotoxicity | Rejection |
| History | Donor > 50 years old or hypotensive | Antidonor immune response |
| Prolonged kidney preservation | Retransplant patient | |
| Prolonged anastomosis time | ||
| Concomitant nephrotoxic drugs | ||
| Clinical | Often > 6 weeks postopb | Often < 4 weeks postopb |
| Prolonged initial nonfunction (acute tubular necrosis) |
Fever > 37.5°C | |
| Weight gain > 0.5 kg | ||
| Graft swelling and tenderness | ||
| Decrease in daily urine volume > 500 mL (or 50%) | ||
| Laboratory | CyA serum trough level > 200 ng/mL | CyA serum trough level < 150 ng/mL |
| Gradual rise in Cr (< 0.15 mg/dL/day)a | Rapid rise in Cr (> 0.3 mg/dL/day)a | |
| Cr plateau < 25% above baseline | Cr > 25% above baseline | |
| BUN/Cr ≥ 20 | BUN/Cr < 20 | |
| Biopsy | Arteriolopathy (medial hypertrophya, hyalinosis, nodular deposits, intimal thickening, endothelial vacuolization, progressive scarring) |
Endovasculitisc (proliferationa, intimal arteritisb, necrosis, sclerosis) |
| Tubular atrophy, isometric vacuolization, isolated calcifications |
Tubulitis with RBCb and WBCb casts, some irregular vacuolization |
|
| Minimal edema | Interstitial edemac and hemorrhageb | |
| Mild focal infiltratesc | Diffuse moderate to severe mononuclear infiltratesd | |
| Diffuse interstitial fibrosis, often striped form |
Glomerulitis (mononuclear cells)c | |
| Aspiration Cytology | CyA deposits in tubular and endothelial cells |
Inflammatory infiltrate with mononuclear phagocytes, macrophages, lymphoblastoid cells, and activated T-cells |
| Fine isometric vacuolization of tubular cells |
These strongly express HLA-DR antigens | |
| Urine Cytology | Tubular cells with vacuolization and granularization |
Degenerative tubular cells, plasma cells, and lymphocyturia > 20% of sediment |
| Manometry | Intracapsular pressure < 40 mm Hgb | Intracapsular pressure > 40 mm Hgb |
| Ultrasonography | Unchanged graft cross-sectional area | Increase in graft cross-sectional area |
| AP diameter ≥ Transverse diameter | ||
| Magnetic Resonance Imagery |
Normal appearance | Loss of distinct corticomedullary junction, swelling, image intensity of parachyma approaching that of psoas, loss of hilar fat |
| Radionuclide Scan | Normal or generally decreased perfusion | Patchy arterial flow |
| Decrease in tubular function | Decrease in perfusion > decrease in tubular function | |
| (131 I-hippuran) > decrease in perfusion (99m Tc DTPA) |
Increased uptake of Indium 111 labeled platelets or Tc-99m in colloid |
|
| Therapy | Responds to decreased Sandimmune (cyclosporine) |
Responds to increased steroids or antilymphocyte globulin |
ap <0.05, bp <0.01, cp <0.001, dp <0.0001
A form of chronic progressive cyclosporine-associated nephrotoxicity is characterized by serial deterioration in renal function and morphologic changes in the kidneys. From 5% to 15% of transplant recipients will fail to show a reduction in a rising serum creatinine despite a decrease or discontinuation of cyclosporine therapy. Renal biopsies from these patients will demonstrate an interstitial fibrosis with tubular atrophy. In addition, toxic tubulopathy, peritubular capillary congestion, arteriolopathy, and a striped form of interstitial fibrosis with tubular atrophy may be present. Though none of these morphologic changes is entirely specific, a histologic diagnosis of chronic progressive cyclosporine-associated nephrotoxicity requires evidence of these.
When considering the development of chronic nephrotoxicity it is noteworthy that several authors have reported an association between the appearance of interstitial fibrosis and higher cumulative doses or persistently high circulating trough concentrations of cyclosporine. This is particularly true during the first 6 posttransplant months when the dosage tends to be highest and when, in kidney recipients, the organ appears to be most vulnerable to the toxic effects of cyclosporine. Among other contributing factors to the development of interstitial fibrosis in these patients must be included, prolonged perfusion time, warm ischemia time, as well as episodes of acute toxicity, and acute and chronic rejection. The reversibility of interstitial fibrosis and its correlation to renal function have not yet been determined.
Impaired renal function at any time requires close monitoring, and frequent dosage adjustment may be indicated. In patients with persistent high elevations of BUN and creatinine who are unresponsive to dosage adjustments, consideration should be given to switching to other immunosuppressive therapy. In the event of severe and unremitting rejection, it is preferable to allow the kidney transplant to be rejected and removed rather than increase the Sandimmune (cyclosporine) dosage to a very high level in an attempt to reverse the rejection.
Due to the potential for additive or synergistic impairment of renal function, caution should be exercised when coadministering Sandimmune with other drugs that may impair renal function. (See PRECAUTIONS, Drug Interactions)
Thrombotic Microangiopathy
Occasionally patients have developed a syndrome of thrombocytopenia and microangiopathic hemolytic anemia which may result in graft failure. The vasculopathy can occur in the absence of rejection and is accompanied by avid platelet consumption within the graft as demonstrated by Indium 111 labeled platelet studies. Neither the pathogenesis nor the management of this syndrome is clear. Though resolution has occurred after reduction or discontinuation of Sandimmune (cyclosporine) and 1) administration of streptokinase and heparin or 2) plasmapheresis, this appears to depend upon early detection with Indium 111 labeled platelet scans. (See ADVERSE REACTIONS)
Hyperkalemia
Significant hyperkalemia (sometimes associated with hyperchloremic metabolic acidosis) and hyperuricemia have been seen occasionally in individual patients.
Hepatotoxicity
Cases of hepatotoxicity and liver injury including cholestasis, jaundice, hepatitis, and liver failure have been reported in patients treated with cyclosporine. Most reports included patients with significant co-morbidities, underlying conditions and other confounding factors including infectious complications and comedications with hepatotoxic potential. In some cases, mainly in transplant patients, fatal outcomes have been reported (See ADVERSE REACTIONS, Postmarketing Experience)
Hepatotoxicity, usually manifested by elevations in hepatic enzymes and bilirubin, was reported in patients treated with cyclosporine in clinical trials: 4% in renal transplantation, 7% in cardiac transplantation, and 4% in liver transplantation. This was usually noted during the first month of therapy when high doses of Sandimmune (cyclosporine) were used. The chemistry elevations usually decreased with a reduction in dosage.
Malignancies
As in patients receiving other immunosuppressants, those patients receiving Sandimmune (cyclosporine) are at increased risk for development of lymphomas and other malignancies, particularly those of the skin. The increased risk appears related to the intensity and duration of immunosuppression rather than to the use of specific agents. Because of the danger of oversuppression of the immune system, which can also increase susceptibility to infection, Sandimmune (cyclosporine) should not be administered with other immunosuppressive agents except adrenal corticosteroids. The efficacy and safety of cyclosporine in combination with other immunosuppressive agents have not been determined. Some malignancies may be fatal. Transplant patients receiving cyclosporine are at increased risk for serious infection with fatal outcome.
Serious Infections
Patients receiving immunosuppressants, including Sandimmune, are at increased risk of developing bacterial, viral, fungal, and protozoal infections, including opportunistic infections. These infections may lead to serious, including fatal, outcomes (See BOXED WARNING, and ADVERSE REACTIONS).
Polyoma Virus Infections
Patients receiving immunosuppressants, including Sandimmune, are at increased risk for opportunistic infections, including polyoma virus infections. Polyoma virus infections in transplant patients may have serious, and sometimes, fatal outcomes. These include cases of JC virus-associated progressive multifocal leukoencephalopathy (PML), and polyoma virus-associated nephropathy (PVAN), especially due to BK virus infection, which have been observed in patients receiving cyclosporine.
PVAN is associated with serious outcomes, including deteriorating renal function and renal graft loss, (See ADVERSE REACTIONS/Postmarketing Experience). Patient monitoring may help detect patients at risk for PVAN.
Cases of PML have been reported in patients treated with Sandimmune. PML, which is sometimes fatal, commonly presents with hemiparesis, apathy, confusion, cognitive deficiencies and ataxia. Risk factors for PML include treatment with immunosuppressant therapies and impairment of immune function. In immunosuppressed patients, physicians should consider PML in the differential diagnosis in patients reporting neurological symptoms and consultation with a neurologist should be considered as clinically indicated.
Consideration should be given to reducing the total immunosuppression in transplant patients who develop PML or PVAN. However, reduced immunosuppression may place the graft at risk.
Neurotoxicity
There have been reports of convulsions in adult and pediatric patients receiving cyclosporine, particularly in combination with high-dose methylprednisolone.
Encephalopathy, including Posterior Reversible Encephalopathy Syndrome (PRES), has been described both in postmarketing reports and in the literature. Manifestations include impaired consciousness, convulsions, visual disturbances (including blindness), loss of motor function, movement disorders and psychiatric disturbances. In many cases, changes in the white matter have been detected using imaging techniques and pathologic specimens. Predisposing factors such as hypertension, hypomagnesemia, hypocholesterolemia, high-dose corticosteroids, high cyclosporine blood concentrations, and graft-versus-host disease have been noted in many but not all of the reported cases. The changes in most cases have been reversible upon discontinuation of cyclosporine, and in some cases, improvement was noted after reduction of dose. It appears that patients receiving liver transplant are more susceptible to encephalopathy than those receiving kidney transplant. Another rare manifestation of cyclosporine-induced neurotoxicity is optic disc edema including papilloedema, with possible visual impairment, secondary to benign intracranial hypertension.
Specific Excipients
Anaphylactic Reactions
Rarely (approximately 1 in 1000), patients receiving Sandimmune Injection (cyclosporine injection, USP) have experienced anaphylactic reactions. Although the exact cause of these reactions is unknown, it is believed to be due to the Cremophor EL (polyoxyethylated castor oil) used as the vehicle for the intravenous (IV) formulation. These reactions can consist of flushing of the face and upper thorax, and noncardiogenic pulmonary edema, with acute respiratory distress, dyspnea, wheezing, blood pressure changes, and tachycardia. One patient died after respiratory arrest and aspiration pneumonia. In some cases, the reaction subsided after the infusion was stopped.
Patients receiving Sandimmune Injection (cyclosporine injection, USP) should be under continuous observation for at least the first 30 minutes following the start of the infusion and at frequent intervals thereafter. If anaphylaxis occurs, the infusion should be stopped. An aqueous solution of epinephrine 1:1000 should be available at the bedside as well as a source of oxygen.
Anaphylactic reactions have not been reported with the soft gelatin capsules or oral solution which lack Cremophor EL (polyoxyethylated castor oil). In fact, patients experiencing anaphylactic reactions have been treated subsequently with the soft gelatin capsules or oral solution without incident.
Alcohol (ethanol)
The alcohol content (See DESCRIPTION) of Sandimmune should be taken into account when given to patients in whom alcohol intake should be avoided or minimized, e.g. pregnant or breastfeeding women, in patients presenting with liver disease or epilepsy, in alcoholic patients, or pediatric patients. For an adult weighing 70 kg, the maximum daily oral dose would deliver about 1 gram of alcohol which is approximately 6% of the amount of alcohol contained in a standard drink. The daily intravenous dose would deliver approximately 15% of the amount of alcohol contained in a standard drink.
Care should be taken in using Sandimmune (cyclosporine) with nephrotoxic drugs. (See PRECAUTIONS)
Conversion from Neoral to Sandimmune
Because Sandimmune (cyclosporine) is not bioequivalent to Neoral, conversion from Neoral to Sandimmune (cyclosporine) using a 1:1 ratio (mg/kg/day) may result in a lower cyclosporine blood concentration. Conversion from Neoral to Sandimmune (cyclosporine) should be made with increased blood concentration monitoring to avoid the potential of underdosing.
Legal Issues
There is currently no legal information available for this drug.
FDA Safety Alerts
There are currently no FDA safety alerts available for this drug.
Manufacturer Warnings
There is currently no manufacturer warning information available for this drug.
FDA Labeling Changes
There are currently no FDA labeling changes available for this drug.
Uses
Sandimmune (cyclosporine) is indicated for the prophylaxis of organ rejection in kidney, liver, and heart allogeneic transplants. It is always to be used with adrenal corticosteroids. The drug may also be used in the treatment of chronic rejection in patients previously treated with other immunosuppressive agents.
Because of the risk of anaphylaxis, Sandimmune Injection (cyclosporine injection, USP) should be reserved for patients who are unable to take the soft gelatin capsules or oral solution.
History
There is currently no drug history available for this drug.
Other Information
Cyclosporine, the active principle in Sandimmune (cyclosporine) is a cyclic polypeptide immunosuppressant agent consisting of 11 amino acids. It is produced as a metabolite by the fungus species Beauveria nivea.
Chemically, cyclosporine is designated as [R-[R*,R*-(E)]]-cyclic(L-alanyl-D-alanyl-N-methyl-L-leucyl-N-methyl-L-leucyl-N-methyl-L-valyl-3-hydroxy-N,4-dimethyl-L-2-amino-6-octenoyl-L-α-amino-butyryl-N-methylglycyl-N-methyl-L-leucyl-L-valyl-N-methyl-L-leucyl).
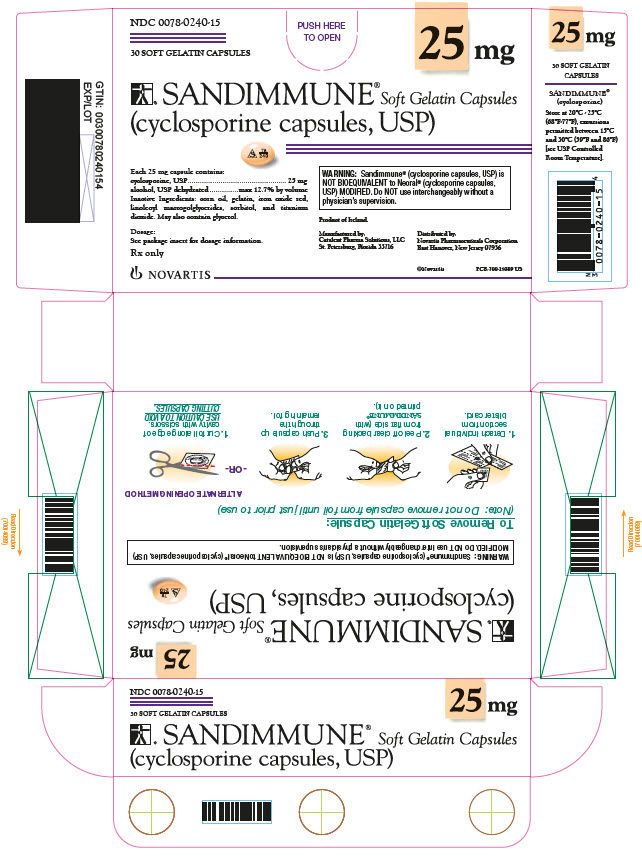
Sandimmune® Soft Gelatin Capsules (cyclosporine capsules, USP) are available in 25 mg and 100 mg strengths.
Each 25 mg capsule contains:
cyclosporine, USP…………………………………………………………………………………………25 mg
alcohol, USP dehydrated………………………………………………………………max 12.7% by volume
Each 100 mg capsule contains:
cyclosporine, USP……………………………………………………………………………………….100 mg
alcohol, USP dehydrated………………………………………………………………max 12.7% by volume
Inactive Ingredients: corn oil, gelatin, iron oxide red, linoleoyl macrogolglycerides, sorbitol, and titanium dioxide. May also contain glycerol. 100 mg capsules may contain iron oxide yellow.
Sandimmune® Oral Solution (cyclosporine oral solution, USP) is available in 50 mL bottles.
Each mL contains:
cyclosporine, USP……………………………………………………………………………………….100 mg
alcohol, Ph. Helv. ……………………………………………………………………………12.5% by volume
dissolved in an olive oil, Ph. Helv./Labrafil M 1944 CS (polyoxyethylated oleic glycerides) vehicle which must be further diluted with milk, chocolate milk, or orange juice before oral administration.
Sandimmune® Injection (cyclosporine injection, USP) is available in a 5 mL sterile ampul for intravenous (IV) administration.
Each mL contains:
cyclosporine, USP…………………………………………………………………………………………50 mg
*Cremophor® EL (polyoxyethylated castor oil)………………………………………………………..650 mg
alcohol, Ph. Helv. ……………………………………………………………………………32.9% by volume
nitrogen………………………………………………………………………………………………………….qs
which must be diluted further with 0.9% Sodium Chloride Injection or 5% Dextrose Injection before use.
The chemical structure of cyclosporine (also known as cyclosporin A) is
Sources
Sandimmune Manufacturers
-
Novartis Pharmaceuticals Corporation
![Sandimmune (Cyclosporine) Capsule, Liquid Filled Sandimmune (Cyclosporine) Injection Sandimmune (Cyclosporine) Solution [Novartis Pharmaceuticals Corporation]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sandimmune | Novartis Pharmaceuticals Corporation
![Sandimmune (Cyclosporine) Capsule, Liquid Filled Sandimmune (Cyclosporine) Injection Sandimmune (Cyclosporine) Solution [Novartis Pharmaceuticals Corporation] Sandimmune (Cyclosporine) Capsule, Liquid Filled Sandimmune (Cyclosporine) Injection Sandimmune (Cyclosporine) Solution [Novartis Pharmaceuticals Corporation]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Sandimmune Soft Gelatin Capsules (cyclosporine capsules, USP) and Sandimmune Oral Solution (cyclosporine oral solution, USP)Sandimmune Soft Gelatin Capsules (cyclosporine capsules, USP) and Sandimmune Oral Solution (cyclosporine oral solution, USP) have decreased bioavailability in comparison to Neoral Soft Gelatin Capsules (cyclosporine capsules, USP) MODIFIED and Neoral Oral Solution (cyclosporine oral solution, USP) MODIFIED. Sandimmune and Neoral are not bioequivalent and cannot be used interchangeably without physician supervision.
The initial oral dose of Sandimmune (cyclosporine) should be given 4 to 12 hours prior to transplantation as a single dose of 15 mg/kg. Although a daily single dose of 14 to 18 mg/kg was used in most clinical trials, few centers continue to use the highest dose, most favoring the lower end of the scale. There is a trend towards use of even lower initial doses for renal transplantation in the ranges of 10 to 14 mg/kg/day. The initial single daily dose is continued postoperatively for 1 to 2 weeks and then tapered by 5% per week to a maintenance dose of 5 to 10 mg/kg/day. Some centers have successfully tapered the maintenance dose to as low as 3 mg/kg/day in selected renal transplant patients without an apparent rise in rejection rate.
(See Blood Concentration Monitoring, below)
Specific Populations
Renal Impairment
Cyclosporine undergoes minimal renal elimination and its pharmacokinetics do not appear to be significantly altered in patients with end-stage renal disease who receive routine hemodialysis treatments (See CLINICAL PHARMACOLOGY). However, due to its nephrotoxic potential (See WARNINGS), careful monitoring of renal function is recommended; cyclosporine dosage should be reduced if indicated. (See WARNINGS and PRECAUTIONS)
Hepatic Impairment
The clearance of cyclosporine may be significantly reduced in severe liver disease patients (See CLINICAL PHARMACOLOGY). Dose reduction may be necessary in patients with severe liver impairment to maintain blood concentrations within the recommended target range. (See WARNINGS and PRECAUTIONS)
Pediatrics
In pediatric usage, the same dose and dosing regimen may be used as in adults although in several studies, children have required and tolerated higher doses than those used in adults.
Adjunct therapy with adrenal corticosteroids is recommended. Different tapering dosage schedules of prednisone appear to achieve similar results. A dosage schedule based on the patient’s weight started with 2.0 mg/kg/day for the first 4 days tapered to 1.0 mg/kg/day by 1 week, 0.6 mg/kg/day by 2 weeks, 0.3 mg/kg/day by 1 month, and 0.15 mg/kg/day by 2 months and thereafter as a maintenance dose. Another center started with an initial dose of 200 mg tapered by 40 mg/day until reaching 20 mg/day. After 2 months at this dose, a further reduction to 10 mg/day was made. Adjustments in dosage of prednisone must be made according to the clinical situation.
To make Sandimmune Oral Solution (cyclosporine oral solution, USP) more palatable, the oral solution may be diluted with milk, chocolate milk, or orange juice preferably at room temperature. Patients should avoid switching diluents frequently. Sandimmune Soft Gelatin Capsules and Oral Solution should be administered on a consistent schedule with regard to time of day and relation to meals.
Take the prescribed amount of Sandimmune (cyclosporine) from the container using the dosage syringe supplied after removal of the protective cover, and transfer the solution to a glass of milk, chocolate milk, or orange juice. Stir well and drink at once. Do not allow to stand before drinking. It is best to use a glass container and rinse it with more diluent to ensure that the total dose is taken. After use, replace the dosage syringe in the protective cover. Do not rinse the dosage syringe with water or other cleaning agents either before or after use. If the dosage syringe requires cleaning, it must be completely dry before resuming use. Introduction of water into the product by any means will cause variation in dose.
Sandimmune® Injection (cyclosporine injection, USP)FOR INFUSION ONLY
Note: Anaphylactic reactions have occurred with Sandimmune Injection (cyclosporine injection, USP). (See WARNINGS)
Patients unable to take Sandimmune Soft Gelatin Capsules or Oral Solution pre- or postoperatively may be treated with the intravenous (IV) concentrate. Sandimmune Injection (cyclosporine injection, USP) is administered at 1/3 the oral dose. The initial dose of Sandimmune Injection (cyclosporine injection, USP) should be given 4 to 12 hours prior to transplantation as a single intravenous dose of 5 to 6 mg/kg/day. This daily single dose is continued postoperatively until the patient can tolerate the soft gelatin capsules or oral solution. Patients should be switched to Sandimmune Soft Gelatin Capsules or Oral Solution as soon as possible after surgery. In pediatric usage, the same dose and dosing regimen may be used, although higher doses may be required.
Adjunct steroid therapy is to be used. (See aforementioned.)
Immediately before use, the intravenous concentrate should be diluted 1 mL Sandimmune Injection (cyclosporine injection, USP) in 20 mL to 100 mL 0.9% Sodium Chloride Injection or 5% Dextrose Injection and given in a slow intravenous infusion over approximately 2 to 6 hours.
Diluted infusion solutions should be discarded after 24 hours.
The Cremophor® EL (polyoxyethylated castor oil) contained in the concentrate for intravenous infusion can cause phthalate stripping from PVC.
Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
Blood Concentration MonitoringSeveral study centers have found blood concentration monitoring of cyclosporine useful in patient management. While no fixed relationships have yet been established, in one series of 375 consecutive cadaveric renal transplant recipients, dosage was adjusted to achieve specific whole blood 24-hour trough concentrations of 100 to 200 ng/mL as determined by high-pressure liquid chromatography (HPLC).
Of major importance to blood concentration analysis is the type of assay used. The above concentrations are specific to the parent cyclosporine molecule and correlate directly to the new monoclonal specific radioimmunoassays (mRIA-sp). Nonspecific assays are also available which detect the parent compound molecule and various of its metabolites. Older studies often cited concentrations using a nonspecific assay which were roughly twice those of specific assays. Assay results are not interchangeable and their use should be guided by their approved labeling. If plasma specimens are employed, concentrations will vary with the temperature at the time of separation from whole blood. Plasma concentrations may range from 1/2 to 1/5 of whole blood concentrations. Refer to individual assay labeling for complete instructions. In addition, Transplantation Proceedings (June 1990) contains position papers and a broad consensus generated at the Cyclosporine-Therapeutic Drug Monitoring conference that year. Blood concentration monitoring is not a replacement for renal function monitoring or tissue biopsies.
Login To Your Free Account