![Ziprasidone Hydrochloride (Ziprasidone Hcl) Capsule [American Health Packaging] Ziprasidone Hydrochloride (Ziprasidone Hcl) Capsule [American Health Packaging]](/wp-content/themes/bootstrap/assets/img/loading2.gif)
Duloxetine should be swallowed whole and should not be chewed or crushed, nor should the capsule be opened and its contents sprinkled on food or mixed with liquids. All of these might affect the enteric coating. Duloxetine can be given without regard to meals.
2.1 Initial Treatment
Major Depressive Disorder — Duloxetine should be administered at a total dose of 40 mg/day (given as 20 mg twice daily) to 60 mg/day (given either once daily or as 30 mg twice daily). For some patients, it may be desirable to start at 30 mg once daily for 1 week, to allow patients to adjust to the medication before increasing to 60 mg once daily. While a 120 mg/day dose was shown to be effective, there is no evidence that doses greater than 60 mg/day confer any additional benefits. The safety of doses above 120 mg/day has not been adequately evaluated [see Clinical Studies (14.1)].
Generalized Anxiety Disorder — For most patients, the recommended starting dose for duloxetine is 60 mg administered once daily. For some patients, it may be desirable to start at 30 mg once daily for 1 week, to allow patients to adjust to the medication before increasing to 60 mg once daily. While a 120 mg once daily dose was shown to be effective, there is no evidence that doses greater than 60 mg/day confer additional benefit. Nevertheless, if a decision is made to increase the dose beyond 60 mg once daily, dose increases should be in increments of 30 mg once daily. The safety of doses above 120 mg once daily has not been adequately evaluated [see Clinical Studies (14.2)].
Diabetic Peripheral Neuropathic Pain — The recommended dose for duloxetine is 60 mg administered once daily. There is no evidence that doses higher than 60 mg confer additional significant benefit and the higher dose is clearly less well tolerated [see Clinical Studies (14.3)]. For patients for whom tolerability is a concern, a lower starting dose may be considered.
Since diabetes is frequently complicated by renal disease, a lower starting dose and gradual increase in dose should be considered for patients with renal impairment [see Dosage and Administration (2.3), Use in Specific Populations (8.10), and Clinical Pharmacology (12.3)].
Fibromyalgia — The recommended dose for duloxetine is 60 mg administered once daily. Treatment should begin at 30 mg once daily for 1 week, to allow patients to adjust to the medication before increasing to 60 mg once daily. Some patients may respond to the starting dose. There is no evidence that doses greater than 60 mg/day confer additional benefit, even in patients who do not respond to a 60 mg dose, and higher doses are associated with a higher rate of adverse reactions [see Clinical Studies (14.4)].
Chronic Musculoskeletal Pain — The recommended dose for duloxetine is 60 mg once daily. Dosing may be started at 30 mg for one week, to allow patients to adjust to the medication before increasing to 60 mg once daily. There is no evidence that higher doses confer additional benefit, even in patients who do not respond to a 60 mg dose, and higher doses are associated with a higher rate of adverse reactions [see Clinical Studies (14.5)].
2.2 Maintenance/Continuation/Extended Treatment
Major Depressive Disorder — It is generally agreed that acute episodes of major depression require several months or longer of sustained pharmacologic therapy. Maintenance of efficacy in MDD was demonstrated with duloxetine as monotherapy. Duloxetine should be administered at a total dose of 60 mg once daily. Patients should be periodically reassessed to determine the need for maintenance treatment and the appropriate dose for such treatment [see Clinical Studies (14.1)].
Generalized Anxiety Disorder — It is generally agreed that episodes of generalized anxiety disorder require several months or longer of sustained pharmacological therapy. Maintenance of efficacy in GAD was demonstrated with duloxetine as monotherapy. Duloxetine should be administered in a dose range of 60-120 mg once daily. Patients should be periodically reassessed to determine the continued need for maintenance treatment and the appropriate dose for such treatment [see Clinical Studies (14.2)].
Diabetic Peripheral Neuropathic Pain — As the progression of diabetic peripheral neuropathy is highly variable and management of pain is empirical, the effectiveness of duloxetine must be assessed individually. Efficacy beyond 12 weeks has not been systematically studied in placebo-controlled trials.
Fibromyalgia — Fibromyalgia is recognized as a chronic condition. The efficacy of duloxetine in the management of fibromyalgia has been demonstrated in placebo-controlled studies up to 3 months. The efficacy of duloxetine was not demonstrated in longer studies; however, continued treatment should be based on individual patient response.
Chronic Musculoskeletal Pain — The efficacy of duloxetine has not been established in placebo-controlled studies beyond 13 weeks.
2.3 Dosing in Special Populations
Hepatic Insufficiency — It is recommended that duloxetine should ordinarily not be administered to patients with any hepatic insufficiency [see Warnings and Precautions (5.13) and Use in Specific Populations (8.9)].
Severe Renal Impairment —Duloxetine is not recommended for patients with end-stage renal disease or severe renal impairment (estimated creatinine clearance <30 mL/min) [see Warnings and Precautions (5.13) and Use in Specific Populations (8.10)].
Elderly Patients — No dose adjustment is recommended for elderly patients on the basis of age. As with any drug, caution should be exercised in treating the elderly. When individualizing the dosage in elderly patients, extra care should be taken when increasing the dose [see Use in Specific Populations (8.5)].
Pregnant Women — There are no adequate and well-controlled studies in pregnant women; therefore, duloxetine should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus [see Use in Specific Populations (8.1)].
Lilly maintains a pregnancy registry to monitor the pregnancy outcomes of women exposed to duloxetine while pregnant. Healthcare providers are encouraged to register any patient who is exposed to duloxetine during pregnancy by calling the Cymbalta Pregnancy Registry at 1-866-814-6975 or by visiting www.cymbaltapregnancyregistry.com
Nursing Mothers — Because the safety of duloxetine in infants is not known, nursing while on duloxetine is not recommended [see Use in Specific Populations (8.3)].
2.4 Discontinuing Duloxetine
Symptoms associated with discontinuation of duloxetine and other SSRIs and SNRIs have been reported. A gradual reduction in the dose rather than abrupt cessation is recommended whenever possible [see Warnings and Precautions (5.7)].
2.5 Switching a Patient To or From a Monoamine Oxidase Inhibitor (MAOI) Intended to Treat Psychiatric Disorders
At least 14 days should elapse between discontinuation of an MAOI intended to treat psychiatric disorders and initiation of therapy with duloxetine. Conversely, at least 5 days should be allowed after stopping duloxetine before starting an MAOI intended to treat psychiatric disorders [see Contraindications (4.1)].
2.6 Use of Duloxetine with Other MAOIs such as Linezolid or Methylene Blue
Do not start duloxetine in a patient who is being treated with linezolid or intravenous methylene blue because there is an increased risk of serotonin syndrome. In a patient who requires more urgent treatment of a psychiatric condition, other interventions, including hospitalization, should be considered [see Contraindications (4.1)].
In some cases, a patient already receiving duloxetine therapy may require urgent treatment with linezolid or intravenous methylene blue. If acceptable alternatives to linezolid or intravenous methylene blue treatment are not available and the potential benefits of linezolid or intravenous methylene blue treatment are judged to outweigh the risks of serotonin syndrome in a particular patient, duloxetine should be stopped promptly, and linezolid or intravenous methylene blue can be administered. The patient should be monitored for symptoms of serotonin syndrome for 5 days or until 24 hours after the last dose of linezolid or intravenous methylene blue, whichever comes first. Therapy with duloxetine may be resumed 24 hours after the last dose of linezolid or intravenous methylene blue [see Warnings and Precautions (5.4)].
The risk of administering methylene blue by non-intravenous routes (such as oral tablets or by local injection) or in intravenous doses much lower than 1 mg/kg with duloxetine is unclear. The clinician should, nevertheless, be aware of the possibility of emergent symptoms of serotonin syndrome with such use [see Warnings and Precautions (5.4)].

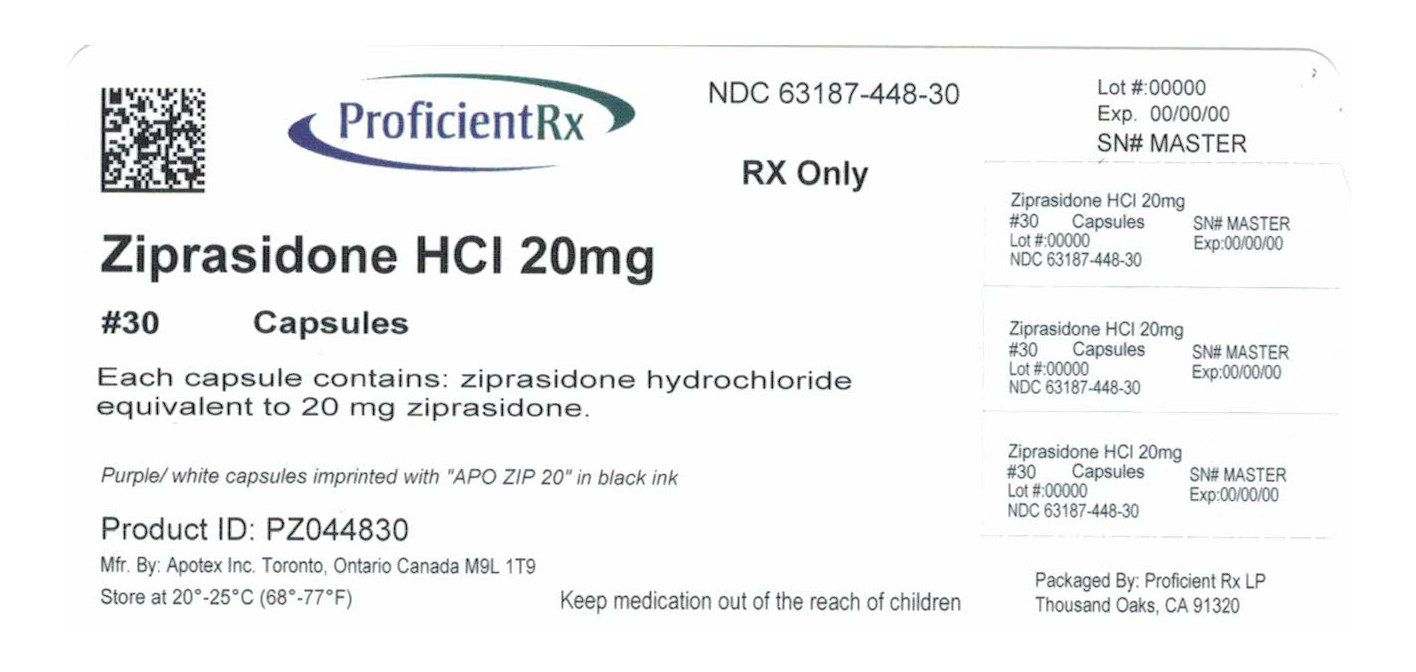

![Ziprasidone Hydrochloride Capsule [Proficient Rx Lp]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=bc0a2047-5e3b-45e6-98bc-1e404c859d96&name=terbinafine-02.jpg)
![Ziprasidone Hydrochloride (Ziprasidone Hcl) Capsule [American Health Packaging]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=bb15bd15-b27e-4814-b4cf-7636f25c0792&name=duloxetine-20mg-contain-60-5700.jpg)
![Ziprasidone Hydrochloride Capsule [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=f368e4c2-25a9-453f-a96f-e35636b5670a&name=MM2.jpg)
![Ziprasidone Hydrochloride Capsule [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=02199d0e-0eef-4126-8f58-6eac9f06e80b&name=MM2.jpg)
![Ziprasidone Hydrochloride (Ziprasidone Hcl) Capsule [Golden State Medical Supply, Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=b1f52226-4fb4-48bf-8bfd-0c9df6ca02fa&name=LabelGraphic-Ziprasidone20mg60s.jpg)
![Ziprasidone Hydrochloride Capsule [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=99bcde9b-81db-4b04-b2a6-c779f80ec05e&name=MM2.jpg)
![Ziprasidone Hydrochloride Capsule [Major Pharmaceuticals]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=ca55c149-5b9a-4144-b586-37cb5e84dc4e&name=ziprasidone-hydrochloride-capsules-2.jpg)
![Ziprasidone Hydrochloride Capsule [Rebel Distributors Corp]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=6f63fe2d-fe55-473f-99cd-9c8eb97e562b&name=6f63fe2d-fe55-473f-99cd-9c8eb97e562b-02.jpg)
![Ziprasidone Hydrochloride Capsule [Wockhardt Usa Llc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=7850be55-aeec-42e9-992d-5467b22cf2d9&name=ziprasidonecapsules-figure-02.jpg)
![Ziprasidone Hydrochloride Capsule [Wockhardt Limited]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=81ca60c4-376b-43b7-b050-09e328fc403c&name=ziprasidoncapsules-m-figure-02.jpg)
![Ziprasidone Hydrochloride Capsule [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=f9196d56-6f1e-4bb3-b233-22d17aef10b4&name=MM2.jpg)
![Ziprasidone Hydrochloride Capsule [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=6f985781-0ff8-4551-b8d5-72960b984794&name=MM2.jpg)
![Ziprasidone Hydrochloride Capsule [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=0da8c62a-bcd5-493b-ad6f-2acfb972e960&name=MM2.jpg)
![Ziprasidone Hydrochloride Capsule [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=c79dfacb-4e63-4d1b-875a-4a1340d48f7f&name=MM3.jpg)
![Ziprasidone Hydrochloride Capsule [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=ca146c7a-10aa-4a4f-89e9-534a36edbd08&name=MM2.jpg)
![Ziprasidone Hydrochloride Capsule [Unit Dose Services]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=79cb0abf-e80f-4c28-a3f9-a962efa5fdbd&name=rspl50436-0331.jpg)
![Ziprasidone Hydrochloride Capsule [American Health Packaging]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=ff43707b-0faa-4492-8102-bc288a576e3a&name=1ee99454-fcea-4c72-a75b-497263135bd9-01.jpg)
![Ziprasidone Hydrochloride Capsule [Cardinal Health]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=a1205cde-9534-43a9-914e-ac4e75a78b0d&name=a1205cde-9534-43a9-914e-ac4e75a78b0d-01.jpg)
![Ziprasidone Hydrochloride Capsule [Dr. Reddy’s Laboratories Limited]](http://www.recallguide.org/wp-content/themes/recallguide/assets/img/drug-image-placeholder.jpg)
![Ziprasidone Hydrochloride Capsule [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=8e243447-d4f1-4853-847f-b1e4a0e27732&name=MM2.jpg)
![Ziprasidone Hydrochloride Capsule [Sandoz Inc]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=0607a7bf-1833-41f0-99e3-b8ce87fa26f8&name=image-01.jpg)
![Ziprasidone Hydrochloride Capsule [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=fda8b339-9be2-496e-a4fe-0045df09e49d&name=MM2.jpg)
![Ziprasidone Hydrochloride Capsule [Cardinal Health]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=0090b65d-d663-4588-b0e6-e6fc903ca18c&name=b6625089-0629-4f6e-8164-0b582c56d475-02.jpg)
![Ziprasidone Hydrochloride Capsule [Mylan Pharmaceuticals Inc.]](https://www.recallguide.org/wp-content/themes/bootstrap/assets/img/drug-image-placeholder.jpg)
![Ziprasidone Hydrochloride Capsule [Bluepoint Laboratories]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=14811f3a-f053-49b2-a296-e592973135c6&name=14811f3a-f053-49b2-a296-e592973135c6-02.jpg)
![Ziprasidone Hydrochloride Capsule [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=500a2ff3-4c11-4c7a-b9bf-ecabc89f643c&name=MM2.jpg)
![Ziprasidone Hydrochloride (Ziprasidone Hcl) Capsule [Clinical Solutions Wholesale]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=37d443cc-385c-44a3-aca2-6053b50ad5e9&name=37d443cc-385c-44a3-aca2-6053b50ad5e9-02.jpg)
![Ziprasidone Hydrochloride Capsule [Remedyrepack Inc. ]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=0fb14e11-18bb-48b5-9b44-b3247f899c74&name=MM2.jpg)
![Ziprasidone Hydrochloride (Ziprasidone Hcl) Capsule [Apotex Corp.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=d2253f76-d451-4eea-bb16-0607054a7e94&name=RubbingAlcohol_70pct_Unscented_16oz.jpg)
![Ziprasidone Hydrochloride Capsule [Tya Pharmaceuticals]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=4890cf77-8da3-46ae-b6f6-abea7aae6b4d&name=64725-0993.jpg)
![Ziprasidone Hydrochloride Capsule [Tya Pharmaceuticals]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=5752ef72-c515-4ead-a359-69d4761ad7f4&name=64725-2164.jpg)
![Ziprasidone Hydrochloride Capsule [Tya Pharmaceuticals]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=e05f08d9-682b-4113-bfa1-d0e351e30fa1&name=64725-0259.jpg)
![Ziprasidone Hydrochloride Capsule [Mylan Institutional Inc.]](http://dailymed.nlm.nih.gov/dailymed/image.cfm?setid=07513379-6025-41e3-9d0c-d0a48a73b3ae&name=image-01.jpg)